There are several new scientific developments regarding Covid-19 that might be useful to you, given that we are in a big wave right now. Here is a quick research roundup.
(Note: I will dive deeper into long Covid next week. We’ve learned a lot more over the past year. Stay tuned.)
Fall 2023 vaccines are effective
What we know: Recommendations for an updated 2023 Covid-19 vaccine were based on lab and some human data. We didn’t have real-world data or clinical trial efficacy data. (This follows a similar model to the flu.)
New info: Vaccine effectiveness data is rolling in:
70% effectiveness against hospitalization (preprint; Netherlands; among 60+ year-olds previously vaccinated).
Another study found significant added protection for (at least) 30 days against emergency department use, outpatient use, and hospitalization. (Kaiser; among those over 18 years.)
Why does this matter? If you’re up-to-date on vaccines, you can be confident it’s providing additional protection.
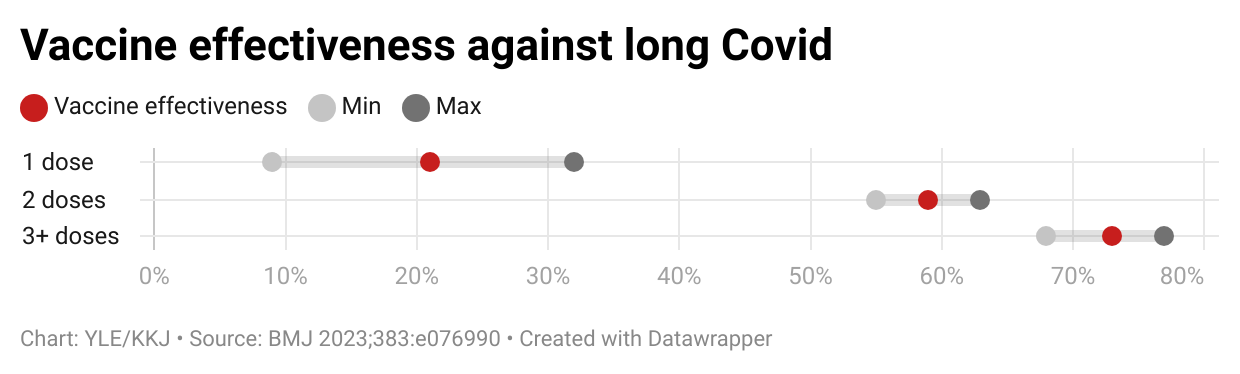
Vaccines help protect against long covid
What we know: Vaccines have many benefits, including preventing long covid. We didn’t know the incremental benefit of additional doses.
New info: A recent study showed that the more vaccines you get, the less likely you will get long covid. This is called a dose-response relationship: One dose of vaccine reduces risk by 21%, 2 doses reduce by 59%, and 3+ doses reduce by 73%.
Why does it matter? Most people still pay attention to Covid-19 to prevent long covid. Keeping up with vaccines helps a lot.
Children and vaccines
New info: We’ve been lacking real-world effectiveness data among children lately. The evidence is flooding in now. Four recent studies show:
Vaccines were highly effective against infection and severe disease across all pandemic periods. Across 4 Nordic countries, for example, there was 73% vaccine effectiveness against severe disease among adolescents. The risk difference was 2 per 10,000 adolescents vaccinated.
Vaccines are safe. The rate and cause of sudden cardiac death in young people was not due to vaccines during the pandemic. One study even included autopsy investigations.
Transmission takes hours
New info: Transmission increased linearly by 1% chance per hour. Most transmission resulted from exposures lasting one hour to several days. Households accounted for 6% of contacts but 40% of transmissions.
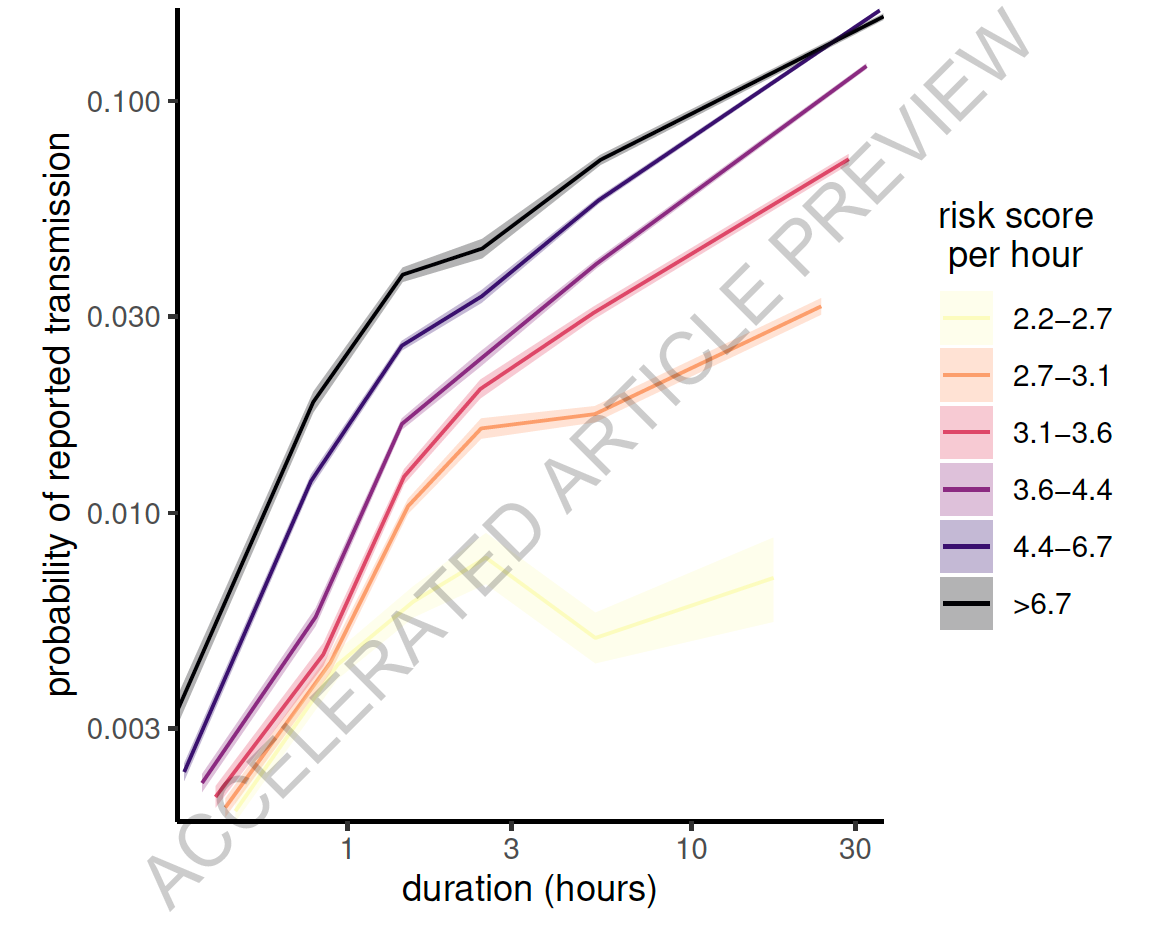
Why does this matter? Transmission = time x proximity. This may help your risk calculations. Quick passersby at a grocery store are far less risky than staying in a house with someone infected.
JN.1 is more severe?
New info: Lab data suggests that JN.1 (the dominant subvariant today) is more severe on a microscopic level than other Omicron variants.
Why does this matter? We don’t know whether this has implications on an individual level (i.e., feeling more crappy). But, it does not seem to affect a population level (hospitalizations are less common than last year). Regardless, it may be worth doubling down on protections right now.
Covid-19 viral load peaking later
What we knew: The virus and our immunity wall have changed significantly over time, which may have implications for antigen testing.
New info: A new study showed that, during the Omicron era, viral load peaked (i.e., had low values in the graph below) on days 3-4. This is very different than the beginning of the pandemic when it peaked at the start of symptoms. (They also looked at the flu, which peaked on days 1-2.)
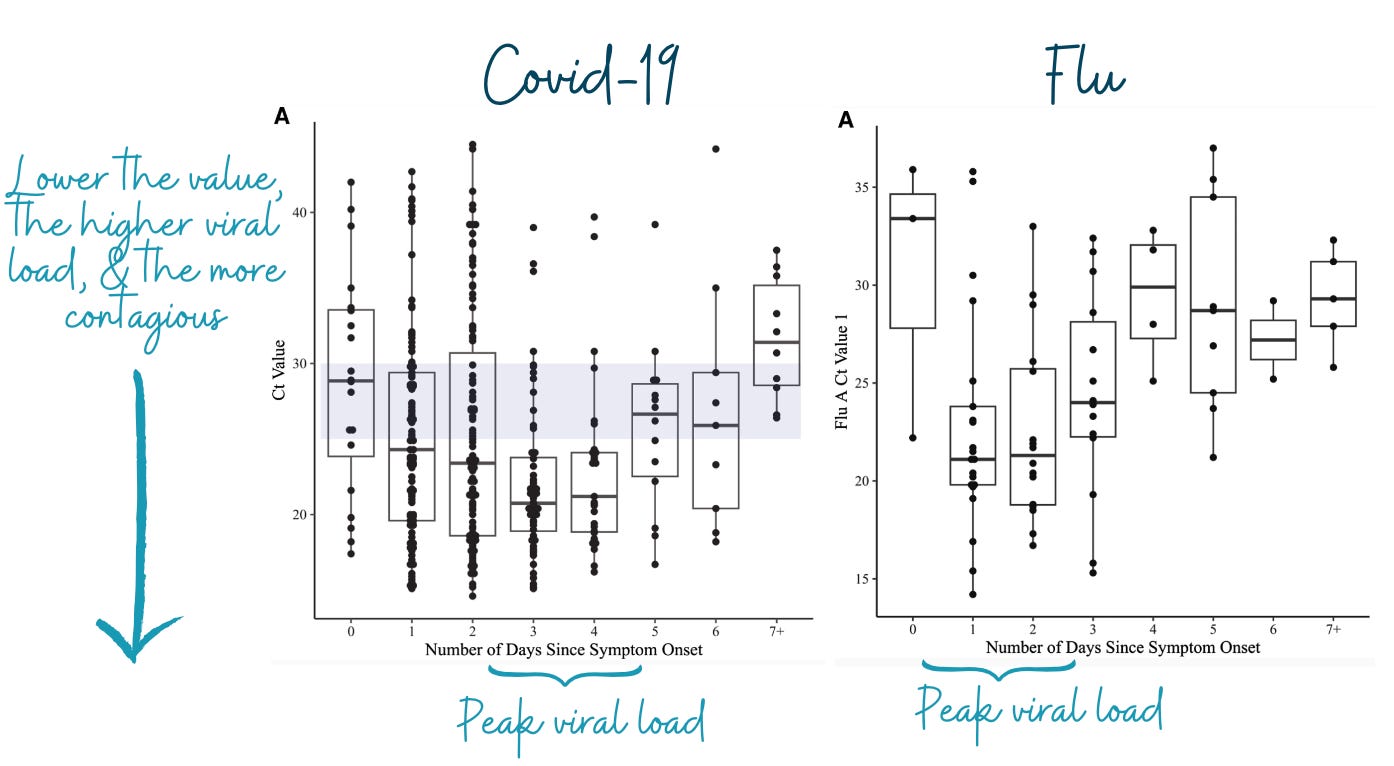
Why does this matter? You may not reliably test positive on a rapid antigen test until the third, fourth, or even fifth day of symptoms. This raises questions on how best to use tests, too, like with Paxlovid (which needs to be given within 5 days of symptoms) and isolation.
No seasonality?
What we knew: Other viruses are sensitive to temperatures, partially explaining the seasonality patterns of flu and the common cold, for example.
What’s new: A recent animal study suggested SARS-CoV-2 transmission is not driven by temperature or humidity changes. SARS-CoV-2 remains capable of transmission under a variety of temperature and humidity conditions. This is surprising.
Why does this matter? We will likely continue to see multiple waves per year, as human behavior and immune status dominantly determine when we get waves of Covid-19 infection, not the environment.
Bottom line
Although we are four years into this thing, we still learn every day. Yes, science can still help us make better and more informed decisions.
You’re now caught up.
Love, YLE
“Your Local Epidemiologist (YLE)” is written by Dr. Katelyn Jetelina, M.P.H. Ph.D.—an epidemiologist, wife, and mom of two little girls. During the day, she is a senior scientific consultant to several organizations, including CDC. At night, she writes this newsletter. Her main goal is to “translate” the ever-evolving public health world so that people will be well-equipped to make evidence-based decisions. This newsletter is free, thanks to the generous support of fellow YLE community members. To support this effort, subscribe below:





Thank you, Dr. Jetelina. This is very useful information. It’s reassuring that having six vaccinations for Covid-19 lessen my odds of getting long covid. Knowing a bit more about how hour plus exposure time is where transmission tends to happen is also helpful. I’m glad I still have plenty of masks and rapid at-home tests. The one question I have is the one you raised—when to test, especially when symptoms may “just” be slight congestion and fatigue.
I don't usually have a criticism, but this statement needs re-visiting: "Quick passersby at a grocery store are far less risky than staying in a house with someone infected. " Too many people are going to interpret this to mean little to no risk and forget that this is in comparison to the much larger risk in a home where you are likely unmasked and spending hours.
You should NEVER pop into the the Walmart or where ever else you like to pop, without a mask. Let's not forget the obscure finding from Australian health authorities who documented a FIVE-TEN SECOND passing contact as a source of infection at a time when this disease was orders of magnitude less infectious. https://www.theguardian.com/world/2021/jun/27/delta-covid-variant-may-be-edging-race-against-vaccines
[Update: Thanks to Martin for finally putting this story from Australia to sleep. It apparently is a result of very sloppy work and is not true. However, this does not mean that the time you spend in a store unmasked is going to work out well for you and should most definitely be avoided, especially if your dash includes standing in line to pay. Don't do that.
Remember the early research and the "15 minute " rule? Don't count on that, either. https://www.npr.org/sections/goatsandsoda/2020/10/09/922385856/coronavirus-faq-whats-the-deal-with-the-15-minute-rule
Unless you have the ability to see virus, as in clouds of cigarette smoke, your best bet is to mask indoors each and every time.]
But there have been more than enough stories of infections picked up more recently by going unmasked for "just a minute" into the viral soup of local commerce. Do not let the above finding she wrote about mis-lead you or others into thinking "quick" means zero. It does not.