Covid-19 is now the 10th leading cause of death
And, yes, it’s still more severe than the flu.
Throughout the pandemic, many have longed to understand Covid-19 in the context of flu. It makes sense—they’re both respiratory viruses with similar symptoms transmitted in similar ways. Flu is a familiar risk—we knew where it stood in our repertoire of threats, making it a helpful comparison for calculating the risk of a novel threat.
Covid-19 is here to stay, but the risks—severe disease, death, and long covid—have declined dramatically.
So, in anticipation of the upcoming fall season, this begs the question: Is Covid-19 still more severe than the flu? Yes, but the gap is narrowing.
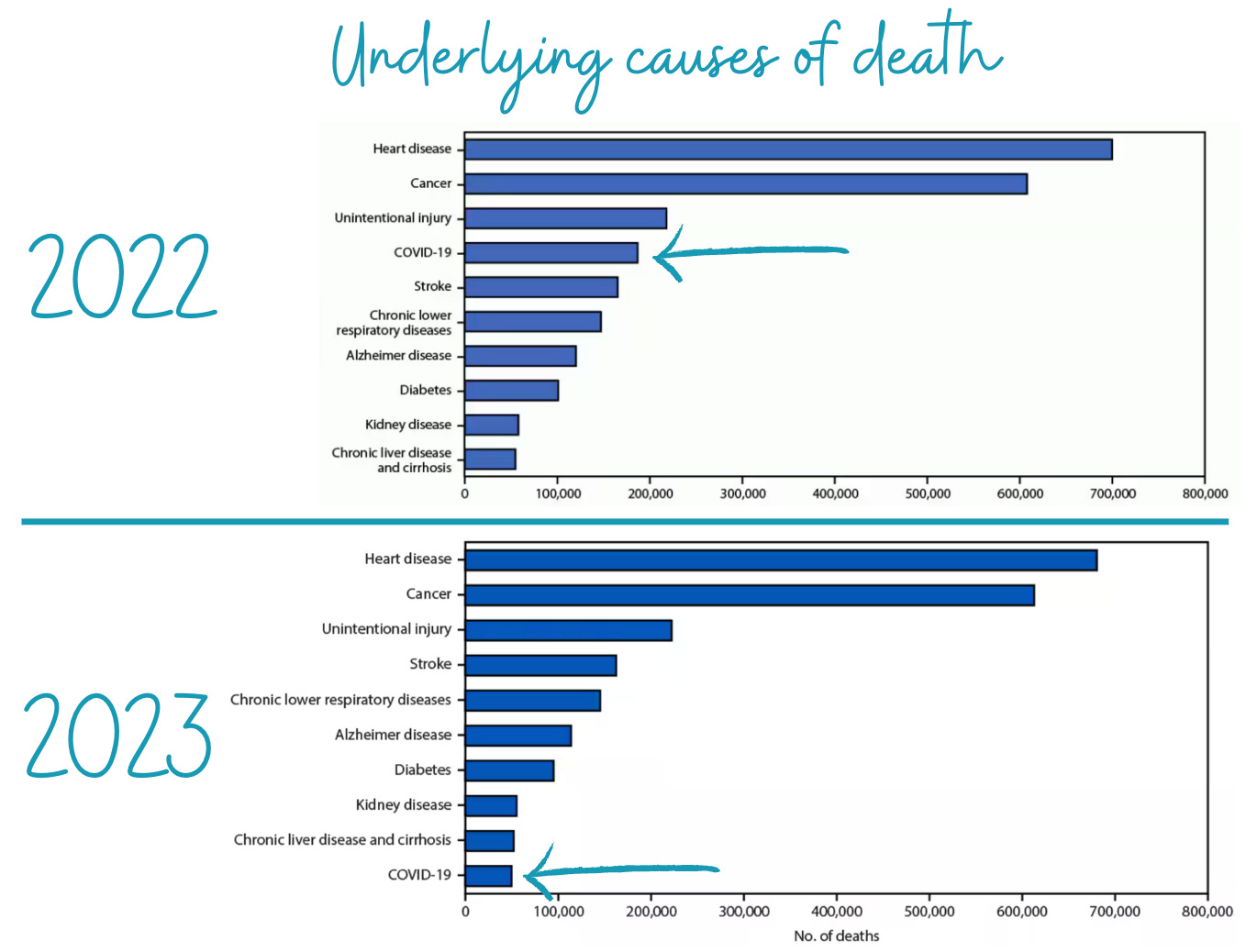
Covid-19 is now the 10th leading cause of death
Last week, CDC published 2023 provisional data on causes of death. This is basically a first draft of data—the numbers may shift with more death certificate reviews, but they typically don’t change dramatically.
What did CDC find? Last year Covid-19 plunged to the 10th leading cause of death—down from 4th in 2022 and 3rd in 2021. When looking at raw numbers, there was a nearly 70% decrease in one year! (245,614 deaths in 2022 vs. 76,446 in 2023.) We’ve come a long way.
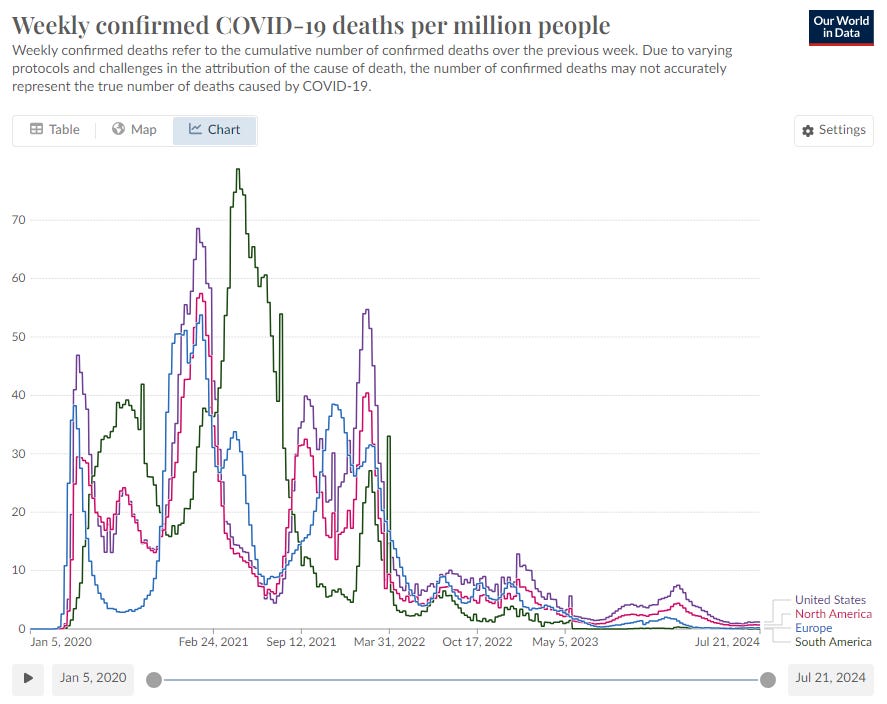
This dramatic decline in deaths wasn’t just in the U.S. We’ve seen deaths plunge across the globe thanks to immunity (from vaccination and infection) and treatments like monoclonal antibodies and antivirals.
While this is incredible news, Covid-19 is still more deadly than flu
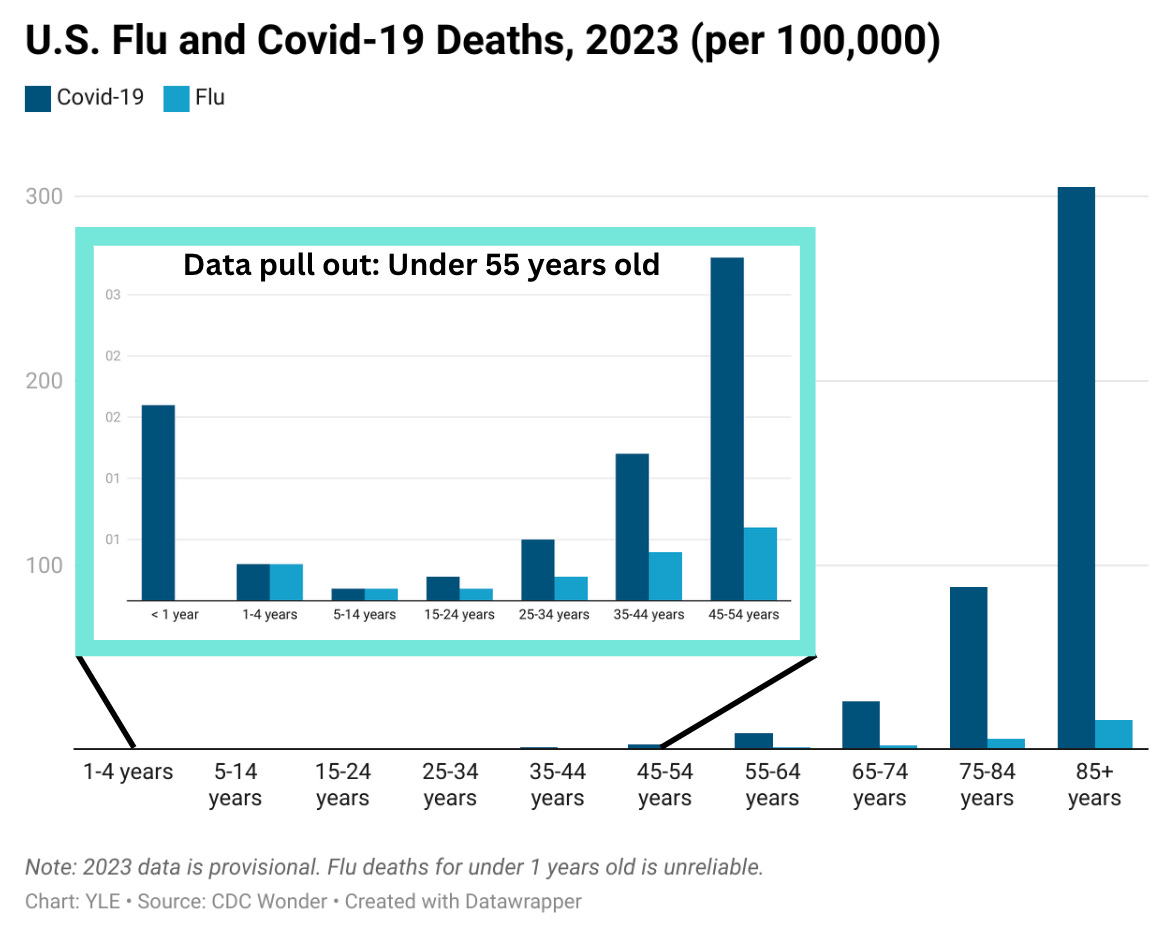
Below is the percentage of deaths attributed to flu (blue) and Covid-19 (orange). We still see a whole lot more orange compared to blue.
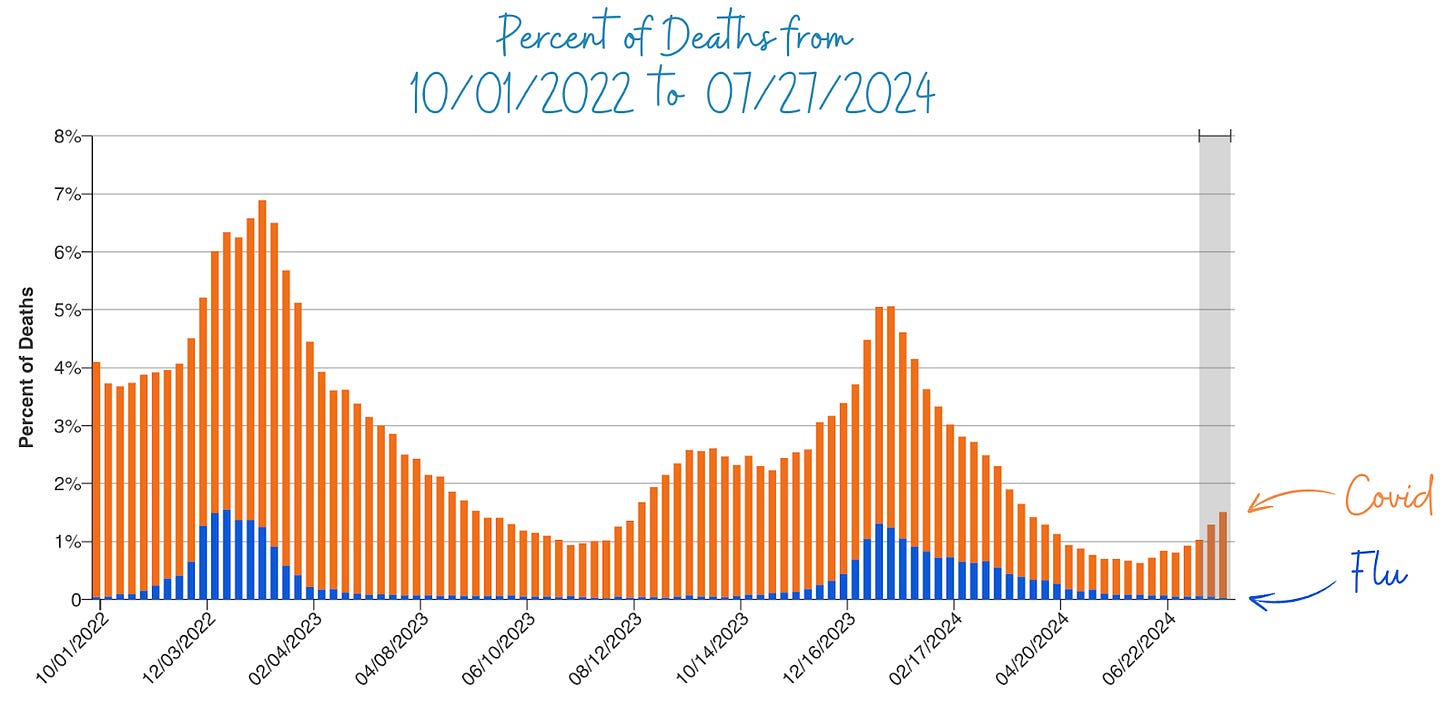
This is the case across almost all ages except between 1- 14 years old.
However, death surveillance may be biased. For example, more people may write Covid-19 on death certificates than flu.
So, the Veterans Affairs St. Louis Health Care System examined health records of 11,000 patients this past 2023-2024 season. They found that 6% of patients hospitalized with Covid-19 died within 30 days of admission versus 4% of patients with flu. In other words, the risk of death from Covid-19 was 35% higher than from flu among hospitalized patients.
However, there are two silver linings:
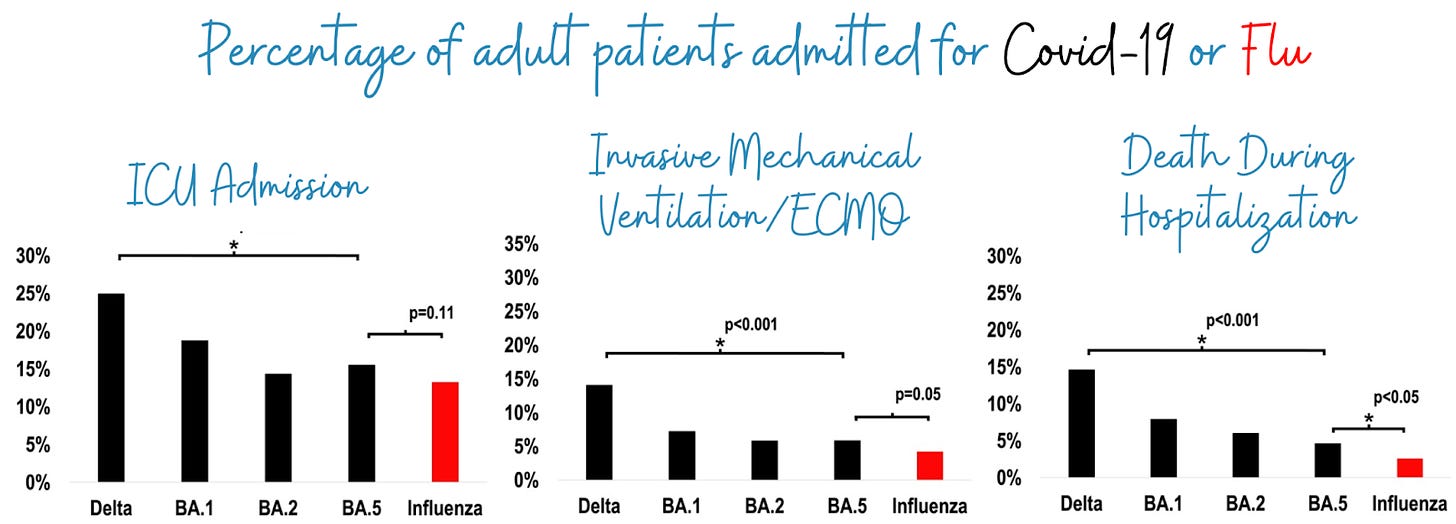
The gap between flu and Covid-19 is decreasing. In the prior year (2022), scientists noted a 60% higher risk of death for hospitalized Covid-19 patients.
Hospital outcomes are becoming more similar. Another study compared hospital outcomes of patients in 2021 (Delta) to 2022 (Omicron) and found that the severity of outcomes decreased, meaning that fewer and fewer people had to be admitted to the ICU, fewer received invasive treatment, and fewer died over time.
While the threat of severe Covid-19 to our individual lives might have decreased, the burden on our healthcare system and economy continues to persist. A report from McKinsey & Company estimated endemic Covid-19 would add $220 billion to our total healthcare costs by 2027, mostly driven by outpatient costs.
Flu isn’t necessarily something to brush off, either
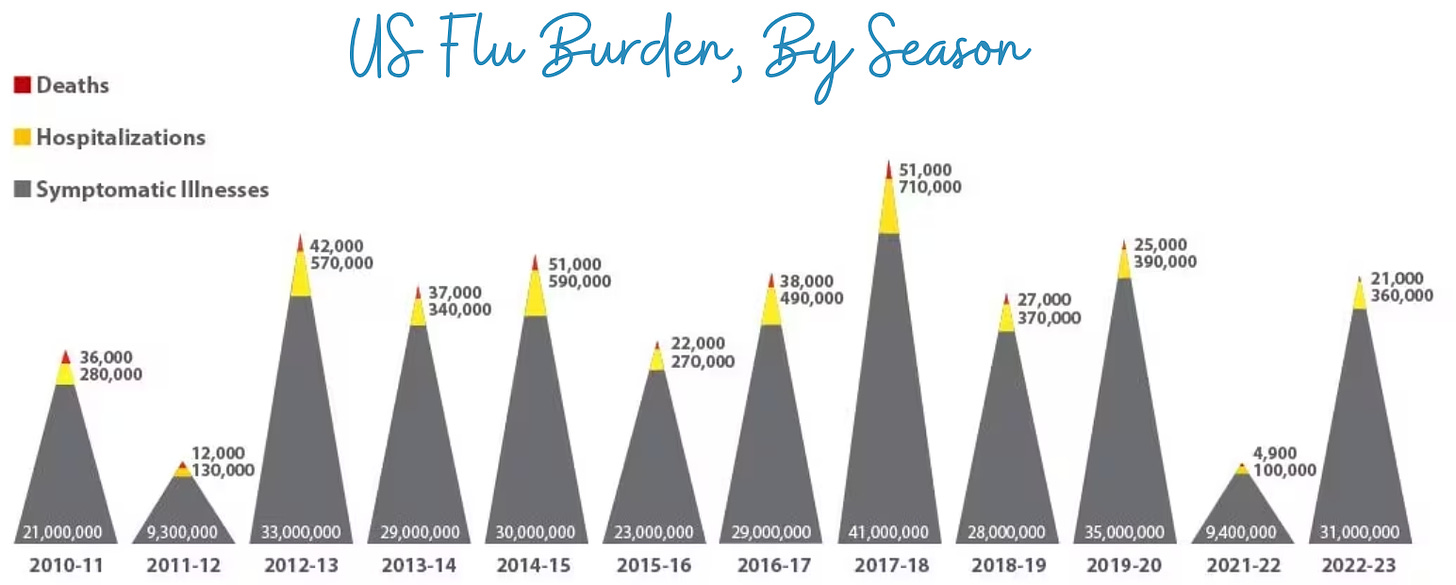
Although Covid-19 is still more severe than flu, it’s important to remember that flu causes a lot of preventable morbidity and mortality. Each year, between 140,000 and 710,000 are hospitalized for flu in the U.S., and 12,000 to 52,000 Americans die. The economic burden of flu is estimated at $11.2 billion per year.
Flu can also cause “long flu” just like Covid-19 can (albeit at different rates—there’s a higher risk of long Covid than long flu, which YLE touched on previously).
The flu- vs. Covid-19 vaccine paradox
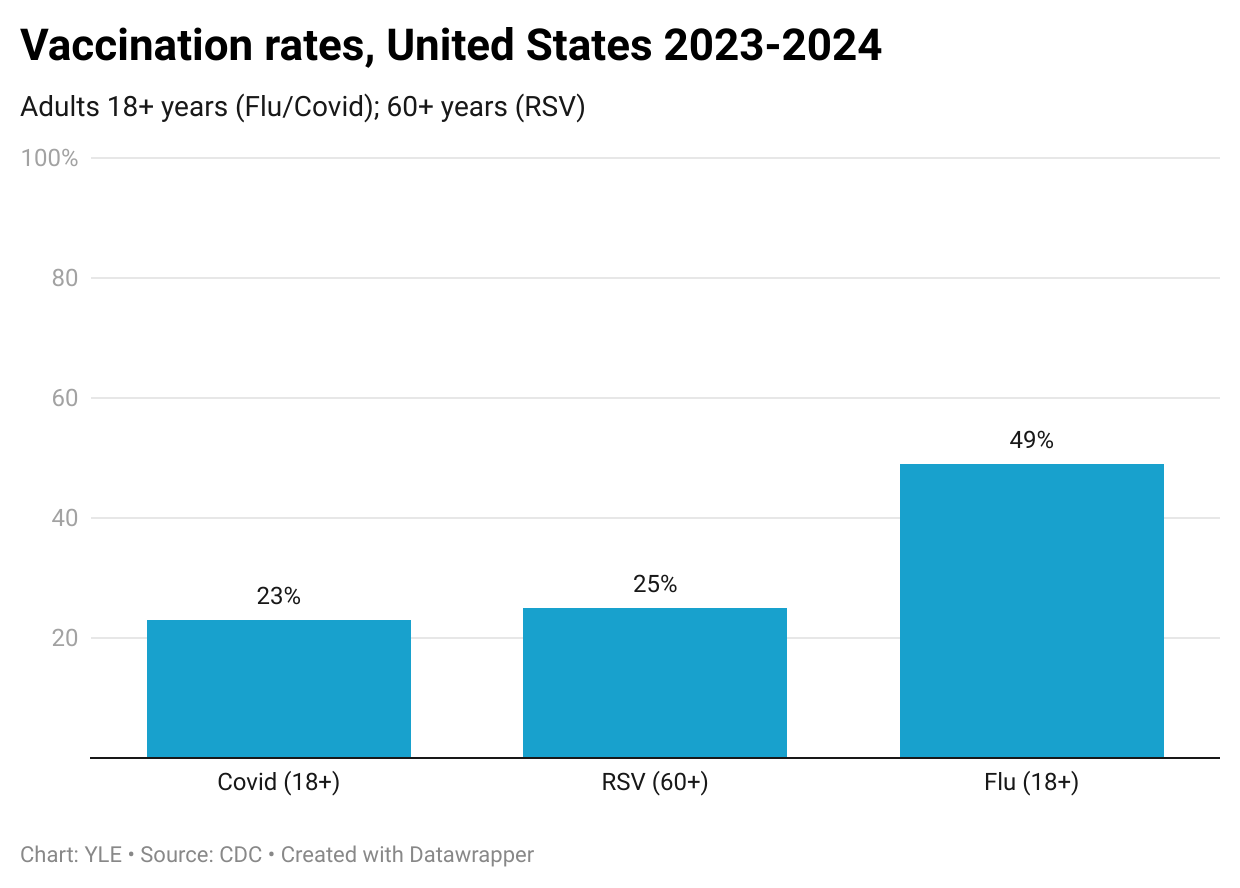
Despite Covid-19 being more severe than flu, far fewer people are vaccinated for Covid-19 than flu. Last fall, 1 in 4 U.S. adults received the updated Covid-19 vaccine, while 1 in 2 received the flu vaccine. This interesting (and disappointing) paradox is mainly driven by loss of trust, vaccine hesitancy, pandemic fatigue, and limited access.
Bottom line
Even as Covid-19 falls in death rankings, it’s still more severe than the flu. Fortunately, for both, we have vaccines. But we need to actually utilize them so these viruses stop costing lives and disrupting our economy and overall well-being year after year.
Love,
Andrea Tamayo
Andrea Tamayo is an intern at YLE. She is a health and science journalist, and recent graduate of the University of California, Santa Cruz Science Communication Program. You can find more of her stories at andreactamayo.com.
“Your Local Epidemiologist (YLE)” is founded and operated by Dr. Katelyn Jetelina, MPH PhD—an epidemiologist, wife, and mom of two little girls. The main goal of this newsletter is to “translate” the ever-evolving public health science so that people will be well-equipped to make evidence-based decisions. This newsletter is free to everyone, thanks to the generous support of fellow YLE community members. To support this effort, subscribe below:





I wish this article had acknowledged that, while there’s good news about DEATH (hooray), COVID causes disability and secondary medical complications (stroke, heart attacks, cognitive impairments, diminished immune function, and diabetes) at much higher rates than flu does. It’s great that the death rate is down, but there’s a real danger that people will see that and stop thinking about the other post Covid issues.
I agree with Nemo and Caryn, this is SoOoo much more than the flu and death rate is not the only way to measure COVID’s impacts. As a physician, I find frequently that these labs may be positive in patients post covid many months after the fact if not years-Fibrinogen activity, d dimer levels, IL6,TNF alpha, IL 17, IL2. We’ve had multiple patients where we suspect “fatigue” was long Covid tested and they had a negative baseline but then “really “ got Covid and are positive for one or all of these biomarkers. Plus with antibody testing we get a forensic history for the patient ( just to note if someone has not been exposed to covid for over 2 years esp if prior infection was mild there is a possibility that the nucleocapside Ab goes negative)Covid has a sustained effect on the immune system. I have seen this in both vaccinated and unvaccinated populations. If public health doesn’t start measuring all its ramifications we will miss its impacts entirely. I have also seen healthy children go into the hospital for “normal” strep infections and at the elementary school level we are suffering from chronic absences that are over prepandemic levels. Nobody bats an eye with school districts being over 20% chronically absent for the last 3 years nationally! Peds are seeing kids sick over and over again again at higher rates. https://www.caschooldashboard.org/
https://www.ppic.org/blog/chronic-absenteeism-in-k-12-schools-remains-troublingly-high/
Children and young persons are also having higher rates of cancer which I know can be multi factorial.
https://www.frontiersin.org/journals/pediatrics/articles/10.3389/fped.2024.1357093/full
https://www.cancer.org/research/acs-research-news/facts-and-figures-2024.html
https://www.who.int/news/item/01-02-2024-global-cancer-burden-growing--amidst-mounting-need-for-services
https://gco.iarc.fr/today/en
But, this implies that the research that UCSF with Dr Peluso et al are correct that their long covid patients have T cell exhaustion ( cd4/cd8 cells) and we have many undiagnosed with it already at this stage including children. One of the jobs of T cells is to fight cancer.
https://youtu.be/rMt6ZV-hHSE?si=kkdZtrSfBVRAPonf
If we don’t follow correlation and timing to covid plus clotting disorders, autoimmune disease, infections, neurologic disease, cancers ( everything that covid affects through the immune system) we will miss its ramifications on society.
https://www.phcc.org.nz/briefing/long-covid-aotearoa-nz-risk-assessment-and-preventive-action-urgently-needed
Unfortunately, not to be a doomsdayer but we now have to consider COVID’s implications on the animal population and whether we are going to wipe out animal species with us through immune dysfunction in their populations. So how will we manage this on a global level at this point… I’m not sure. https://share.newsbreak.com/85s0msco?s=i0