This morning the FDA authorized boosters for everyone aged 18+. An ACIP meeting quickly followed, as all vaccine policy goes through the CDC before being rolled out. I was hoping this meeting would clarify three things:
What is the vaccine effectiveness in the United States?
Does a booster change the definition of “fully vaccinated” for mandates?
What about a booster for 12-17 year olds?
Here is the agenda. Here are the powerpoints. And, here are your cliff notes…
What is the vaccine effectiveness in the United States?
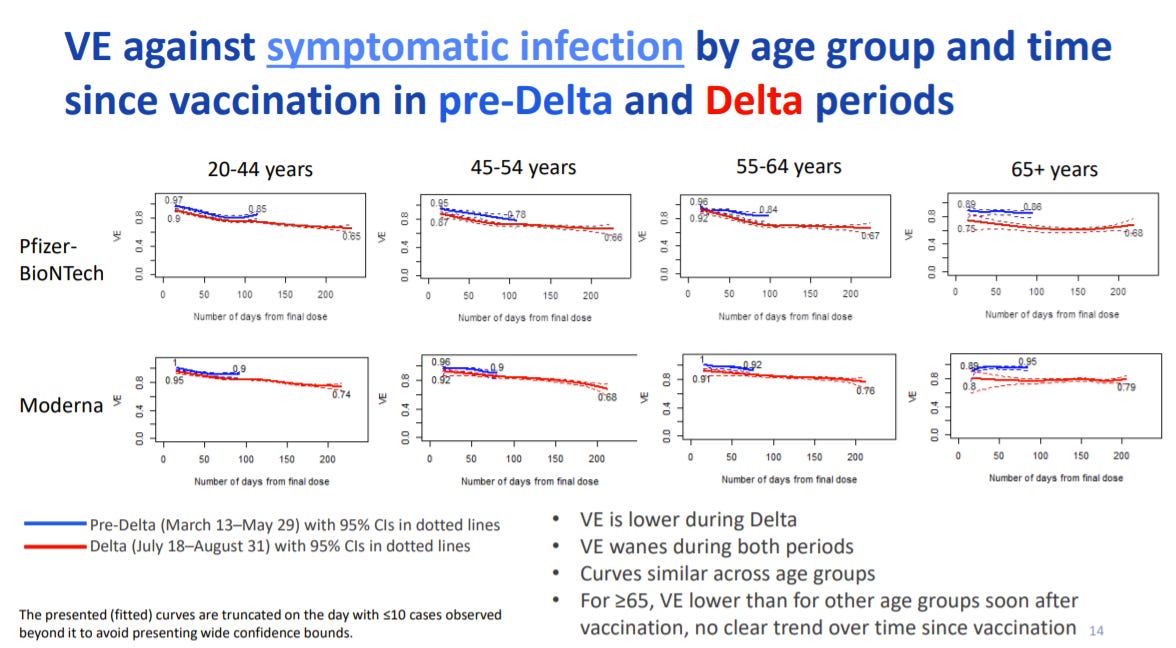
We finally got some insight on vaccine effectiveness (VE) over time in the States. The CDC pulled data from the IVY network (21 hospitals) and found that VE against any infection (mild to severe disease) is decreasing (slide below). Waning immunity is faster with Delta; It is happening in all age groups (20+ years); and is happening with both Pfizer and Moderna vaccines (although Moderna is slower).
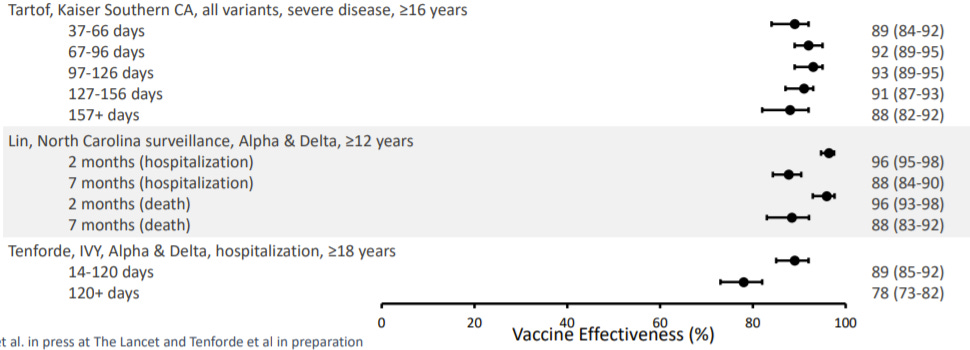
For VE against severe disease (hospitalization and death), ACIP relied on 3 studies, which all showed slightly different stories:
Kaiser study: VE against severe disease is not waning over time
North Carolina study: VE against severe disease is waning for hospitalization, but maybe not for death
IVY Data: VE against severe disease is waning for hospitalizations
So, we don’t have a clear picture. But this isn’t a surprise given all three studies were done with very different populations, done at slightly different times, and done with different statistical models. Below is a slide that summarized the studies.
And this is it. This is all the data the CDC presented today. Which is insane— the United States does not have a real-time, comprehensive picture of our vaccines, nor the number of breakthrough cases, nor who’s more likely to have a breakthrough case or not. I cannot emphasize enough of how detrimental this is to our public health response. Bad data produces (potentially) bad policy. We are flying blind. And I don’t know if we can blame the CDC. We have to blame our own inaction to fund public health infrastructures before a pandemic. Now that a pandemic is here we can only piecemeal a system together.
What else?
Other than VE, there are other factors to consider too. Specifically the benefit-risk ratio of boosters:
Benefits of a booster: Prevention of infection; Prevention of severe disease for some; Potential to reduce transmission; Ease of implementation (In mid-October, 4 out of 10 vaccinated adults were unsure if they were eligible for a booster)
Risks of a booster: Potential myocarditis. However, boosters thus far have resulted in a rate of 2 myocarditis cases per 1,000,000 doses. This matches the background rate.
Discussion/Vote
Almost all members voiced strong opinions that the main goal of these vaccines is to prevent severe disease and death. Secondary goals include infection and reduced transmission. Many members said we cannot simply prevent all infections.
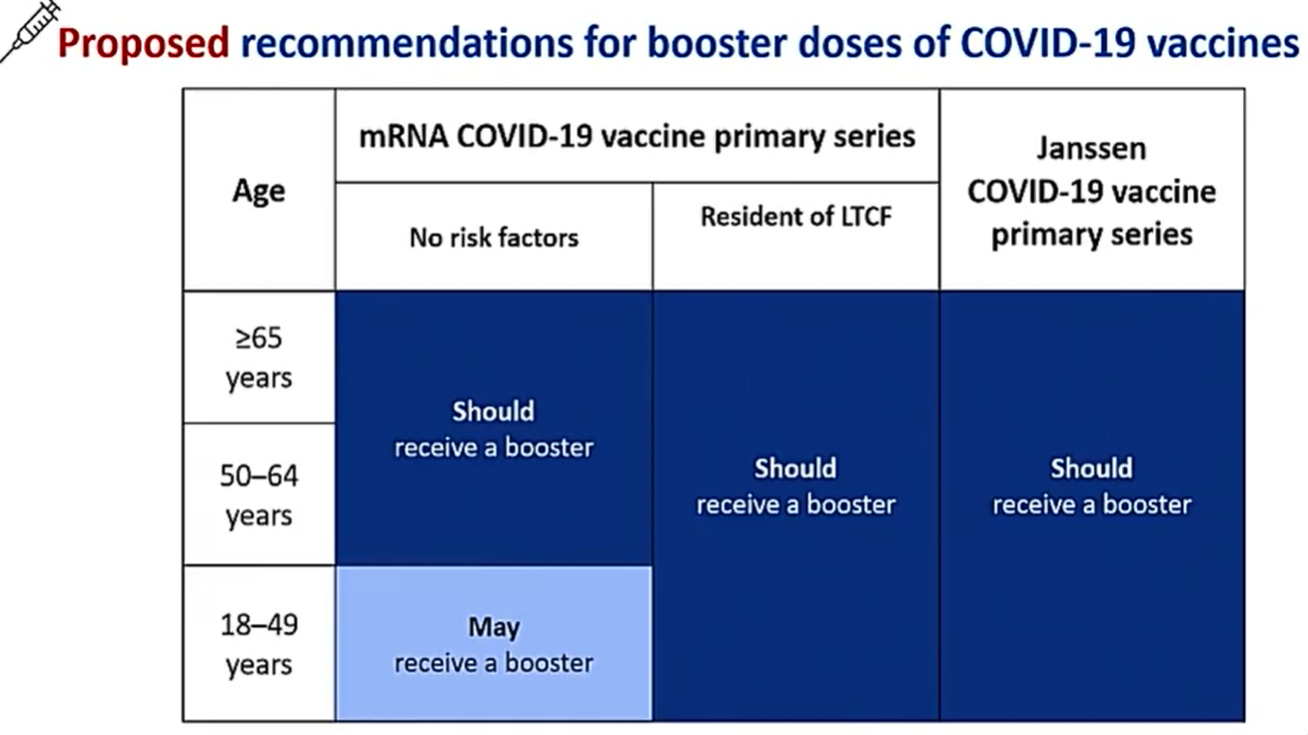
With this main goal in mind, members emphasized there is still a difference between who “should” get a booster compared to those who “may”. For example, adults aged 50+ should get a booster if they have a chronic conditions. But those younger than 50 may get a booster if they are in high exposure occupations or live with a vulnerable family member.
The ACIP members were asked to vote on the following policy:
And they unanimously voted yes.
What about 12-17 year olds?
Many parents are asking if their adolescent should get a booster because the 6 month mark is coming up soon. This ACIP meeting didn’t discuss 12-17 year olds. The FDA and CDC hasn’t provided an official explanation either. But I have an idea why...
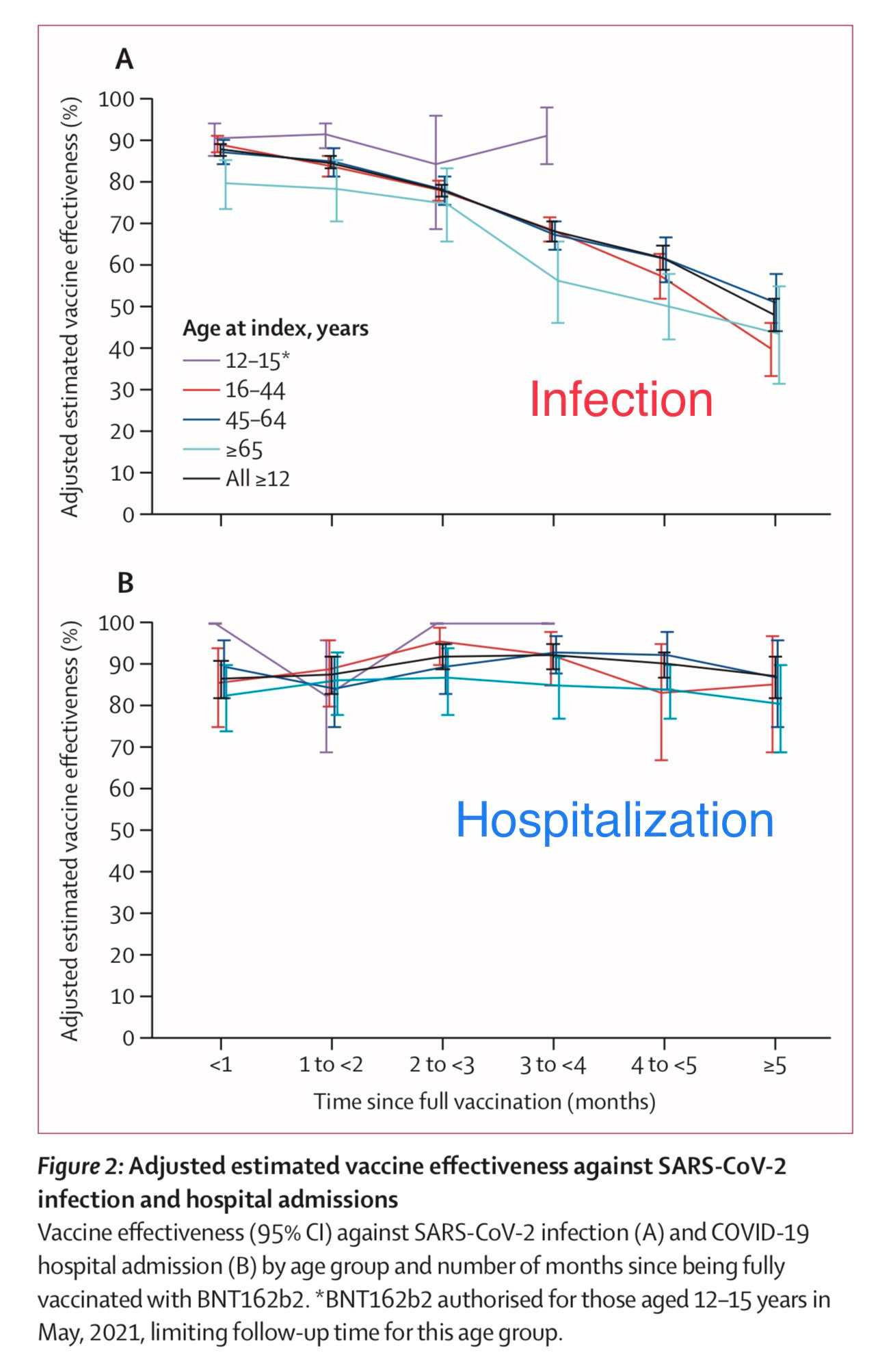
During clinical trials, 12-17 year olds had an even higher neutralizing antibody response than adults even though they were given the same dose. So, while adult antibodies are waning, the waning isn’t as urgent for adolescents. In October, we saw this phenomenon in a peer-reviewed study from the Lancet. The scientists measured VE over time for different age groups and plotted it on a graph (see below). Adolescent vaccines were not declining at the same rate as adults. Are they today? Maybe. Again, we don’t have the data.
Also, the peak for vaccine-induced myocarditis risk is at 16 years old. Regulatory agencies (FDA, CDC) are being very careful to assess whether the benefits outweigh the risks for this age group. Adolescents will likely need a booster one point. It’s just not right now.
Have a great weekend,
Katelyn
“Your Local Epidemiologist (YLE)” is written by Dr. Katelyn Jetelina, MPH PhD— an epidemiologist, biostatistician, professor, researcher, wife, and mom of two little girls. During the day she has a research lab and teaches graduate-level courses, but at night she writes this newsletter. Her main goal is to “translate” the ever-evolving public health science so that people will be well-equipped to make evidence-based decisions, rather than decisions based in fear. This newsletter is free thanks to the generous support of fellow YLE community members. To support the effort, please subscribe here:





Really interesting that there's apparently lower myocarditis risk after the third dose than after the second. A function of the 6-month dosing interval? Or just due to those who experienced it with the second dose, perhaps being predisposed, not getting the third? Worth investigating.
Thank you! So disappointed they wouldn’t even discuss 16-17 year olds. Many work in risky situations or live with high risk people. Many have had Pfizer for 8 months! Sounds like they won’t even let their doctors decide.