Si quiere leer la versión en español, pulse aquí.
The next big scientific discussion bubbling to the surface is the potential of another booster: Will SARS-CoV-2 continue to mutate to escape antibody protection? Do we need another booster? If so, what’s the next formula? For example, do we need an Omicron-specific vaccine? By the time an Omicron-specific vaccine is tested, we won’t have an Omicron wave anymore. So, is there still value in rolling it out?
All of the above are difficult questions to answer because they require predicting how this virus will mutate. Some scientific labs have started this work and the story they are finding is nothing short of fascinating.
Will SARS-CoV-2 continue to mutate to escape antibody protection?
While all viruses mutate in many ways, when talking about vaccines, we’re really only interested in how viruses change to escape immunity (called antigenic phenotype). With this lens, there are two sides of the viral evolution spectrum:
Flu: On one end, we have the flu. It mutates a lot to escape our immunity, and about every 2-5 years our immune systems need a new vaccine formula to fight the virus. The new vaccine formula is fairly predictable, because the virus mutates in a ladder-like pattern: there is one major lineage, and every few years, a new variant sweeps and the others go extinct. (See Panel A in the figure below for a depiction). Because of this ladder, we can predict fairly well—although we are sometimes off—where the virus may go to proactively create the next vaccine formula.
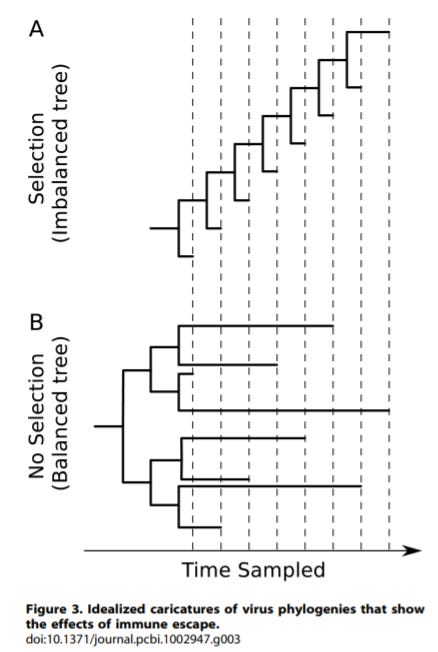
Measles: On the other end of the spectrum is measles. While measles mutates, it does not mutate to escape immunity. It has a more balanced evolutionary tree (See panel B in the figure above). There is no immune pressure that constantly pushes one mutation to outcompete another. So there is no ladder-like pattern. And, thankfully, our vaccines from the mid-1960s still work today.
But the flu and measles are very different from coronaviruses. To understand how SARS-CoV-2 may change to escape immunity over time, we must look at other coronaviruses that have been circulating for decades.
CoV-229E
The Bloom lab explored how another coronavirus—called CoV-229E—evolved over time. This is one of the “common colds” that has been circulating since at least the 1960s, although we think much longer. CoV-229E is probably a good indicator of what’s to come with SARS-CoV-2 because the viruses look fairly similar. Also, and importantly, they are mutating largely in the same physical places. The purpose of this study was to assess how CoV-229E evolved over time, which may give us some insight into how SARS-CoV-2 will mutate over time. So what did they find?
CoV-229E mutated over time in a clear ladder-like pattern, just like the flu (see figure below).
Over time, mutations of CoV-229E eroded antibody protection. In other words, people that were only infected by CoV-229E in 1984 weren’t well protected today.
The rate of antibody erosion was highly variable across people.

This tells us that we should expect a ladder-like evolution of SARS-CoV-2 through which we could predict the next variant.
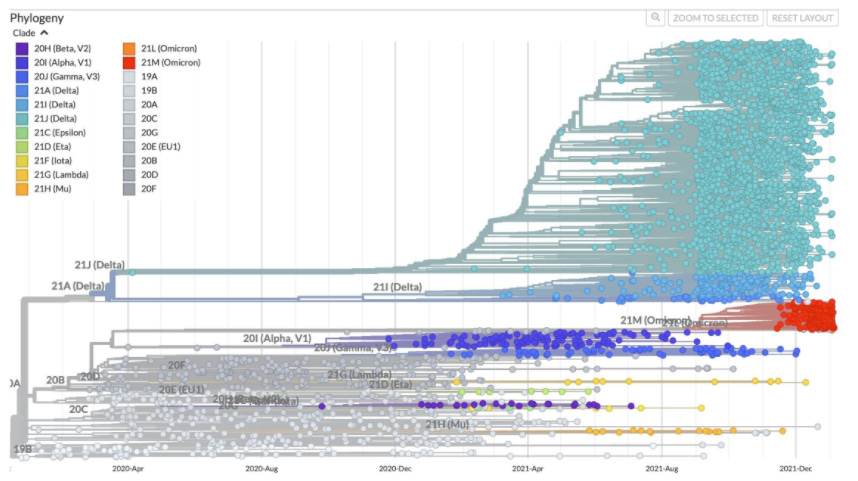
However, much to our surprise, this hasn’t happened
SARS-CoV-2 has thrown us for a loop, as the mutations haven’t evolved in a ladder-like fashion. The next variant hasn’t been coming from the last: Omicron didn’t come from Delta, and Delta didn’t come from Alpha. The fact that SARS-CoV-2 has lacked a pattern of evolution like other coronaviruses or the flu is incredibly puzzling.
But (and this is a big but), we haven’t had a lot of time for this pattern to play out. It’s only been 2 years and other evolutionary trees, like CoV-229E, also had 2-year time frames in which there were no ladder-like changes.
We expect the ladder-like pattern to arise with SARS-CoV-2 eventually. But because it hasn’t yet, we don’t know which direction SARS-CoV-2 is heading. This makes proactively predicting the next booster formulas challenging and risky (from financial and logistic standpoints). This leads us to the next question…
Do we need another booster right now?
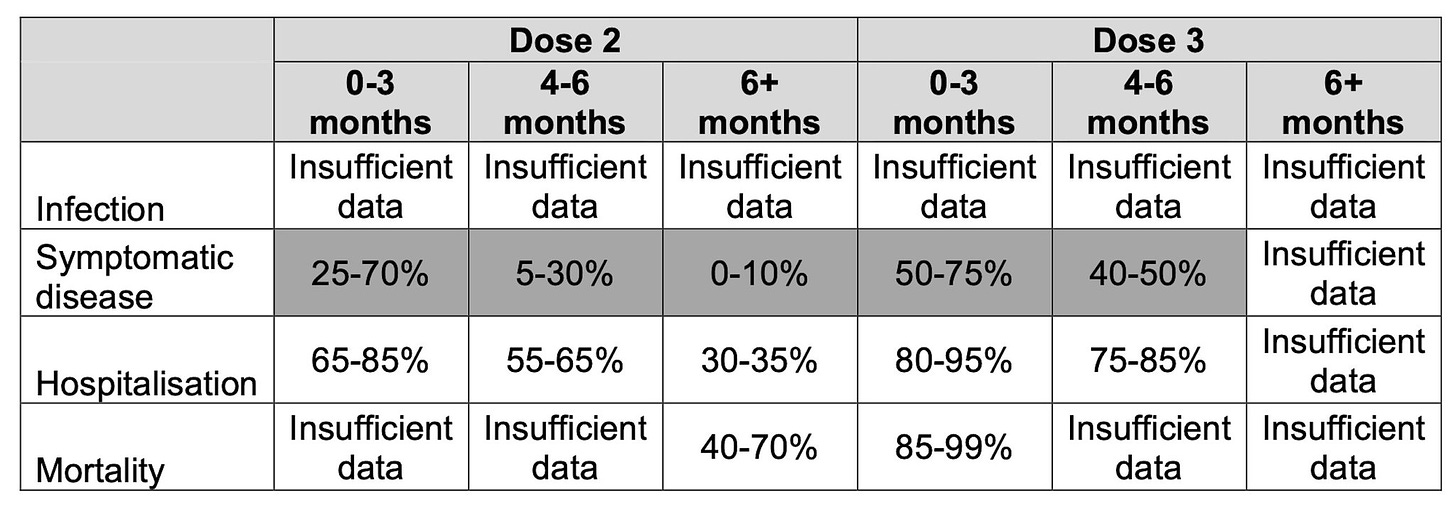
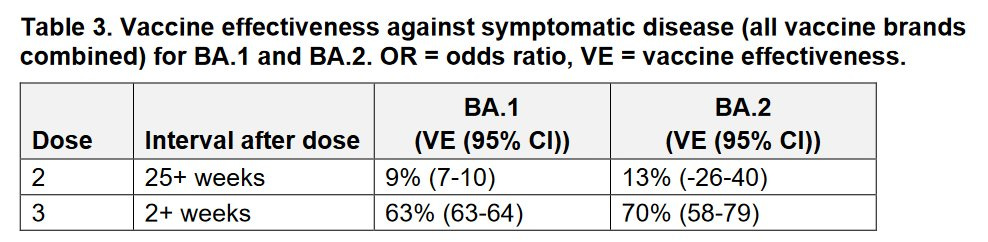
There are really two camps of thought right now:
There is not enough evidence that we need another booster. Boosters are working fantastically well against severe disease during the Omicron wave. For example, in the U.K., we see that even 4-6 months after inoculation, efficacy of a booster against hospitalization is 75-85% compared to 2-dose series, which has an efficacy of 30-35%. This is even the case with BA.2 (sister lineage of Omicron), where there is less immunity escape than BA.1. The same goes for those that received the original J&J with one booster. A study out of South Africa found that a second dose of J&J was 85% effective against hospitalization during a time when Omicron was circulating, compared with 63% after one dose. In addition, T-cells, our second line of defense that keeps us out of the hospital, are mutating but have much less evolutionary pressure than our first line of defense (antibody protection). So there’s also a chance the current vaccine series will continue to protect against severe disease for a while.
Roll-out another booster vaccine. On the other hand, Israel already rolled out a second booster (not Omicron specific formula) among those aged 60+ years. The Israel Health Ministry just released data showing a 3-fold decrease in severe disease among those with 60+ years with 2 boosters compared to 1 booster during the Omicron wave (see figure below). Looking forward, there’s a good chance the next variant will come from Omicron (although, because we lack a ladder-like pattern, we could be wrong). If Omicron had enough mutations for partial antibody escape, the next variant may have full immune escape. Boosting with an Omicron-specific formula would then significantly prepare us for what is to come.
Bottom Line: As Yogi Berra said, “It's tough to make predictions, especially about the future.” And SARS-CoV-2 is making it even more difficult with its random evolutionary patterns. The booster discussion that will ensue among scientists in the coming months will be imperative to follow.
Love, YLE and the Bloom Lab
Dr. Jesse Bloom, PhD, is a viral evolutionary scientist and Professor at the Fred Hutch Cancer Research Center and Affiliate Professor, Genome Sciences & Microbiology at the University of Washington. He and his team, including Rachel Eguia, led some of the research described above. They graciously ensured that I captured this complex work accurately for the YLE audience. Some of the research was also done by Trevor Bedford and Katie Kistler.
“Your Local Epidemiologist (YLE)” is written by Dr. Katelyn Jetelina, MPH PhD—an epidemiologist, biostatistician, professor, researcher, wife, and mom of two little girls. During the day she has a research lab and teaches graduate-level courses, but at night she writes this newsletter. Her main goal is to “translate” the ever-evolving public health science so that people will be well equipped to make evidence-based decisions. This newsletter is free thanks to the generous support of fellow YLE community members. To support the effort, please subscribe here:






The graphics are especially helpful in understanding the situation. Thank you so much!
Fascinating story. I read that US Army is heading to Phase II with a pancoronavirus vaccine. Would such a vaccine obviate the need for future boosters? Meanwhile, I simply don't get the slow-mo for giving more current boosters. Boosters will save at least SOME lives with 100% certainty. So what's the downside, and how can that possibly compare with lives saved?