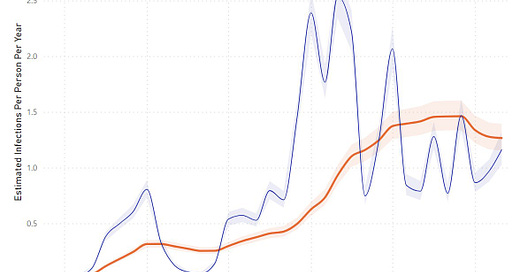
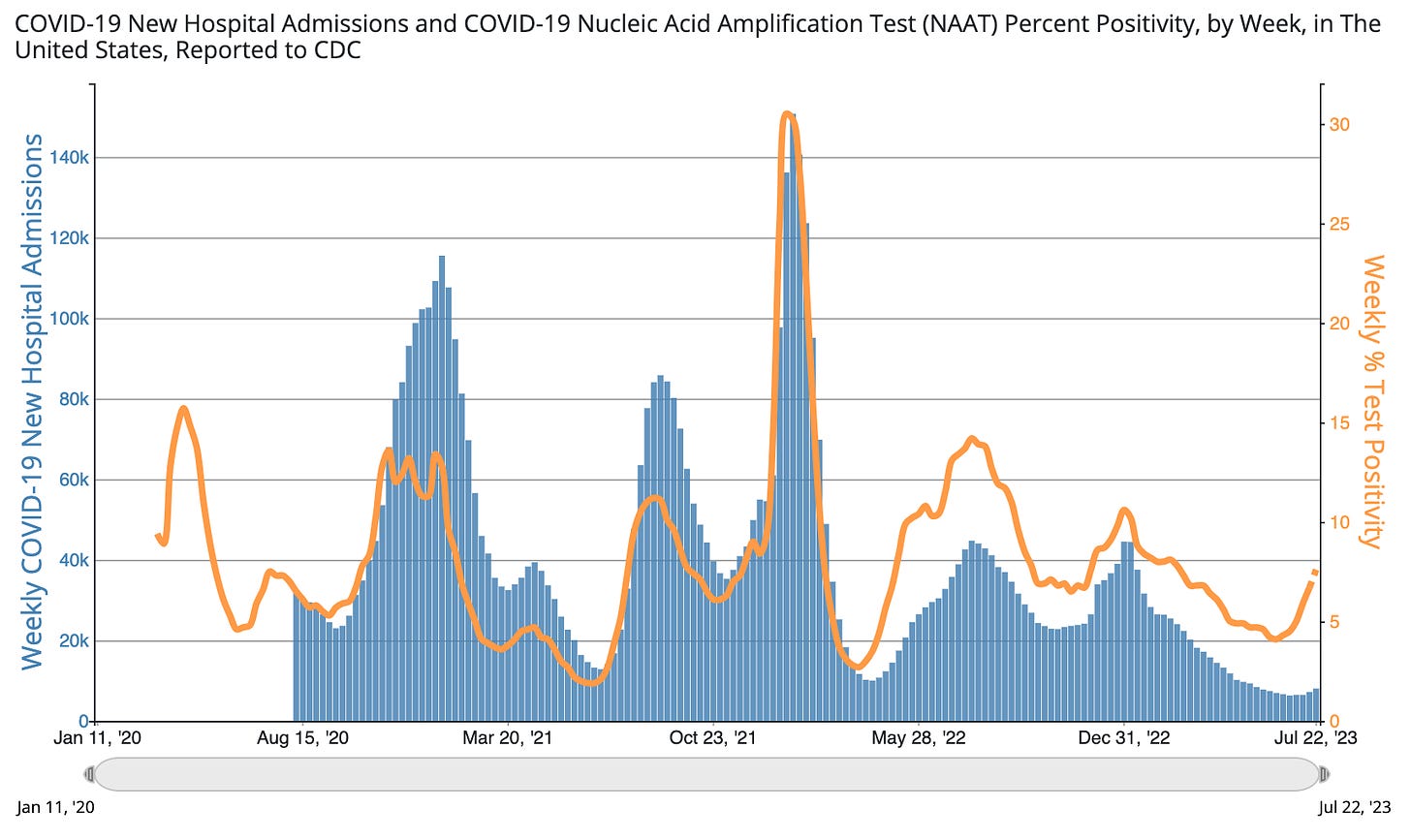
We find ourselves in the middle of a COVID-19 wave. Again. If this summer follows the previous three, we should expect ~10-15% of Americans to get infected.
A nursing home outbreak recently spilled over to my extended family. They had a lot of great questions, particularly about how to manage this virus in 2023. Here are some answers. I hope it helps you, too.
Does health insurance cover at-home tests?
Because the public health emergency ended, coverage depends on your specific insurance plan:
Medicaid: Tests are covered until September 2024.
Private insurance: Coverage is optional, so you must check. (Very few do.)
Flexible spending account (FSA) or a health savings account (HSA): You can use the money to purchase at-home COVID-19 tests.
Uninsured: There’s a stockpile of free tests; use this search tool to find a location.
Do antigen tests expire?
Expiration ranges from 6 months - 2 years, depending on the brand. The date on the box may be incorrect, as the FDA later extended dates. Here is an updated list to see if it’s still good after brushing off cobwebs.
Antigen tests can get too hot (and too cold).
Antigen tests can withstand heat from regular shipping processes. But, if your test has been living inside your car and getting very hot for days, consider it defective.
If you get a negative…
False negatives at the beginning of infection are very common, thanks to the virus mutating. In a recent study, antigen and PCR tests only agreed 47-58% of the time. If they did agree, there was a 1-8 day delay between a PCR turning positive and an antigen test turning positive.
The higher we are in a wave, the more skeptical you should be of a negative result. There are two things you can do to help reduce skepticism (i.e., false negatives):
Swab throat and saliva. These are positive days before the nose.
Repeat testing. Two tests within 48 hours catch 92% of symptomatic cases and 39% of asymptomatic cases. Three tests 48 hours apart detected 94% of symptomatic and 57% of asymptomatic patients.
If you get a positive…
Positives are positives. You’re infectious.
The faintness of a line provides clues, though:
Very bold line= you’re very contagious.
Barely see the line= you’re at the beginning or the end of your infection window.
Should I report my positive to the health department?
I wouldn’t bother. Wastewater is where it’s at these days, and, fortunately, that doesn’t require you to do anything different.
Isolate for five days, at minimum.
When is Day 0? The first day of symptoms (not the day you get a positive test).
When do we leave isolation? Technically the CDC says Day 5. But 2 out of 3 people will still be infectious, so if you do, wear a mask. It’s best to stay in isolation until you have a negative antigen test or it’s been at least ten days.
Where was I infected? Wherever you were ~48 hours before symptoms started.
If you’re over 65, get Paxlovid!
The first question to my 93-year-old relative was: Did you get Paxlovid? I was incredibly disappointed with the answer. The nursing home waited too long to test, so she was outside the eligibility window. (Paxlovid has to be given within five days of symptoms starting.)
She’s not alone. A recent study found only 1 in 4 nursing home residents with COVID-19 were prescribed an antiviral. This is absolutely unacceptable.
How long will I have symptoms?
~6-12 days. Maybe longer, maybe shorter. It depends on a lot of individual factors.
But having symptoms doesn’t necessarily mean you’re infectious. A great way to know is to test to exit (if negative, you’re clear).
Pink eye with kids?
According to the American Academy of Ophthalmology, the newer subvariants of COVID-19 are responsible for some cases of pink eye. In a small study in China, 25% of children aged 2-11 had pink eye during COVID-19 infection. Among adults, it’s much lower rates (1-2% of cases have pink eye).
Should I wear a mask?
In your house: Masks work. A recent study found that if the index case (i.e., infected person) was masked at home, household transmission was reduced by 67%. Not sharing a bedroom reduced risk by 78%.
Going outside. You don’t need to wear a mask to walk your dog.
Does this mean I’m in the clear for Winter?
Maybe. Data from the UK shows that, on average, people get 1-2 infections yearly. You’ll have good protection going into the fall respiratory season. (I would delay a fall booster by at least six months; more on this later).
I’ve never had an infection. Do I have superpowers?
Maybe. Or, perhaps, an infection went undetected. Scientists recently discovered that if you have two copies of a specific gene (HLA-B*15:01), you are 8x more likely to remain asymptomatic. Unfortunately, there’s no way for the average person to know. So, harm reduction is still the name of the game.
Bottom line
A COVID-19 wave is here. Thanks to our immunity wall, 2023 looks very different, but we can still use tools to help minimize disruption. To me, it’s still worth it. (I really don’t want to miss an upcoming summer vacation.)
As we say when catching ocean waves in San Diego: Shaka.
Love, YLE
“Your Local Epidemiologist (YLE)” is written by Dr. Katelyn Jetelina, MPH Ph.D.—an epidemiologist, wife, and mom of two little girls. During the day, she is a senior scientific consultant to several organizations. At night she writes this newsletter. Her main goal is to “translate” the ever-evolving public health world so that people will be well-equipped to make evidence-based decisions. This newsletter is free, thanks to the generous support of fellow YLE community members. To support this effort, subscribe below:




Please let people know that they can report their home test results - both positive AND negative, please! - at MakeMyTestCount.org.
If we can get that address into the public consciousness and get people used to reporting as a matter of course, it would be a great boon. When home multiplex tests come out this winter, you'll be able to report results of flu tests, too. Please - you have such a great reach, please use it to let people know about this resource!
I know 4 people in their late '70s who got Covid, phoned their internists (at reputable institutions on both coasts), and were told they did not need Paxlovid because their files did not indicate they were at increased risk for a serious case. My GP on the other hand, prescribed me and my wife Paxlovid to take with us on a trip, "just in case we needed it", even though we had no particular indicators other than our age (75 and 79). Worrisome that reputable doctors are not in sync with the CDC regarding a proven method to reduce risk of hospitalization and death from this serious disease.