Long COVID, or medically known as post-acute sequelae SARS-CoV-2 infection (PASC), first came on our radar in Summer 2020. A landmark study described, for the first time, that the morbidity of COVID19 goes far beyond initial infection. Since, studies have estimated between 10-30% adults have symptoms lasting longer than 4 weeks, especially for women and/or for those initially hospitalized for COVID19 (here, here, here). In one meta-analysis, 45 studies found 72% of people (mostly hospitalized) reported at least one symptom for 12+ weeks after initial COVID19 infection.
We don’t really know why long COVID happens. There are at least three hypotheses circulating:
Some people may harbor the virus in an organ, which would be missed by nasal swab. So, people continue to have long COVID symptoms,
Viral pieces stick around in the body causing symptoms for a long time, or
COVID causes the body to start attacking itself (autoimmune type disease).
Another mystery is that some with initial asymptomatic infection mount long COVID down the road. Something (or more likely a combination of somethings) trigger it.
So, what can we do to prevent, or at least reduce, the burden of long COVID?
Vaccines
Before the roll-out, we hypothesized vaccines would prevent infection (and thus prevent long COVID). We also hypothesized vaccines would reduce viral load among breakthrough cases. Vaccines minimize the time the virus is in the body and reduces the number of infectious particles. So, the less virus, the less likelihood of damaging organs, and the less likelihood of long COVID.
Now that vaccines have been around for almost 12 months, the vaccine’s impact on long COVID is starting to surface. And the results are encouraging. There have been three studies thus far.
First study
The first study was published in the New England Journal of Medicine. Scientists investigated breakthrough cases among healthcare workers in Israel from December 19, 2020, to April 28, 2021 (before Delta). They wanted to describe the rate and symptoms of breakthrough cases. What did they find?
Out of 1,497 vaccinated (with Pfizer), there were 39 breakthrough cases
Among the breakthrough cases, 19% had symptoms lasting more than 6 weeks (i.e. long COVID). This included loss of smell, cough, fatigue, weakness, difficulty breathing, and/or muscle pain.
So, long COVID19 can occur with breakthrough cases, but it’s relatively rare. In this study, the rate of long COVID19 among vaccinated was 0.5%.
Second study
A second more recent and much larger study was published in the Lancet. It compared the rates of long COVID19 among vaccinated to unvaccinated adults in the UK. The scientists leveraged a massive sample (1,240,009 adults). They assessed the rate of partially vaccinated breakthrough cases (positive test after 1st dose but before 2nd dose) and rate of fully vaccinated breakthrough cases (positive test after dose 2). They also compared the duration of symptoms among breakthrough cases compared to unvaccinated cases. What did they find?
Of the ~1.2 million adults, there were 6,030 (0.5%) breakthrough cases among partially vaccinated. There were 2,370 (0.2%) cases among fully vaccinated.
The rate of long COVID19 among partially vaccinated breakthrough cases was the same as the rate of long COVID19 among unvaccinated (9.2% vs 10.7%).
The rate of long COVID19 among fully vaccinated breakthrough cases was lower than the rate of long COVID19 among unvaccinated (5.2% vs. 11.4%).
So, this study was consistent with the first: vaccines don’t 100% prevent long COVID19. But, they significantly reduce the chances if fully vaccinated.
Vaccine after long COVID
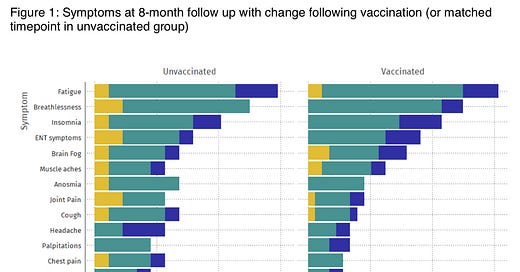
In addition, some adults with long COVID that then get vaccinated are finding a nice surprise. A study found that ~30% of people with long COVID19 reported getting better with a vaccine (~20% said symptoms got worse; 50% said symptoms stayed the same). When the scientists compared long COVID19 to unvaccinated, there were also promising results:
14.3% of symptoms worsened in unvaccinated individuals compared to 5.6% of vaccinated patients
15.4% of symptoms improved in unvaccinated patients compared to 23.2% of vaccinated patients
So, vaccines help some alleviate long COVID19 after vaccination. Why? We think the vaccine is helping the immune system in one of two ways:
The vaccine clears some of these reservoirs in the organs and essentially eliminates the cause of the problem.
The vaccine reprograms the autoreactive cells. Basically, the vaccine tells the cells that are attacking to stop.
Is this temporary relief? Maybe. Is it a combination of #1 and #2? Likely. An immunologist (Dr. Akiko Iwasaki) said on NPR:
“The fact that not everybody's feeling better after the vaccine indicate that there may be multiple reasons why people are suffering from long COVID.”
What about with children?
These studies did not include children because vaccines haven’t been available for very long. We are at the mercy of time. Studies will be coming, but in the meantime we hypothesize that vaccines will reduce long COVID among kids too.
Excitingly, the National Institutes of Health announced this week the start of the long-term study of children with COVID19 disease. This study will enroll at least 1,000 children ranging from birth to 21 years. The scientists will track the long-term health effects of COVID-19 and attempt to determine risk factors (for example, sex, race/ethnicity, etc.) for complications. They will also assess whether immunological factors influence long-term outcomes.
Bottom Line: Long COVID19 is complex and we have a lot of unanswered questions. However, strong evidence shows that vaccines help and are our best bet at preventing long-term morbidity altogether.
Love, YLE
“Your Local Epidemiologist (YLE)” is written by Dr. Katelyn Jetelina, MPH PhD— an epidemiologist, biostatistician, professor, researcher, wife, and mom of two little girls. During the day she has a research lab and teaches graduate-level courses, but at night she writes this newsletter. Her main goal is to “translate” the ever-evolving public health science so that people will be well-equipped to make evidence-based decisions, rather than decisions based in fear. This newsletter is free thanks to the generous support of fellow YLE community members. To support the effort, please subscribe here:





I think the jury is still out on this one. Another large study, based on medical records rather than self-reporting, found no difference PASC between vaccinated and unvaccinated individuals: https://www.medrxiv.org/content/10.1101/2021.10.26.21265508v1.full.pdf. And another, based on VA records, found some reduced risk in vaccinated individuals, but far less than the ~50% reduction touted in the Lancet study: https://www.researchsquare.com/article/rs-1062160/v1.
While reducing the risk of infection obviously reduces the risk of PASC, the very high degree of sterilizing immunity achieved right after the second (third?) shot doesn't last very long. Protection vs. symptomatic COVID-19 is more persistent, but small comfort given findings of long COVID symptoms following asymptomatic infections.
Reports of PASC sufferers feeling better following vaccination are interesting, but they could just as plausibly be explained by a placebo effect as either of the mechanisms proposed by Prof. Iwasaki. (On the other hand, this study and the handful of others like it do seem to show that vaccinations doesn't often make long-haulers feel *worse*, which is good.)
In any case, we desperately need some answers when it comes to long COVID. If we're going to "live with" COVID-19 as an endemic disease, then we need to figure out how to prevent it from disabling large numbers of people. The world's social welfare systems can no more sustain such a surge than hospitals can one of severe acute cases.
Just a quick question--why is the percentage of unvaccinated different in these two bullets (under the "Second Study" heading)?
* The rate of long COVID19 among partially vaccinated breakthrough cases was the same as the rate of long COVID19 among unvaccinated (9.2% vs 10.7%).
* The rate of long COVID19 among fully vaccinated breakthrough cases was lower than the rate of long COVID19 among unvaccinated (5.2% vs. 11.4%).