I put together the following post about boosters for 5-11 year olds yesterday afternoon. Shortly thereafter, 19 kids in this age bracket died during a mass shooting in Texas. It suddenly felt silly to send. Our kids need boosters but also much, much more. They need to come home after school. They need their community to advocate for their safety. They need to live long, prosperous lives. Enough is enough. We can and need to change this insanity. As a mom, researcher, and neighbor, I will do all in my power to change this. I hope you will join me.
For those looking for immediate resources, the National Child Traumatic Stress Network developed the following to help children, families, educators, and communities navigate what they are seeing and hearing, acknowledge their feelings, and find ways to cope together. These resources include:
Helping Youth After a Community Trauma: Tips for Educators (En Español)
Coping After Mass Violence: For Adults.
Last week, in the middle of monkeypox news, the CDC ACIP met to discuss a COVID-19 booster for 5-11 year olds. Here were the presentations and the agenda. Ultimately, CDC strongly recommended dose 3 for 5-11 year olds, five months after dose 2. Since then, I have received many, many questions. Here is my best attempt to answer them.
Get your kid vaccinated.
Before I go into boosters, only 28% of 5-11 year olds have received the primary series to date. This is abysmally low. The vaccine works, is safe, and is needed for children. During the Omicron wave, 87% of hospitalized children were unvaccinated. Even though infection-induced immunity is high among children after Omicron, it’s not 100%. And, even so, there are three big reasons why I wouldn’t rely on this protection (read more here). Occurrence of long COVID19 is also higher among adolescents compared to younger kids, and risk is reduced with vaccination. And, in general, being sick for a week or two is just not fun (for mom, dad, or kid). Go get your kid vaccinated.
Why do children need a booster?
Data suggests that this was always a three-dose series, we just didn’t know it at the beginning of the vaccine roll-out. The two-dose series is sub-optimal against infection because Omicron is particularly good at escaping neutralizing antibodies—our first line of defense. Among 5-11 year olds, two-dose vaccine effectiveness against infection ranges from 30-40%. Unfortunately, protection also wanes more quickly against Omicron compared to previous variants, like Delta. The CDC presented the graph below last week, which showed waning immunity among 5-11 year olds following the trend of adults. (Notice after two doses adults and adolescents reached ~0% effectiveness against infection after five months).
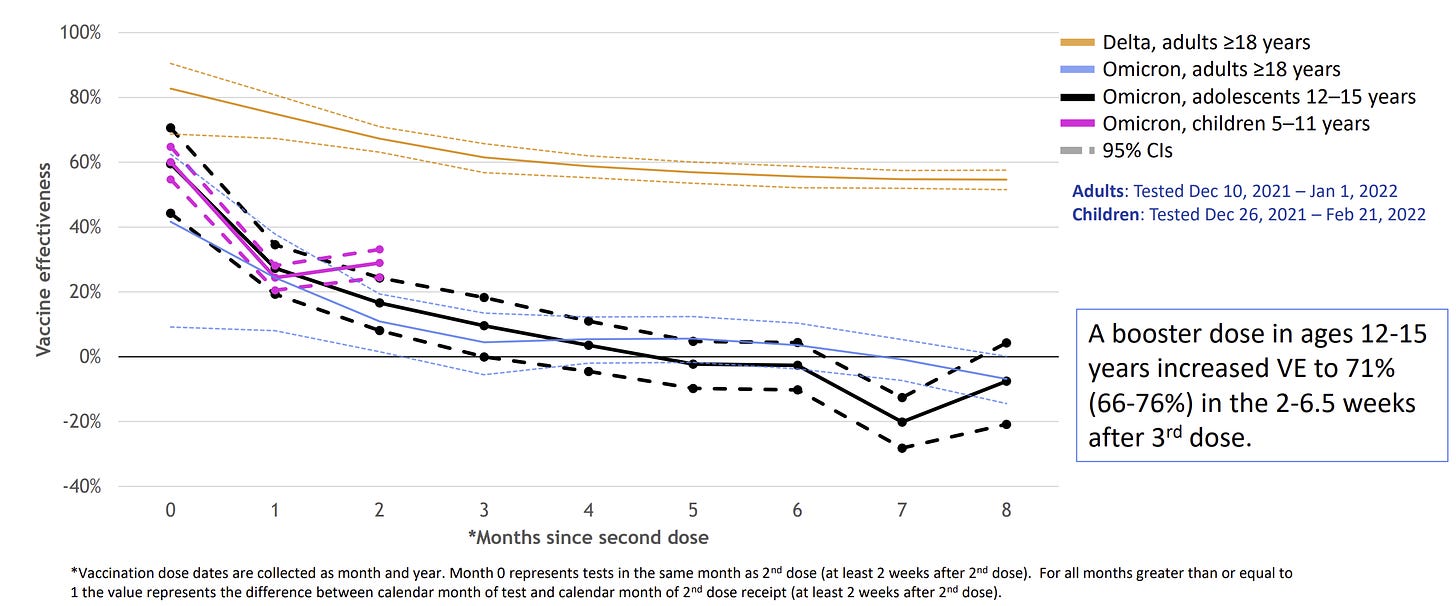
Vaccine effectiveness against severe disease is 68% among 5-11 year olds with the two-dose series. A third dose will make this higher. We don’t know if protection is waning because hospitalizations are a relatively rare event, so our confidence in the rate at which effectiveness is (or is not) waning is not strong. The data is just too noisy to have a clear picture. We do have stronger data suggesting the vaccine is slightly waning for 12-17 year olds and, theoretically, there’s no reason to believe this would be different for 5-11 year olds.
What are the side effects of a booster?
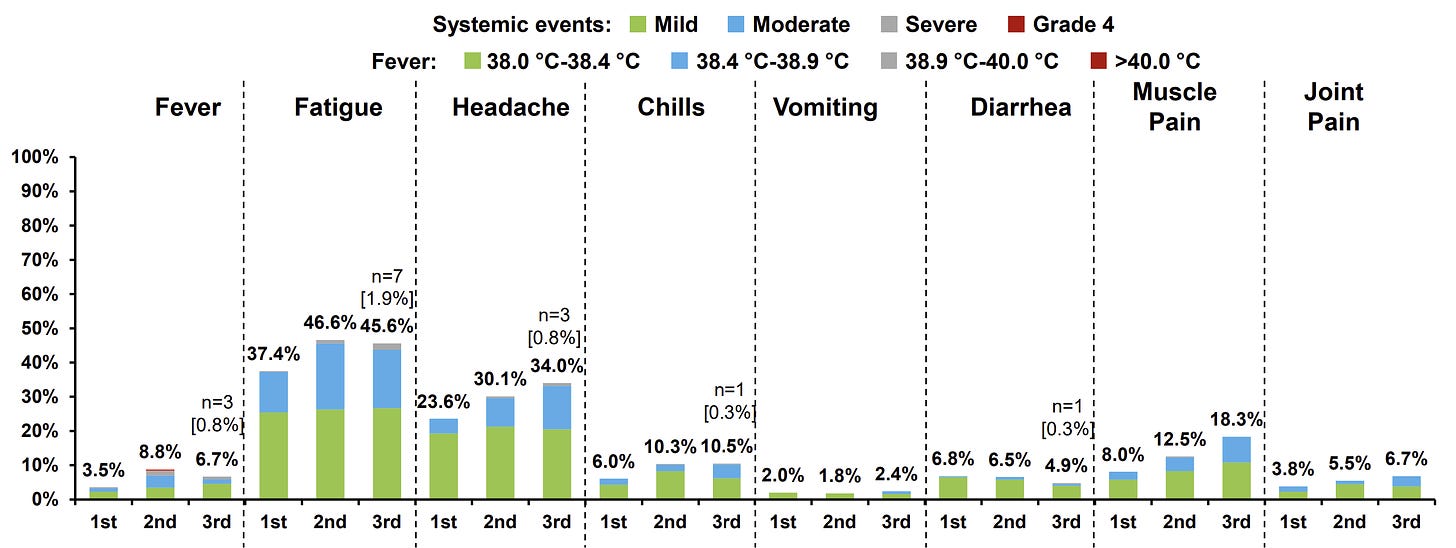
In Pfizer’s clinical trial, side effects among 5-11 year olds were about the same in dose 3 compared to dose 2. Quite a few kids will experience fatigue, headaches, and muscle pain.
Myocarditis update?
Out of 18.1 million doses administered among 5-11 year olds, 20 cases of vaccine-induced myocarditis have been reported to the CDC:
Of these, 14 occurred after dose 2; six cases occurred after dose 1.
17 out of the 20 were hospitalized. And, as of last week, 14 fully recovered.
1 death in a male child is being investigated. He had a fever 12 days after dose 1 followed by abdominal pain, vomiting, and death the next day. The autopsy confirmed myocarditis, and testing did not find evidence of a viral infection.
The estimated “background rate” of myocarditis is 0.2 to 2.2 per 1 million. So, among 5-11 year old boys, there is a slight increased risk of vaccine-induced myocarditis as shown on the slide below. It’s important to note that kids can also get myocarditis from viral infections, like SARS-CoV-2. Thankfully, vaccine-induced myocarditis continues to be far less severe than infection-induced myocarditis. We expect myocarditis rates from dose 3 to be even lower, as the 5-month period between doses allows the immune system to calm down.

Is OAS risk among kids higher?
As I have written before, scientific literature shows that original antigenic sin (OAS) is not a general concern at this time. However, a physician recently asked me a wonderful question: Is OAS more risky for kids with a booster given they have more years of life to live? This is a complex answer. Research on influenza suggests that kids make exceptionally broad responses, which would actually mean the opposite is true—OAS is a more of a theoretical risk for adults compared to kids. But, in all transparency, this is a guess in what is formally a “data free zone.” In any case, OAS isn’t insurmountable.
Given that school is starting in a few months, should we wait for a booster?
Delaying the booster and coordinating optimal timing for a vaccine is a slippery slope. I don’t have a crystal ball; no one does. What happens in the fall is unknown and can be a lifetime away during a pandemic. While there are talks of a bivalent vaccine (a vaccine with the original formula + Omicron-specific formula), that’s certainly not decided yet. Also, it’s not clear who would need this vaccine. If data shows that kids need another shot after their booster today, there’s still time for a 5-month window before Winter hits. The timing is actually pretty ideal. We are also in a surge right now and we need to be responsive to the needs of kids’ immune systems right now. And, if anything, a lot of families have fun summer trips planned, and it would be unfortunate to need to cancel because of a COVID19 infection. The way I’ve approached the pandemic vaccination schedule is to stick with what we know today. Take out the rest of the noise.
What if my child was recently infected with COVID-19?
If your child had a confirmed infection in the past 3 months, it’s not unreasonable to delay the booster. Vaccine + infection is called “hybrid immunity” and over 20 studies have shown this works fantastic due to complimentary and broad protection: Vaccine immunity targets the spike protein and infection-induced immunity targets the whole virus. This doesn’t mean you should purposefully get COVID19, but we need to recognize this as a viable path to protection.
To be clear, the FDA and CDC do not recognize hybrid immunity as an option. So, if you don’t follow the official schedule and rely on hybrid immunity, then future moves, like when to get another vaccine, may be tough to navigate. We also don’t know how long hybrid immunity will last among children. Before Omicron, evidence found that hybrid immunity worked great for at least one year. I suspect Omicron is probably negatively impacting this timeline a bit, but we haven’t seen data yet.
What about the under 5 vaccine?
For us parents with kids under 5, hearing about dose 3 for 5-11 year olds is tough because we don’t even have one vaccine yet for our littles. I’m sure you saw the news that the Pfizer 3-dose vaccine works great. The FDA solidified their schedule and will now meet June 13-14 to discuss both Moderna and Pfizer. Assuming both are approved, deciding which one to get will be challenging. I’ll be sure to provide cliff notes and thoughts next month!
Bottom line
If I had a 5-11 year old, I would get them boosted now regardless of previous infection. Maybe it’s just me, but I’m getting tired of overthinking things with this pandemic. If the decision is paralyzing, be sure to talk to their pediatrician and just know you’re already doing a great job protecting your child by getting the original series. You won’t screw it up, regardless of what you do decide about the timing for dose 3.
Love, YLE
“Your Local Epidemiologist (YLE)” is written by Dr. Katelyn Jetelina, MPH PhD—an epidemiologist, biostatistician, wife, and mom of two little girls. During the day she works at a nonpartisan health policy think tank, and at night she writes this newsletter. Her main goal is to “translate” the ever-evolving public health science so that people will be well equipped to make evidence-based decisions. This newsletter is free thanks to the generous support of fellow YLE community members. To support the effort, please subscribe here:






Can the US epidemic of mass shootings (primary targets being schools) be addressed as a public health issue problem, using some of the tools of epidemiology research?
Thank you also for your resources about responding to the school shooting. I'm putting together resources to share with my parish right now. These will be helpful.