In recent weeks, some have been quick to criticize health policy decisions in the U.S. by pointing to decisions made in other countries.
For example, the U.S. has a broad recommendation for the fall Covid-19 vaccine, while the U.K. has a more targeted policy. This conversation is bleeding into flu vaccines and Covid-19 isolation and testing policies, as similar contrasts exist.
It’s fair to wonder why. We are all high-income countries. We all have the same vaccines. We are all looking at the same data. How could public health officials come to different conclusions across countries?
One word: landscape.
The health landscape is entirely different from country to country. Because of this, we should expect country-level policy decisions to vary. How we approach health threats on a population level will be different because the threat’s implications are different.
The U.S. healthcare system is subpar.
U.S. healthcare is hard to access, has poor administrative efficiency, and lacks equity. In 2021, the Commonwealth Fund compared the healthcare systems of 11 high-income countries, using measures such as access to care, equity, and health outcomes. The U.S. had the worst healthcare system performance: an overall ranking of 11 out of 11.
This means that if someone gets sick, it’s hard to get help. And, as we’ve seen throughout the pandemic, it’s harder for certain groups than others. This means we need to do even more in the U.S. to prevent infectious diseases and their poor outcomes, including hospitalization and death, than in other high-income countries.
U.S. health insurance is mostly voluntary.
Even if someone gets to a doctor, Americans have a patchwork of coverage to pay for the costs. This differs from other high-income countries as shown below.

This means that a bigger net needs to be cast, ideally across the whole population, when it comes to providing lower-cost interventions, like a vaccine, so we can avoid people having to go to the doctor in the first place.
CDC estimates that, compared with giving the fall Covid-19 vaccine to only those aged 65 or older, universal vaccination will prevent an additional 200,000 hospitalizations and 15,000 deaths.
There are also significant differences between countries in who will buy Covid-19 vaccines this fall:
U.S.: CDC recommendations determine who pays for the vaccine. By providing universal recommendations, the following happens:
Private insurance companies and public insurers (i.e., Medicaid and Medicare) buy vaccines for all their enrollees;
The Bridge Program—a $1.1 billion new public-private partnership—will pay for uninsured adults;
It will now be included in the federally funded Vaccines for Children— a program that provides vaccines “at no cost to children who might otherwise be vaccinated because of inability to pay.”
U.K.: Has a single-payer system funded by taxation, so it decided not to pay for the vaccine for everyone, giving it instead to those at high risk of severe disease, based on cost-benefit considerations.
U.S. healthcare capacity is lower than average.
The U.S. also doesn’t have much wiggle room in hospitals. The Commonwealth Fund found the U.S. had 2.8 hospital beds per 1,000 population, lower than the OECD average of 4.3. (Notice that the U.K. also has low capacity).
In other words, we need to work harder to keep people out of the hospital so we have enough beds for non-preventable medical needs. Pre-pandemic, our hospitals would reach capacity during just a bad flu season.
The U.S. safety net is unacceptable.
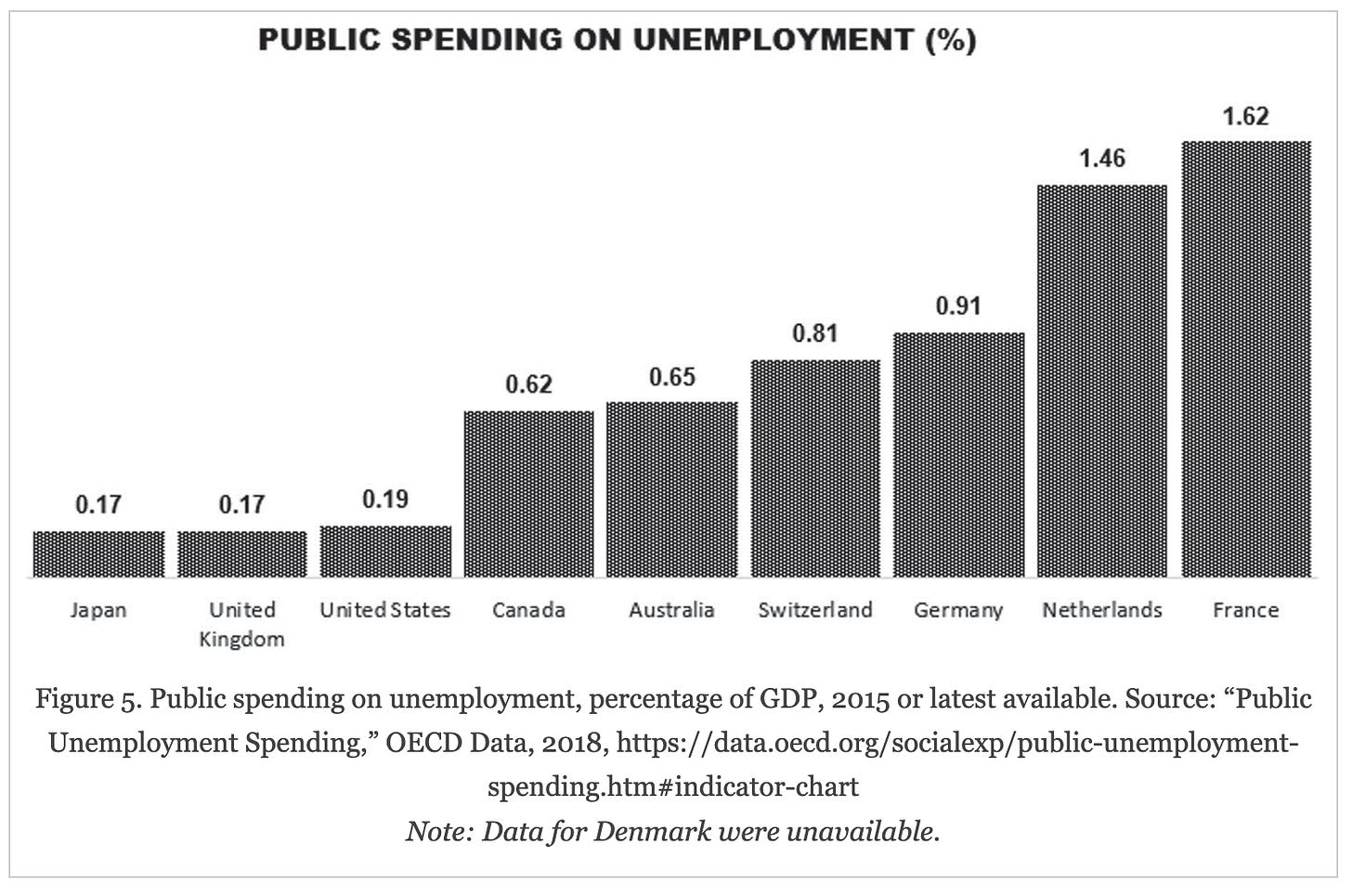
If someone gets sick in the U.S., there isn’t the same level of support as in our peer high-income nations.
For example, we don’t have federally guaranteed sick pay. This means people are more likely to go to work sick and spread viruses. The International Labor Forum summarized it nicely in several graphs.
U.S. health status is poorer.
Taken together, Americans have worse health than their counterparts. In one study, they had worse health across all 16 health outcomes than their English counterparts. This stark disparity is particularly relevant to infectious diseases like Covid-19 that exacerbate underlying health conditions.

In the decisions this fall, CDC noted that “the vast majority of the U.S. population has an underlying condition that would qualify under a risk-based recommendation.”
Bottom line
The U.S. has much less wiggle room to mess up than other countries because we have worse healthcare access, less social support, less healthcare capacity, and worse health. Casting a larger net, such as universal vaccine recommendations for Covid-19, is more necessary than in other countries.
Keep this in mind when it comes to cross-country comparisons.
Love, YLE and GY
Dr. Gavin Yamey is the Hymowitz Professor of Global Health in the Duke Global Health Institute, a Professor of Public Policy in the Duke Sanford School of Public Policy, and Director of Duke University’s Center for Policy Impact in Global Health.
“Your Local Epidemiologist (YLE)” is written by Dr. Katelyn Jetelina, M.P.H. Ph.D.—an epidemiologist, wife, and mom of two little girls. During the day, she is a senior scientific consultant to several organizations. At night, she writes this newsletter. Her main goal is to “translate” the ever-evolving public health world so that people will be well-equipped to make evidence-based decisions. This newsletter is free, thanks to the generous support of fellow YLE community members. To support this effort, subscribe below:














One of the most concise and honestly damning pieces I have seen written about the US Health care system compared to other 1st world nations.
Absolutely spot-on. Excellent documentation of some of the myriad problems our healthcare system has evolved over time. And thanks for the OECD statistics. I need to put together a lecture on this topic, and you've raised points my notes didn't cover yet. I'd not considered the number of beds per capita, obviously a sign I needed more time on the topic, but your summary is very appropriate.
Thank you.