How to (and not to) boost your immune system
The rumor mill is hot with ways to “boost your immune system” this viral season. Legitimate and illegitimate claims on prevention and treatment are entangled on social media and massive podcasts (cough, cough Huberman), making it almost impossible to navigate.
So we pulled together this list for you: What works? What doesn’t work? And why?
Note: The following is just a snippet of a larger document, which can be downloaded at the end of this post.
What works?
If you get symptoms, the best thing you can do is give your immune system time to do its job.
Vaccines can help by reducing viral load, and antivirals can also help stop the virus from replicating. But of the 200+ viruses circulating right now, not all have vaccines or antivirals.
What else can help?
A balanced, nutrient-dense diet. We are not at the point where a diet or specific foods can be recommended to ensure an optimally functioning immune system. This is because our immune system is complex and relies on a balance of many factors. In general, focus on diets rich in produce, fiber, whole grains, lean proteins, and vegetable oils. The most robust evidence of a nutrient-based diet is on specific health outcomes (like stroke, hypertension, or heart disease). However, there are meta-analyses showing a positive, direct impact on the immune system, too.
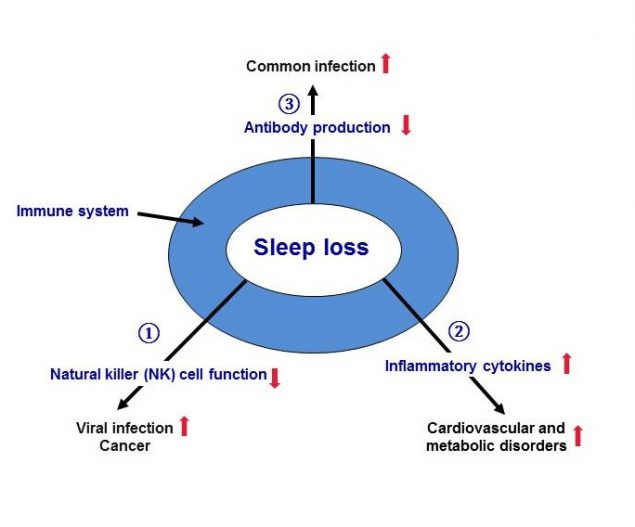
Sleep is critical, as this is when the immune system executes most of its repair processes. This includes the production and regulation of important chemicals required for immune cell function, communication, and tissue regeneration. Those who are chronically sleep-deprived are shown to get colds more often than those who aren’t.
Hydration. Proper fluid balance ensures your body can transport nutrients and immune cells and remove pathogens and waste products (via draining lymph nodes). In addition, proper hydration allows your mucous membranes to maintain their protective barriers.
What does not work?
Many other immune health remedies land in one of three categories:
No evidence of working despite being tested repeatedly
Little evidence either way
Weak evidence for one thing, but claims are exaggerated
Here are the most popular misconceptions:
You do not need to get re-infected to keep your immune system active. Contrary to rumors, we don’t need to get re-infected over and over for our immune systems to be ready to respond. Everything in our life—our house, pets, our own body—is filled with microbes. Although these microbes aren’t harmful, they share enough structural similarities with dangerous microbes to keep our immune systems active and ready to defend against dangerous foreign invaders. Infection doesn’t aid in that.
For the general population, dietary supplements do not work in preventing or reducing the severity of illness. Ingesting one nutrient only benefits those with a substantial deficiency or in a specific subpopulation (e.g., pregnant, lactating). What about…
Vitamin C? A balanced diet can readily obtain the necessary levels to support immune function. There are a lot of misconceptions about megadosing vitamin C for sickness, which stemmed from three things: 1. Vitamin C prevented scurvy in sailors a long time ago, which suggested some role. 2. A book in the 1970s supercharged this misconception with common colds. 3. Some animal studies and small but poorly conducted human studies are often cited as proof.
Vitamin D? Very low vitamin D levels can reduce your ability to deal with respiratory infections, but this level of deficiency is very uncommon in high-income nations like the United States. A recent meta-analysis of randomized controlled trials found that vitamin D supplementation did not impact respiratory illness among subgroups. Only when data were pooled was a small effect (1%) noted, which is unlikely to have clinical relevance.
Iron? This is critical for immune system function, but paradoxically, it is also critical for many pathogens to do their job. Iron deficiency is most common among women and children, particularly in low-income countries. A medical provider should manage legitimate deficiencies, as iron supplement compositions are not regulated and vary widely.
Probiotics? These are dietary supplements that contain live microorganisms, such as bacteria. No evidence suggests that people with normal gastrointestinal tracts can benefit from probiotics for respiratory health. There may also be risks for with individuals with compromised defenses, like children. (There was a recent warning from the FDA to probiotic company after the death of a child.)
There are two problems with supplements:
They aren’t regulated for safety or efficacy. This means that even if you’re buying the same exact supplement from the same exact company, there is variability in the quality, formulation, and bioavailability (i.e., how much is available for your body to use). There can be too much of a good thing, and supplements are a great example.
The placebo effect is real. For example, in a randomized control study of multivitamins, the intervention group reported better health despite no apparent differences in health outcomes. Another study on sham diet supplements found the same and concluded the placebo effect is even more disadvantageous when the first line of treatment is behavioral.
What else doesn’t work?
Cold plunges or ice baths are increasingly popular for “boosting” immunity, but there is inconclusive evidence based on small and conflicting studies. For example, one study of 10 athletes observed a small increase in white blood cell concentrations in blood after many cold plunges in a row (which one could argue may aid immune function), but another study found it didn’t. One randomized control trial in the Netherlands found cold plunges reduced sickness absences from work by 30%, but not the number of days of feeling crummy. The benefits have to outweigh the risks, too. Sudden immersion in water under 60°F can kill a person in <1 minute and cause cardiovascular stress, especially for those with underlying health issues.
Nasal breathing is a recently popularized phenomenon built off the idea that breathing through your nose is better for your immune system than breathing through the mouth. While it is true that nasal breathing can increase nitric oxide levels (an important molecule for the immune system to function), there is limited evidence of the real-world impact. Nasal breathing is not the primary route of nitric oxide: it’s generated via countless other processes and through the consumption of foods, particularly leafy greens. Nasal breathing has been noted to have some benefits for specific populations like patients recently intubated.
Saunas are often purported to sweat out toxins, boost immunity, and more. However, the evidence is limited. The commonly cited study used to justify saunas has serious limitations. For example, the study population was small (20 people), all men, and young (20-25). People with the money to afford a sauna or a gym with a sauna are often higher income, likely to exercise and have access to high-quality foods. Also, while they report statistically significant differences after the sauna, the data overlap.
In summary
We have a few tools to help prevent and treat viral illnesses. However, the best tool we have is our immune systems. Our body does a great job of keeping that tip-top shape without fads. Stay healthy out there!
Love, YLE and Dr. Andrea Love
Below is a PDF document that dives into more: prevention, fever-inducing medication, and more rumors about treatment, like zinc, detoxes, and IV infusions.