Today, ACIP — CDC’s external scientific committee — had their normally scheduled meeting on all vaccines. YLE only stayed for the Covid-19 discussion.
Here are your Cliff notes.
Bottom line up front (BLUF)
CDC says those over 65 should get a second Covid-19 vaccine this spring. (I’m not convinced that all people over 65 need it, though.)
Who is being hospitalized by COVID-19 today?
At this winter’s peak, there were 20,000 new hospital admissions and 2,000 deaths due to Covid-19 per week. This is less than previous winters but still higher than flu. Who is being hospitalized?
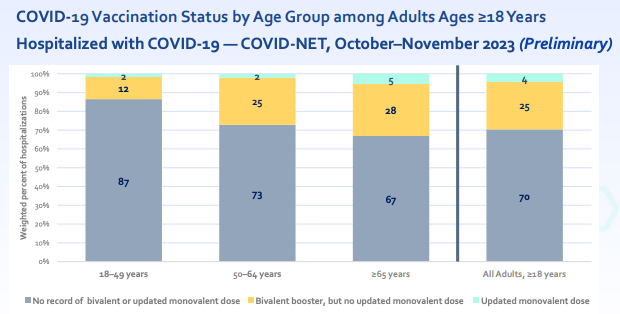
The vast majority (95% of adults) were not up-to-date on their annual Covid-19 vaccine.
16% of hospitalizations are among immunocompromised patients (higher than the general population, which is 3-6%).
About 4% of those hospitalized with Covid-19 die.
The majority of hospitalized patients had obesity, cardiovascular disease, or dementia. (However, this largely reflects the general population, and there’s no “control group” to contextualize risk.)
Why aren’t people getting Covid-19 vaccines?
Vaccine coverage is really quite terrible in the United States. CDC is conducting surveys to understand why. This is what they found:
Among those who aren’t getting the vaccine, Americans say the top concerns are: 1. Unknown side effects; 2. Not enough studies; 3. Too busy or forgetting; 4. Lack of trust; and 5. Effectiveness, including doesn’t prevent infection. Only 19% of Americans said their physician recommended the vaccine to them.
Physicians who are NOT recommending vaccinations say it’s because of: patient medical reasons, patients will refuse the vaccine, or patients are tired of hearing about Covid-19. Many primary care providers do not carry the vaccine because of low interest in or cost of the vaccine.
How effective are the fall vaccines?
Pretty great and largely comparable to flu vaccines every year.
Vaccine effectiveness (VE) against symptomatic infection: 49% additional protection compared to those who did not get a fall vaccine
VE against ED/outpatient visits: 47%
VE against hospitalization: 52%
Some other interesting nuggets:
Interestingly, there was no waning yet. (Lab studies have shown that the antibodies are more stable than previous vaccines, and we don’t know why.)
VE decreased with JN.1 (60% → 45%) but still worked okay.
Context is SO important here. There is a public perception that the vaccines are not as compelling as they wre in the pandemic's beginning. However, the comparison group has changed as collective immunity increased. Most people have been infected and/or vaccinated—nearly 100%. This means VE today is additional protection compared to all the immunity already out there.
Is a spring vaccine cost-effective?
This is a key consideration for many countries (like the U.K.), as their government provides free vaccines for all. This isn’t a main driving policy consideration in the U.S. Regardless, they found:
One dose per year: Cost-effective (in other words, the cost of purchasing a vaccine is cheaper than the cost of hospitalizations)
Two doses per year: May be cost-effective for those over 65 years, depending on how high future waves get
Other information
Timing of previous infection. Unfortunately, no data on vaccination and timing with a recent infection was presented. (I would treat previous infections like a vaccine.)
No data was presented on the effectiveness of the spring vaccine last year. We don’t have data showing the benefit of two doses a year compared to one for those over age 65.
Should vs. may. During the meeting, CDC originally proposed that people “may” get a spring vaccine. However, many external ACIP members pushed back and wanted a “should” recommendation instead. I didn’t see compelling data to suggest such a strong and confident recommendation. The benefits of two doses a year look small. Although safety risks are much smaller, there are risks of coming out too strong, especially with vaccine skeptics. CDC ultimately landed on a “should,” mainly for implementation and communication ease.
Bottom line
People hospitalized today for Covid-19 are not up-to-date on their annual vaccine, even among those over 65 years. CDC says those over 65 should get a second Covid-19 vaccine this spring. This follows Canada’s and, somewhat U.K.’s, spring Covid-19 recommendations.
I’m not convinced that most people over 65 need a spring vaccine. I will be recommending a spring vaccine to my family members in nursing homes (they are over 90 years old) or those who have multiple comorbidities, like heart disease. I don’t think they need to run to get it, but there will be a small benefit, given that we have multiple waves a year and their T cells (immune memory) are weak against Covid-19. (I think those over 65 who never got a fall vaccine should run.)
Love, YLE
P.S. ACIP will cover RSV vaccine information tomorrow. YLE will provide separate Cliff notes.
“Your Local Epidemiologist (YLE)” is written by Dr. Katelyn Jetelina, M.P.H. Ph.D.—an epidemiologist, wife, and mom of two little girls. During the day, she is a senior scientific consultant to several organizations, including CDC. At night, she writes this newsletter. Her main goal is to “translate” the ever-evolving public health world so that people will be well-equipped to make evidence-based decisions. This newsletter is free, thanks to the generous support of fellow YLE community members. To support this effort, subscribe below:






As always, YLE summaries are the best!
On clarification on "cost effective." Katelyn said correctly that the vaccines given to those 65+ annually are cost effective. However, that does not mean that the vaccines would cost less than the prevented hospitalization. That is "cost saving," a special subset of cost-effective. The ACIP reported that a single dose of COVID vaccination annually for those over age 65 was cost saving last fall, but "only" cost effective (Cost of $11K per QALY) with this Spring's evaluation.
We generally consider interventions cost effective if they cost less than $50K (or $100K or $150K) per Quality Adjusted Life Year (QALY) saved. VERY few things within medical care delivery are cost saving (traditional childhood vaccines, birth control and abortion, as well as flu shots for those over 55, palliative care and smoking cessation. But not much else!). So it's pretty amazing that the these vaccinations are cost effective - though they are not cost saving.
Again, thanks to YLE for all that you do to keep us informed!
Thanks for the cliff notes!
You had me at hello with this: "The vast majority (95% of adults) were not up-to-date on their annual Covid-19 vaccine."
Followed by that lovely chart showing only 2-5% of hospitalizations across ALL age groups had received the XBB monovalent vaccine this fall.
Another commenter astutely quoted the vaccine durability looks pretty good through 119 days, but I'm not sure we can say not waning yet, as we are now another 60+days since the end of that period.
With Covid being a systemic disease, and my primary care priority of preventing complications, increased CV risks, long Covid, and problems well beyond the most dire data points of hospitalization and death... I'll be giving the spring boost a thumbs up for my peeps.