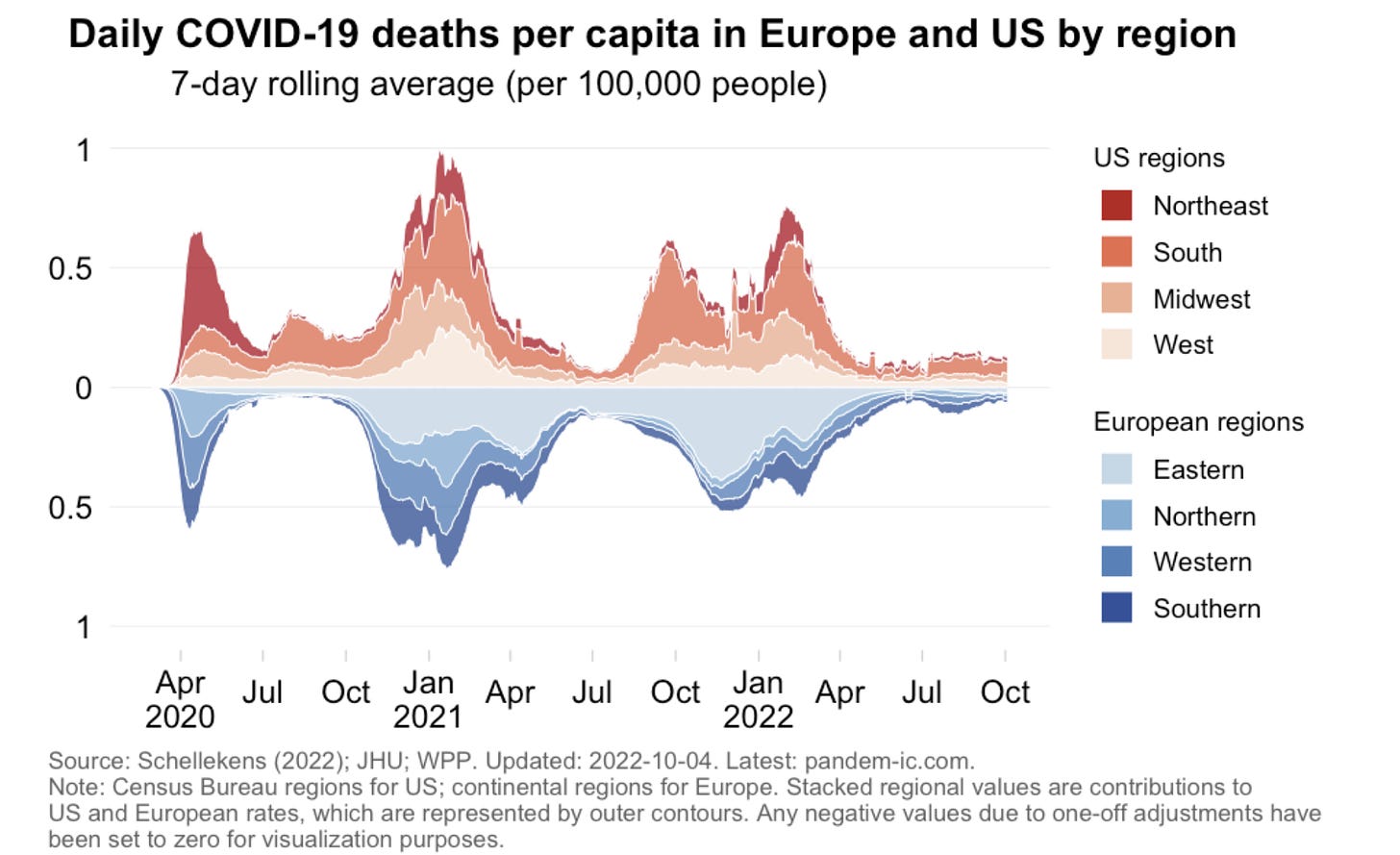
Here we go again. The start of a new wave. Eyes are on Western Europe, as hospitalizations are uniformly increasing. As we’ve seen throughout the pandemic, some are hospitalized “with COVID19,” but it’s important to note that the Germany’s numbers are reported purely as “for COVID19.” In other words, not only are infections increasing, but so is severe disease.

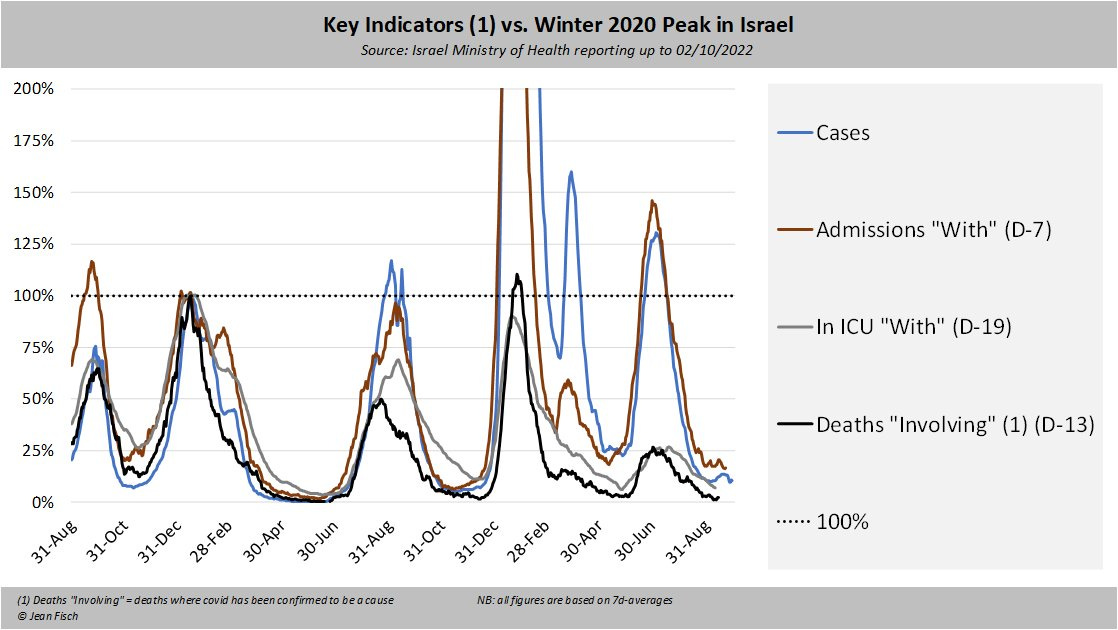
Interestingly, no new subvariant is driving this wave, as the majority of cases are still the “old” BA.5 subvariant. This means changing weather, waning immunity, and/or changing behaviors are the culprit. This theory is only solidified when we see patterns are not changing in neighboring country Israel, for example, whose weather hasn’t started changing yet.
This is concerning because subvariants are brewing. They only make up a small percentage of cases for now, but they are gaining ground; historically, we feel their impact when they make up ~30-50% of cases. These subvariants will eventually add fuel to the fire.
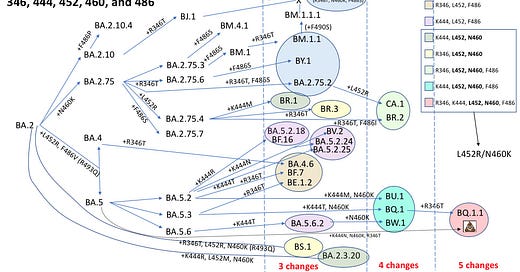
Currently, we have a “subvariant soup” on the horizon—a mix of many different Omicrons trying to dominate the space. Below is a figure of the Omicron subvariants we are closely tracking. Each subvariant has ~10% growth advantage over BA.5, meaning it has the ability to create a wave, but not a tsunami. (As a comparison, Alpha had a growth advantage of 7%/day; the first Omicron BA.1 had a growth advantage of 25%/day).
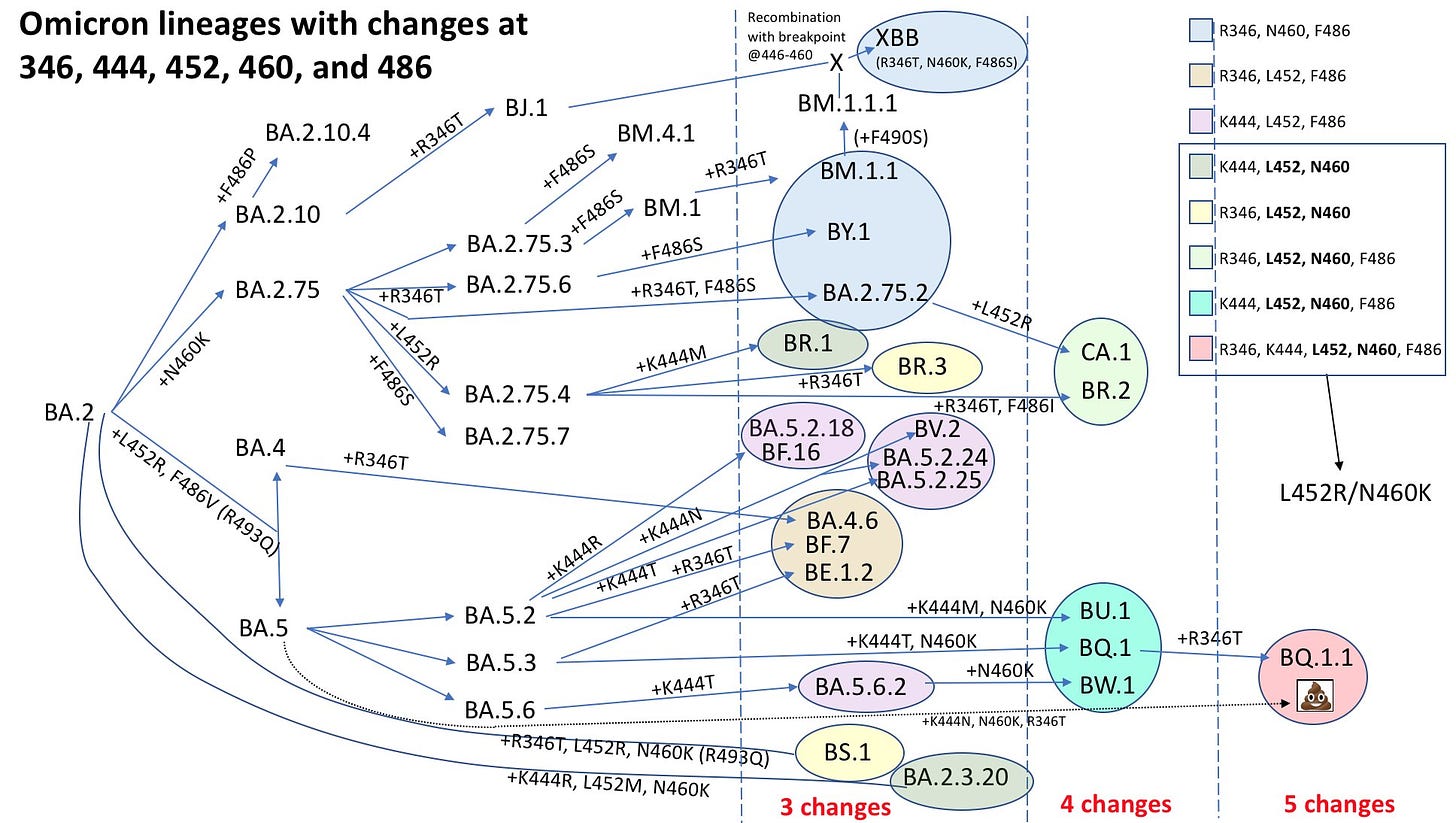
It’s a very busy figure, but there are three specific things to notice:
Convergent evolution. Subvariants with similar mutations are popping up independently across the globe. CA.1 popped up in one place with a R346X mutation, while BQ.1.1 popped up in a different spot with the same mutation. This pattern has been the hallmark of COVID-19, so this isn’t necessarily surprising. What is noteworthy is where these mutations are happening—a spot that helps Omicron continue to partially escape immunity.
Notice BQ.1.1 (in red above). This is a direct descendant of BA.5. While it has the most spike mutations, we picked the BA.5 formula for U.S. fall boosters. Our boosters will work best if this subvariant dominates in the future. For now, BQ.1.1 is winning the race in Europe, so this may have a good chance of taking over in the U.S. We may get lucky.
This is what we know. More than 90% of testing and sequencing has been stopped across the globe. This means we are largely flying blind and there may be a surprise in the mix we are unaware of just yet.
United States
Given the U.S. has mirrored European trends throughout the pandemic, a wave in the U.S. is likely coming.
On a national level, SARS-CoV-2 wastewater has been decreasing the past two weeks, but that deceleration has started to level off. If we zoom in to specific jurisdictions, like Boston, there are concerning signals with sudden increases in viral wastewater levels. Wastewater will continue to be a huge asset moving forward as an early indicator of transmission in communities.
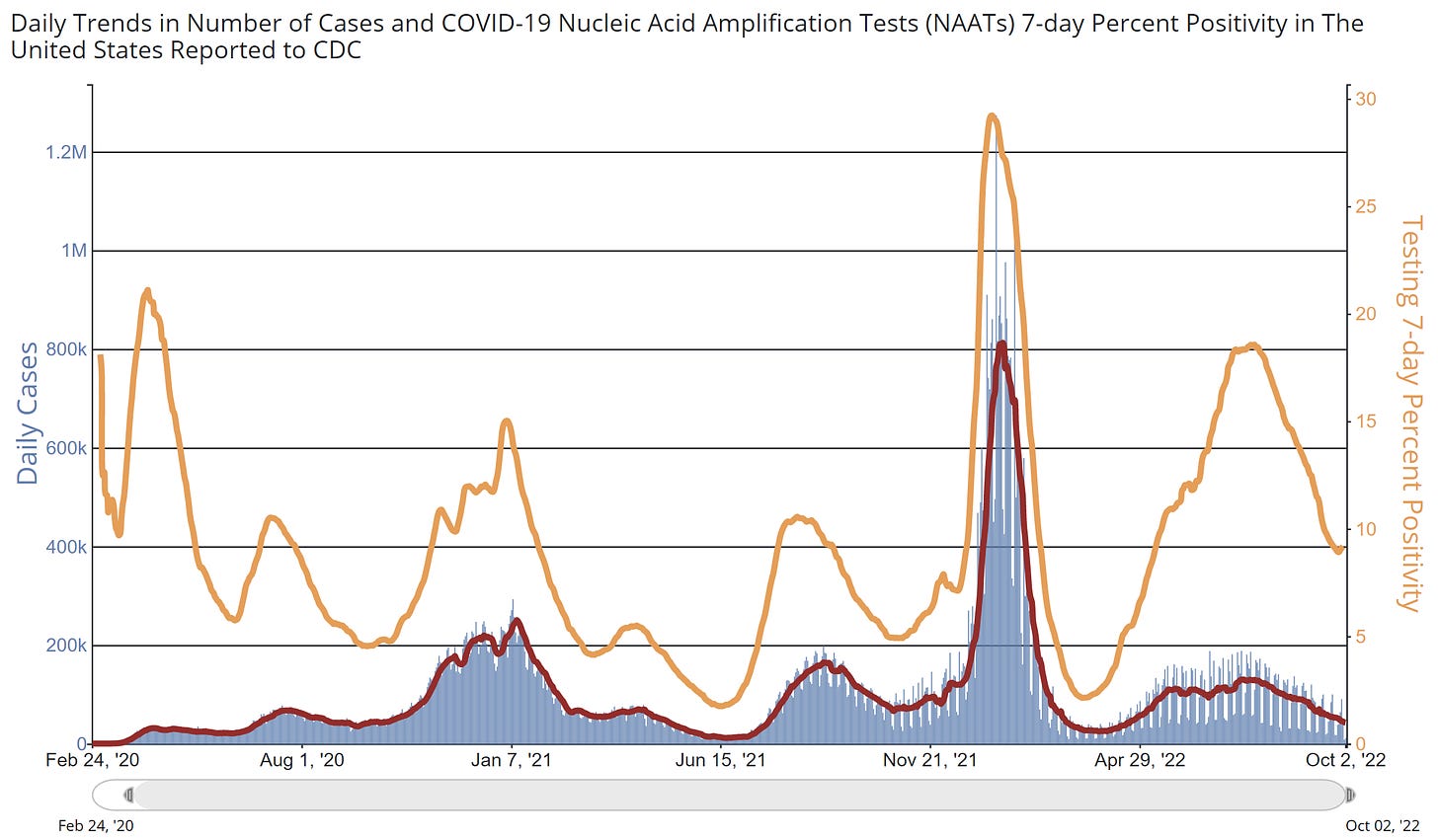
We really don’t know what reported case and testing numbers mean these days, but for what it’s worth national test positivity rate has also plateaued. In the first two years of the pandemic, this metric was a consistent early indicator of what was to come.
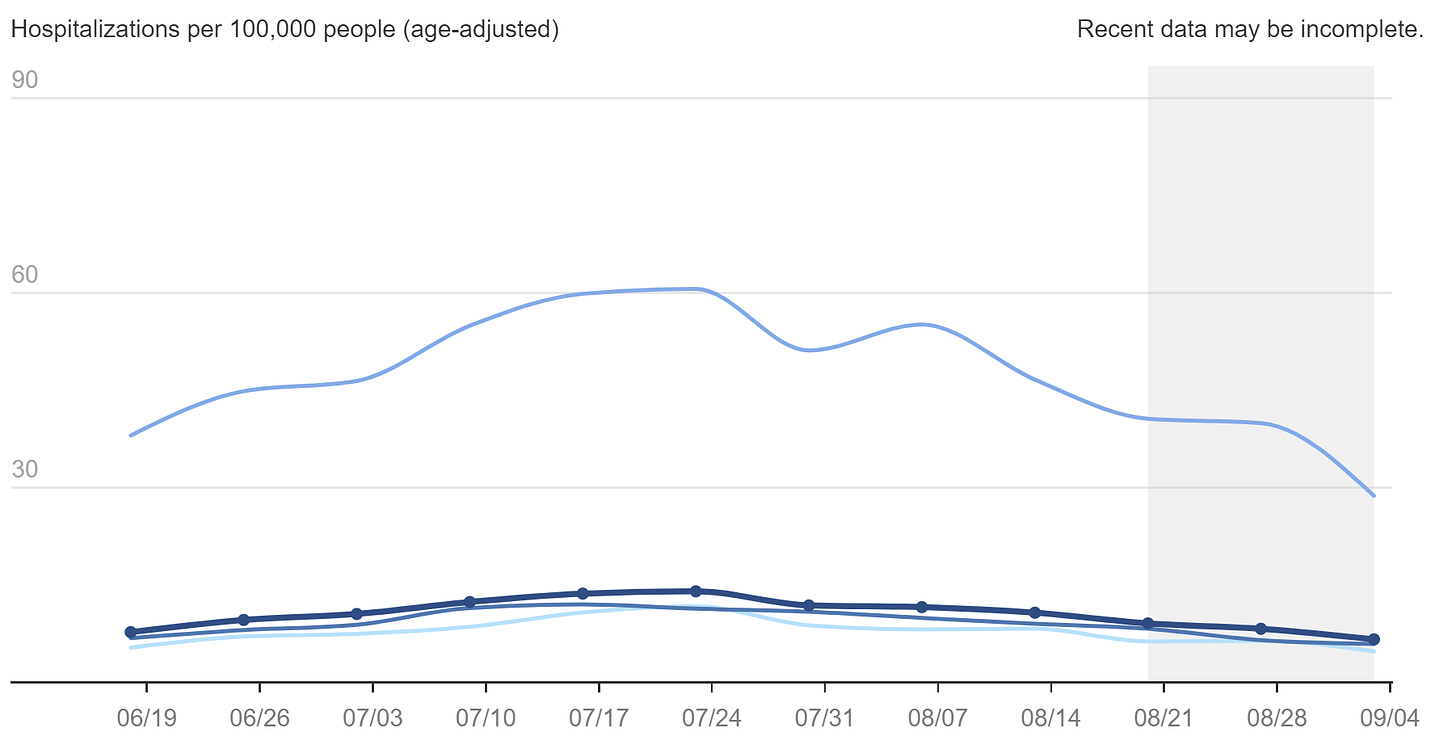
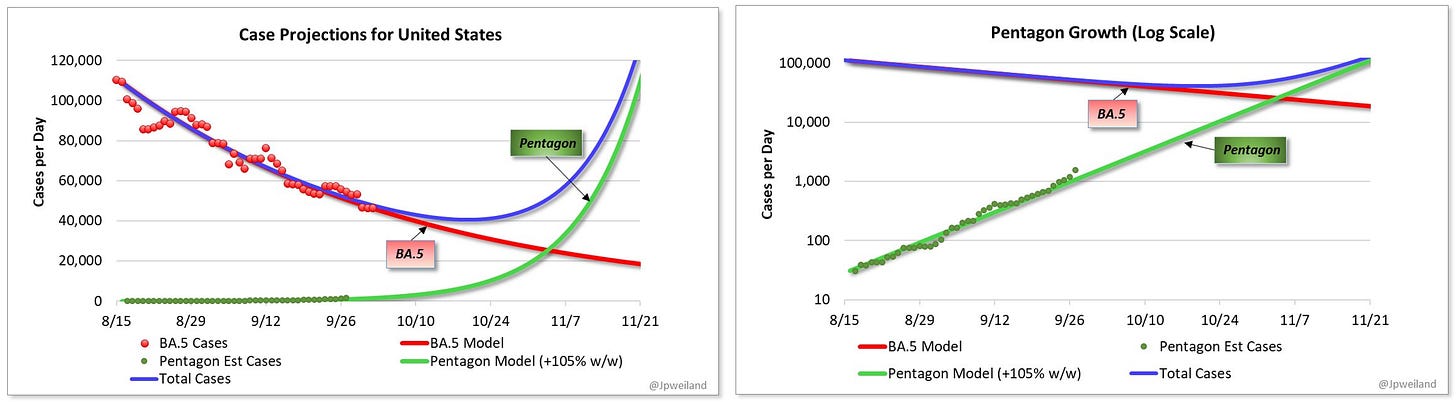
If we combine five of the top new subvariant leaders in the U.S. (referred to as “Pentagon”), it’s clear that case acceleration is brewing below the surface. Given the current growth, we will likely see an impact on national metrics in mid-November.
The height of a U.S. wave is partially dependent on the number of people who get a fall booster. Unfortunately, it looks like the majority of Americans will be going into the winter ill-prepared. A new Kaiser Family Foundation survey found 40% of Americans are unsure if the booster is recommended for them, including about half of fully vaccinated rural residents (54%), Hispanic adults (51%), and those without a college degree (49%). There is clearly a failure of communication and outreach. This must be a priority as vaccines continue to protect against death, severe disease, transmission, cases, and long COVID-19. So far only 7.6 million Americans have received their fall booster.
Bottom line
We may be in for a bumpy ride this winter. SARS-CoV-2 is already gaining ground thanks to weather and behavior change. We expect growth to accelerate with subvariants on the horizon. There’s a lot you can do, but the lowest hanging fruit is to get your fall booster. Also, if you’re older and test positive, remember Paxlovid.
Love, YLE
“Your Local Epidemiologist (YLE)” is written by Dr. Katelyn Jetelina, MPH PhD—an epidemiologist, biostatistician, wife, and mom of two little girls. During the day she works at a nonpartisan health policy think tank, and at night she writes this newsletter. Her main goal is to “translate” the ever-evolving public health science so that people will be well equipped to make evidence-based decisions. This newsletter is free thanks to the generous support of fellow YLE community members. To contribute, subscribe below:





I can give a little insight into the reasons for the slow booster uptake, at least anecdotally from a small Wisconsin town. I went to the local drug store last week, where I almost always get vaccinations (e.g., flu). They are "booked up" for the next 3 weeks for all vaccinations (has never happened before), and are no longer taking appointments after that because they have nobody to administer the shots, even though they have the vaccine on hand. On I went to the local hospital, it took 3 phone calls and 20 minutes: you make a vaccination appointment just like you make a doctor's appointment, and they are offered only on a few days. The situation is no better with flu vaccine (I'll skip the longer story about how my previously reliable Medicare Advantage Plan has managed to screw that up this year). I'm almost 80 and have the time and knowledge to navigate this obstacle course (professional background includes medical sociology and social epidemiology), but to me it represents a massive failure in our public health system. There should be vaccine trucks like ice cream trucks hitting the streets and public events. If the pandemic has proven anything, vaccination is not a "build it and they will come" event. When are we going to learn? As Michael Osterholm is fond of repeating, vaccines do not matter unless you can turn them into vaccinations.
YLE is invaluable, so well explained, timely, clear. Absolutely essential reading. David E. Hoffman