There’s no lack of anecdotal evidence that pediatric hospitals are reaching capacity in many states. This past weekend, Dallas had zero ICU beds for kids.
But, anecdotal evidence can be very different than population-level evidence. So, what are we seeing on a population-level? And, is there anything we should be concerned about?
Epidemiology
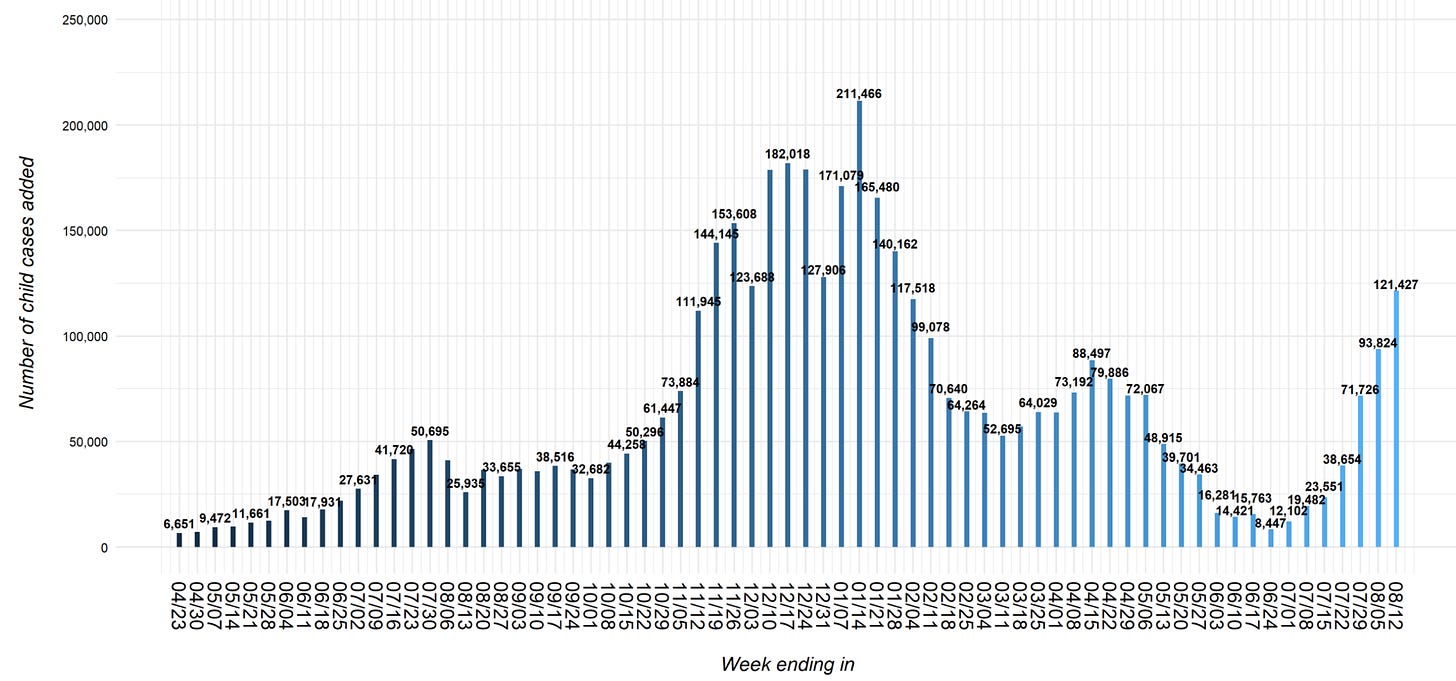
In the past week, 121,427 kids tested positive for COVID19, which represented 18% of the weekly reported cases in the United States. This is increasing at an exponential rate, but adult cases are also increasing exponentially.
In 23 states, 1.9% of child COVID-19 cases resulted in hospitalization. Last Saturday, 1,902 kids were hospitalized for COVID19. The CDC has also made MIS-C (serious condition associated with COVID-19) data publicly available. As of July 31, 4,404 kids were diagnosed with MIS-C associated with COVID19 in the United States.
We are very lucky that kids aren’t as high of risk for severe disease as older adults. But, even given this, I’m still concerned about three things…
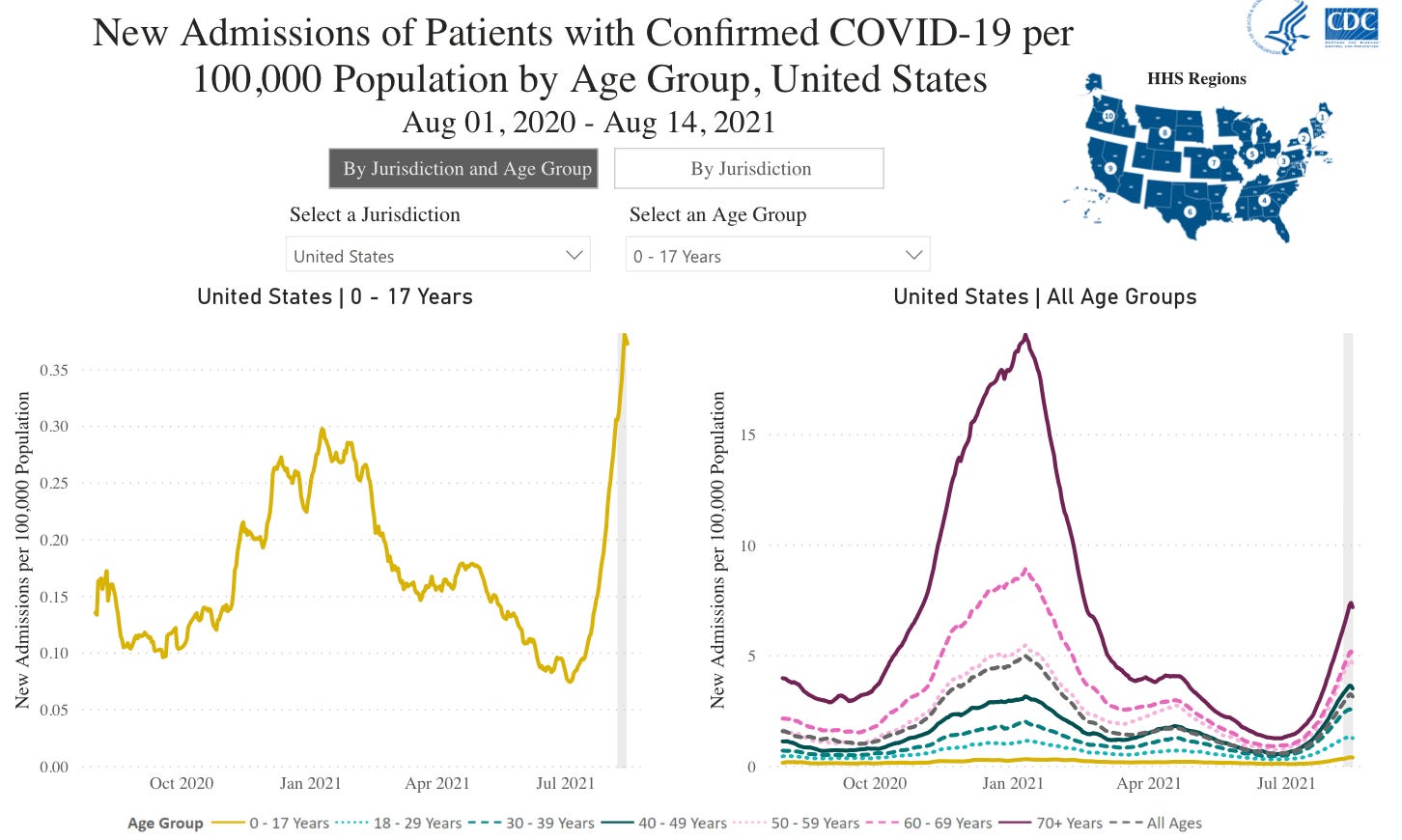
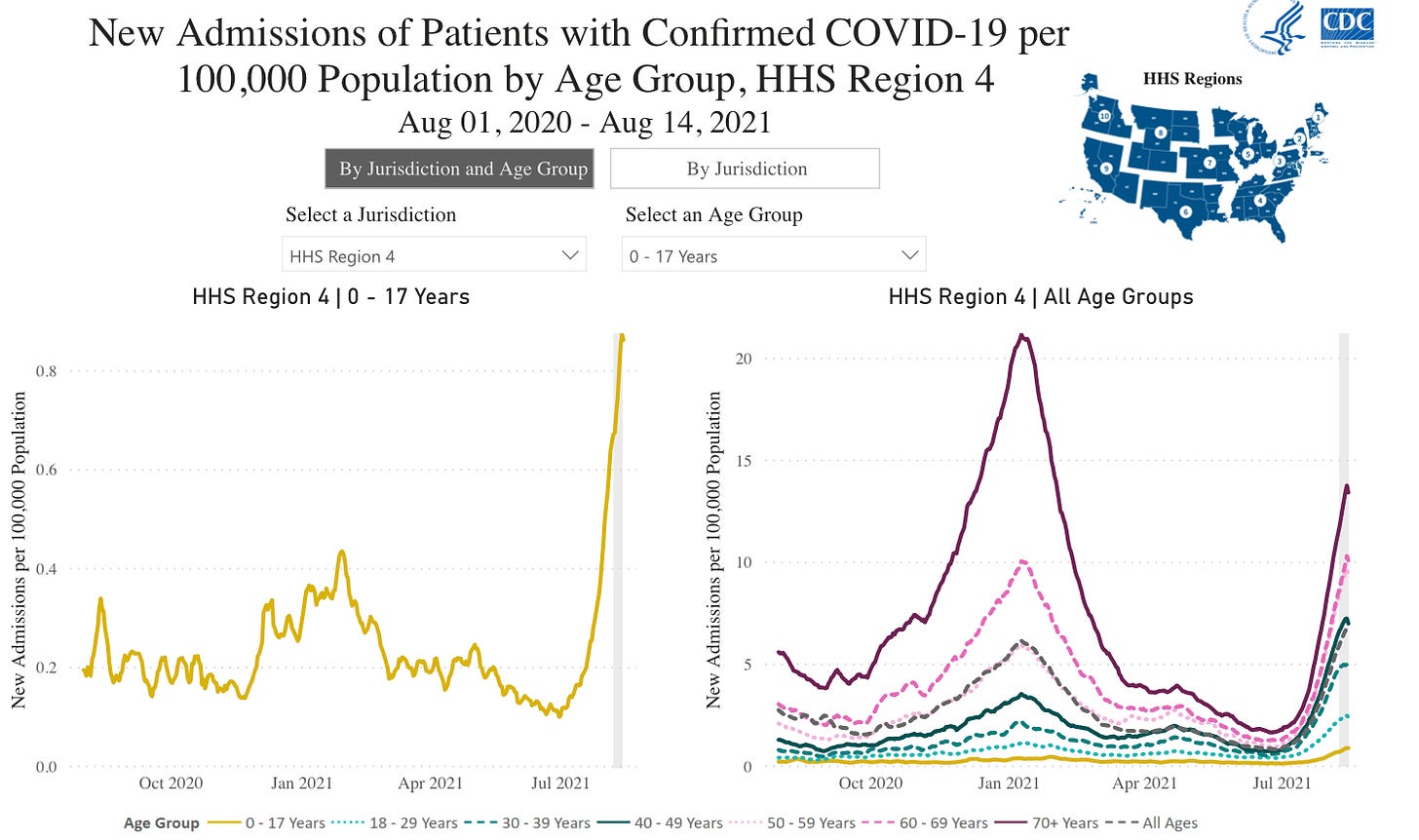
First, the rate in which hospitalizations are increasing. We are far beyond the January peak, which is particularly apparent in the South (second graph). This could be due to pandemic fatigue (we just don’t care anymore). Or this could be due to Delta being more serious than previous variants. There is preliminary evidence from Scotland and Canada that adult hospitalization is more severe with Delta. We have yet to see kid data, but I don’t have reason to believe that it’s different.
Second, pediatric ICU (PICU) capacity. We desperately need to flatten the pediatric hospital curve. Only ~38% of kids have “natural” immunity and the majority of kids aren’t eligible for vaccines, which means we have an estimated 34 million susceptible children in the United States. If 1.9% of infected children are hospitalized, 33% of the kids go to the PICU, and the average hospital stay is 4 days, that means we need 6,800 PICU beds. The U.S. only has 4,500 PICU beds total. (If you want to check the math, go to this amazing thread by Dr. Denise Dewald).
We could easily overwhelm our pediatric hospitals. And this is just with COVID19. RSV is also at an all time high. Car accidents and drownings, for example, are also still happening in the background. We can’t just put kids in adult hospital beds. Kids aren’t tiny adults, they need special equipment, correct dosages, and trained hospital staff (who are getting more and more difficult to find because they are burned out). We also can’t just systematically fly children from Texas (where hospitals are full) to Maryland (where hospitals aren’t full).
What schools do (or do not do) will impact case growth and, thus, impact how our hospitals fare too. A group of scientists in North Carolina modeled what may happen across schools that implement masks and/or surveillance testing. Without masks or regular testing, up to 90% of susceptible students may become infected by the end of the semester.
Third, kids’ role in the transmission chain. Yesterday, an important study was published in JAMA. Scientists sought out to answer how kids of all ages transit COVID19 in Canadian households from June 1 and December 31, 2020. They studied both the index cases and the rate of transmission in the household.
Out of 89,191 households, 6,280 households had a pediatric index case
The proportion of index cases increased with age. For example, 12% of households had an index case aged 0 to 3 years and 38% had an index case aged 14 to 17 years
Younger index cases had a higher proportion associated with a school/childcare outbreak than older kids
Kids aged 4 to 8 years and 9 to 13 years had higher proportion with no symptoms reported compared with index case individuals aged 14 to 17 years or aged 0 to 3 years
1717 households (27%) experienced secondary transmission (i.e. spread in the house)
Of these households, the index case passed it, on average, to 2 other household members
Younger children (aged 0-3) were more likely to transmit SARS-CoV-2 compared with older children (aged 14-17). This was irrespective of factors such as symptoms, school/childcare reopening, or school/childcare outbreaks.
This study tells us that we will not stop transmission in the community without stopping transmission among kids, especially younger kids. This is not only important for pediatric health, but also for adults’ health and to stop this virus from mutating.
Bottom Line: We aren’t sure if this pediatric case increase is the iceberg or just the tip of the iceberg. Delta may be changing the severity of disease, but we have yet to see the science for children. Children could certainly overwhelm hospitals and play an important role in transmission. The next few months will be critical for our children and our community.
Love, YLE








Thank you for this peds-specific post. I use your data all the time in my professional practice (PA for General Int Med) but I just sent my 2 oldest kids to kinder and 2nd grade yesterday and therefore so appreciate this post. Thankfully they attend Dallas ISD schools and masks are mandated (for now); the new data supports this even further. To piggyback on a previous commenter, the idea of 50% of kids getting Covid before the semester is over makes me sick to my stomach- it is hard to feel this helpless as a parent. Keep publishing the truth- many of us out here are listening!
Hello! My kids 5&6 starting school tomorrow. We are in California, so indoor mask mandates and some cohorting is happening at their school. This gives me some peace, but I wish there was some clear data on children's death/hospitaliztion rates and pre-existing conditions. Are these children with pre-existing conditions more vulnerable than heathly children?
Also, can the age ranges of these children be further grouped (under 17)?