It’s been a few weeks since I’ve updated on COVID-19. Here’s the state of affairs.
Surveillance
SARS-CoV-2 continues to decline after a small Spring Break bump. Wastewater levels are the lowest they’ve been in over a year! Hospitalizations and deaths continue to decline as well, but we are still losing 1,300 people per week.

As expected, COVID-19 continues to mutate. Interestingly, scientists are finding that mutations not on the spike protein are becoming more and more influential in the virus’s ability to continue to spread.
XBB.1.16 (which social media has deemed “Arcturus”) has created a huge wave in India, which is finally peaking. But this isn’t necessarily what will happen elsewhere. The last wave in India was nine months ago; there were a lot of susceptible people. In the U.S., XBB.1.16 accounts for 7% of cases. If growth continues, this could create a bump in transmission in weeks to come, but we do not expect a tsunami.
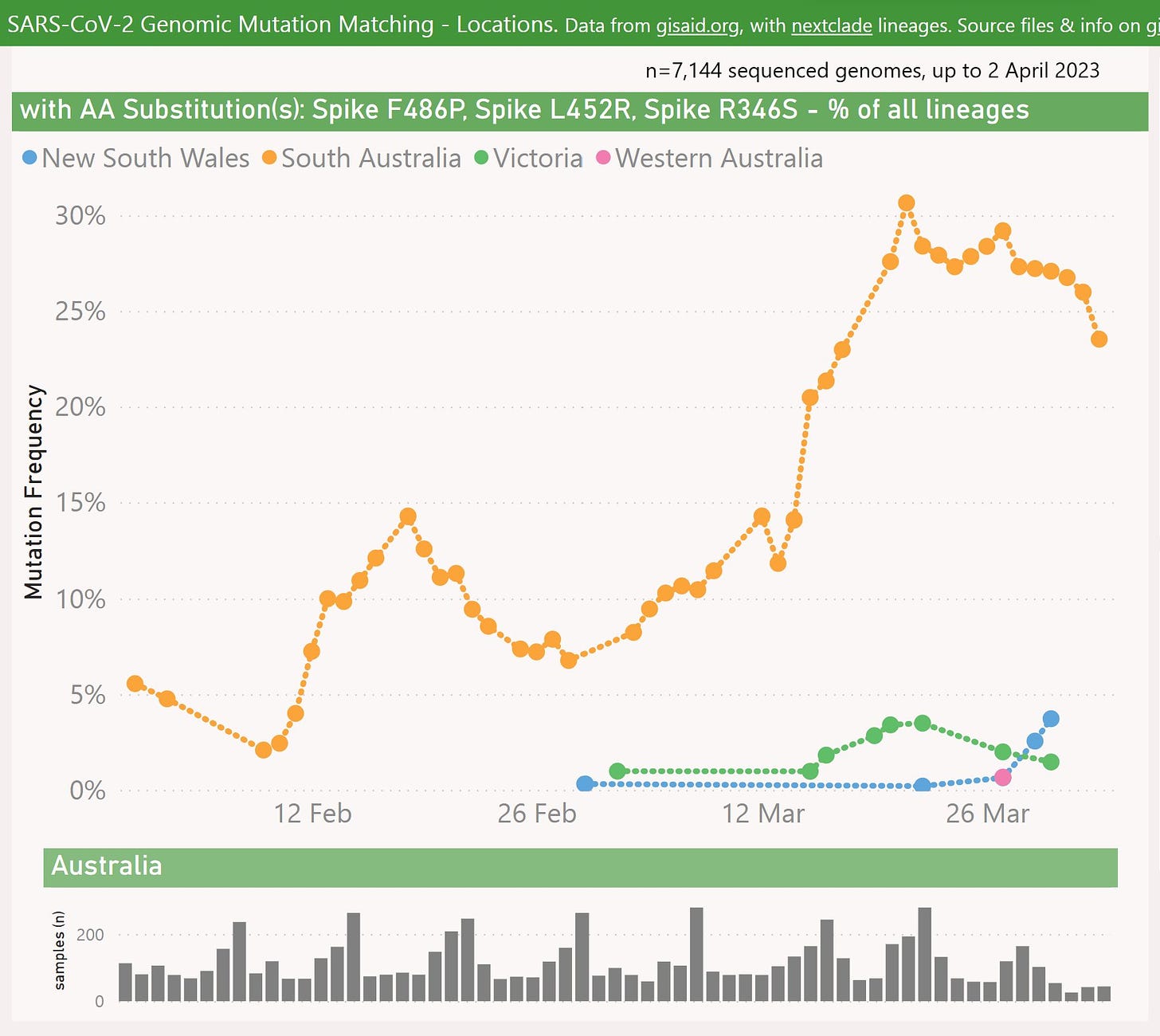
Another up-and-coming Omicron subvariant could provide competition—XBC.1.6. This is a recombination of Delta and Omicron first detected in Southern Australia. It has since caused a wave of cases and hospitalizations there. This may be also one to follow.
Noteworthy pieces of COVID-19 news
Operation Next Gen. The Biden administration announced Operation Next Gen— an allocation of $5 billion dollars to speed up the testing and development of second-generation COVID-19 vaccines and therapies. This is a much needed investment, as a pan-coronavirus or mucosal vaccine could be a game changer. Unfortunately, they are incredibly challenging to make.
Spring boosters. The FDA has been very quiet on this end. Word on the street is they’re deciding on a spring policy and a few other decisions for the future of COVID-19 vaccines (instead of waiting for fall). This would make sense given that ACIP has scheduled a meeting for tomorrow. I’ll be back with Cliff notes if anything noteworthy happens.
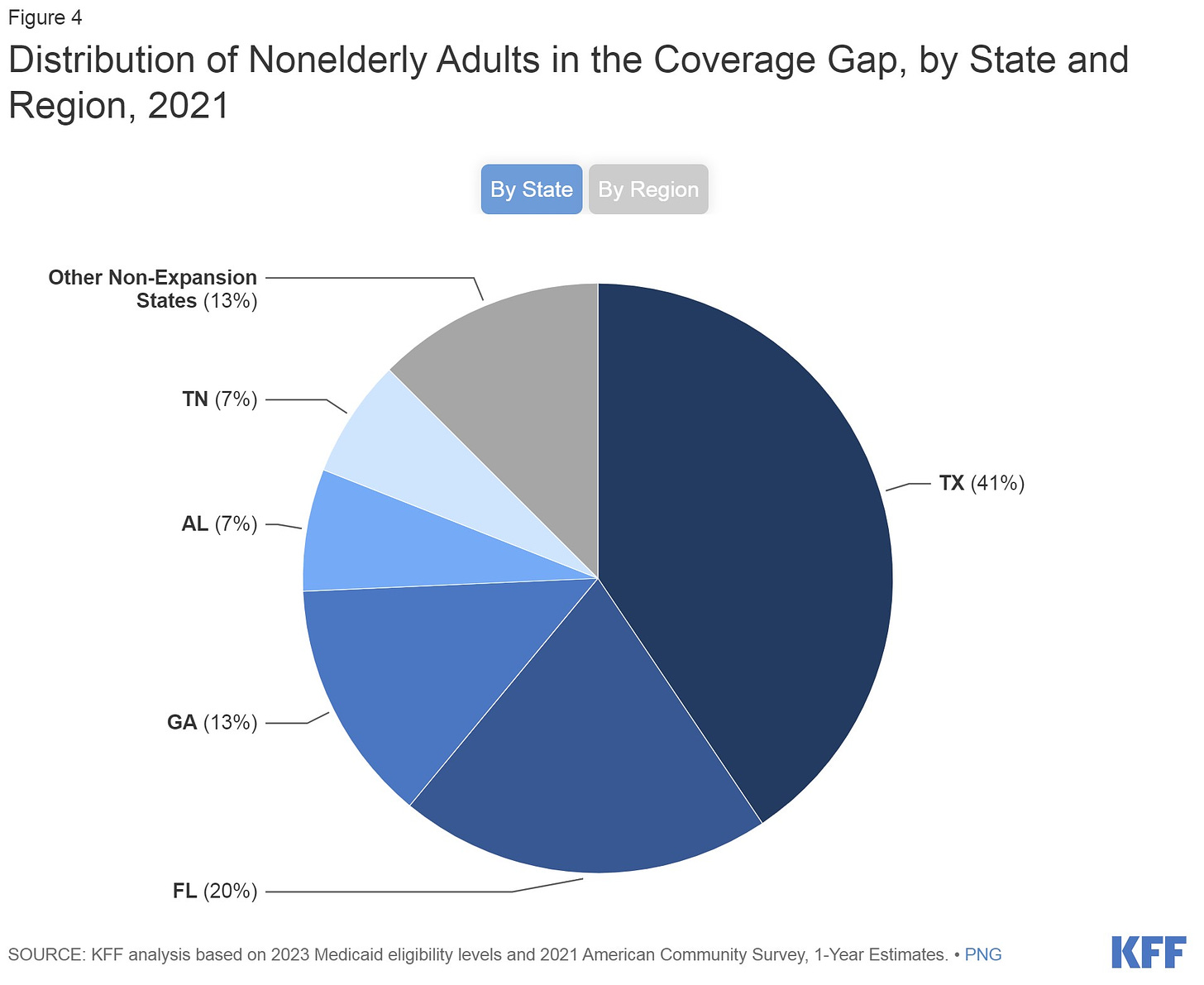
End of the emergency. The National Emergency ended last week, which was the first of five “buckets” of pandemic provisions ending. It mainly had implications for Medicaid eligibility. KFF found that adults impacted are most concentrated in Texas (41%), followed by Florida (20%), and Georgia (13%). Next month, the Public Health Emergency ends, which will mean quite a lot.
Interesting science updates
SARS-CoV-2 is mutating to escape Paxlovid. Scientists have found instances in which SARS-CoV-2 mutated to resist Paxlovid protection. These mutations have not taken off, but it’s a concerning sign. It would really hurt if we lost Paxlovid as a tool.
Where you live matters. Not all states struggled equally in the pandemic. In fact, a Lancet study found a 4-fold difference in deaths between states, even after adjusting for age and key health conditions. Arizona had the highest rate.
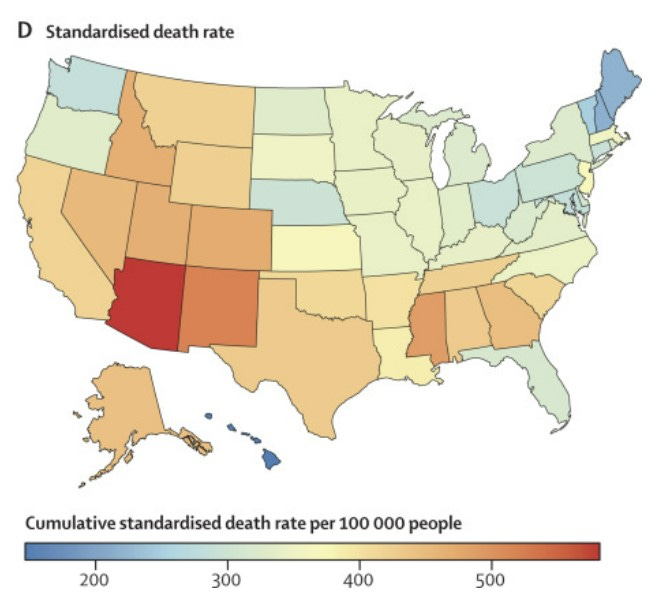
Cumulative COVID-19 infection and death rates by US state. Figure from: Bollyky et al., Lancet. Half of COVID-19 symptomatic healthcare workers went to work sick. Given that masks are dropping at hospitals, this may be a bad sign for hospital-acquired COVID-19 infections, which are increasing and already have a high mortality rate (~10.6%). (Note: This rate of going to work while sick is about the same for flu.)
U.K.’s bet on vaccine timing worked. The U.K. saved ~10,000 lives and 58,000 hospital admissions by separating doses of the primary series by 12 weeks, instead of 3 weeks. This strategy was intended to increase the reach of first doses. Despite the success, I still think it was the right move in the States to stick to the clinical trial protocol (3 weeks), given rising vaccine skepticism.
Bottom line
We are entering a lull in transmission, but COVID-19 continues to show its colors. A big shift is coming in our response as the emergency ends in the next month. Will keep you updated.
Love, YLE
“Your Local Epidemiologist (YLE)” is written by Dr. Katelyn Jetelina, MPH PhD—an epidemiologist, data scientist, wife, and mom of two little girls. During the day she works at a nonpartisan health policy think tank and is a senior scientific consultant to a number of organizations, including the CDC. At night she writes this newsletter. Her main goal is to “translate” the ever-evolving public health science so that people will be well equipped to make evidence-based decisions. This newsletter is free thanks to the generous support of fellow YLE community members. To support this effort, subscribe below.





Please do everything you can to influence ACIP on a positive decision to offer the bivalent booster to the elderly and other vulnerable folks. Thank you for all you do!
A couple of comments: Healthcare workers (as do most workers) do go to work sick. Part of this is they are casual or permanent part time without sick benefits: you don't work, you don't get paid. As a full time employee all my career (and I do realize how lucky I am), I could stay home when sick, but of course didn't always do that. If I had a sore throat but no fever, I would wear a mask when taking patient's blood as part of my role as a lab technologist...long before any pandemic came around.
Second: masks should never fully go away. After SARS in 2003, the province of Ontario developed excellent recommendations for healthcare workers when working with someone with an acute, respiratory infection (ARI), which was defined as a new or worsening cough or shortness of breath and/or fever. If a patient was entering a healthcare environment there was a sign (passive screening) and a box of masks for the patient to don if they had those symptoms. Staff would wear mask and eye protection when working with that patient. I still think anyone with respiratory signs and symptoms who must leave the house should wear a mask to limit spread to others...even if their COVID rapid test is negative: if you are symptomatic...wear a mask!