We know that mitigation measures like masks, ventilation, and distancing worked very well in schools last year. Study after study after study after study after study showed this. But this was pre-Delta. Do the same mitigation measures still work in schools? This is what we know so far…
Transmission
In the beginning of the pandemic, we were most concerned about droplets of transmission. But we learned quickly (or not so quickly) that aerosol transmission is mainly driving this disease. In July 2020, 239 scientists wrote a letter to the World Health Organization indicating their concern about aerosol transmission. In April 2021, the WHO changed their guidance and, in May 2021, the CDC changed its guidance that recognized airborne spread as a key mode of infection.
The difference between droplets and aerosol are the size and, thus, the implications of that size. Droplets are large (50-100 micrometers) and so they are heavier. Droplets can travel up to 6 feet, but then they fall to the ground due to gravity. This is why the famous 6 foot rule was implemented. People spread droplets by coughing and sneezing.
Aerosols, on the other hand, are much tinier (<5 micrometers) and lightweight, so they can become suspended in air and float. And you don’t need to sneeze or cough. These can be spread by just talking. Lab studies have shown that aerosols can stay in the air for up to 16 hours. So, a sick person doesn’t need to be in the room with you. They could be in the room before you and had left particles everywhere.
Surface (i.e. fomite) transmission is just not as common, but it can happen. Mathematical models estimated that each contact with a contaminated surface has a 1 in 10,000 chance of infection. In a recent study with hamsters, we saw that surface transmission can result in virus in the nose. But, importantly, the virus does not land directly into the lungs like aerosols do. So the virus replicates less, usually leading to less disease severity.

Delta is incredibly transmissible with a higher viral load. This changes how easy it enters our cells once it reaches us. It seems to becoming more aerosolized too. While washing hands is always a good idea and 3-6 foot distance helps with droplet transmission, we need effective measures to reduce aerosol transmission in schools.
Ventilation
This continues to be one of the best ways to curb transmission. An open window can do a lot to reduce transmission in the classroom from an infected student. The NYT did a great job visualizing the impact of a window in a classroom.
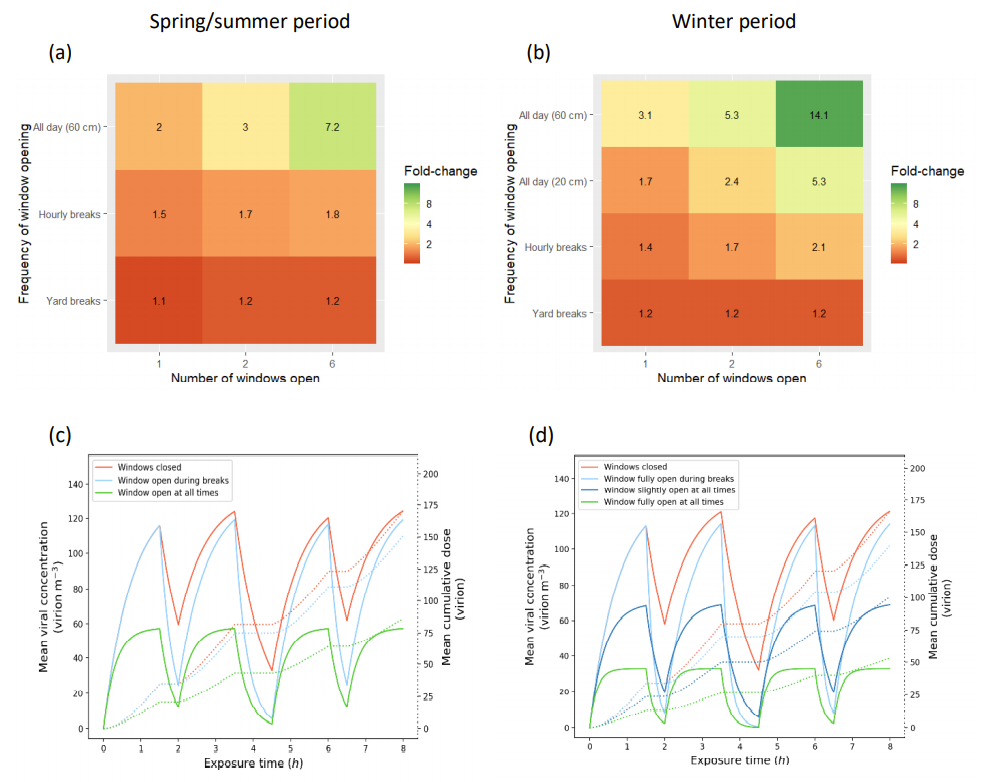
A study this week found that open windows in classrooms can have up to a 14.1 fold reduction in COVID19 transmission. This is highly dependent on the time of year (Summer, Spring, Winter), number of windows, and the frequency in which those windows are open. For example, an open window during the winter is much more impactful than an open window during the summer (14.1 fold decrease vs. 7.2 fold decrease). Also, just opening the window during recess can help a little but not as good as opening a window all day long.
A fan and clean air filter works great too. This can be accomplished using high-efficiency particulate air (HEPA) filtration systems. A Johns Hopkins study found that HEPA filters were responsible for a 65% drop in COVID-19 transmission. Another study found that one HEPA filter is as effective as two windows partly open all day during the winter (2.5-fold decrease in transmission). Two HEPA filters are even more effective (4-fold decrease in transmission).
Masks
Pre-Delta, we knew masks worked very well. Loose fitting masks, like double cloth masks, even still blocked 51% of particles. With Delta, though, we really need to start wearing better masks, especially those that are most vulnerable (i.e. unvaccinated). A Finland study found that Delta was transmitted among healthcare workers using surgical masks; it’s clear that N95’s work best in hospital settings where employees are constantly exposed to COVID-19.
A stimulation study that came out this week showed that, in classrooms, surgical masks reduce transmission 8-fold. Surgical masks have a great filter, but sometimes they are way too loose on kids. Fit and filter are very important with Delta. For great masks look for ASTM-certified surgical or tight-fitting cloth masks for kids. For fantastic masks, look for KN95 or KF94 made for kids. N95’s are not made for kids, so do not buy them for kids to wear; they don’t fit correctly. Dr. Eva Enns from the University of Minnesota School of Public Health put together an amazing list with specific kid mask brands here. Dr. Linsey Marr at Virigina Tech also made an amazing list here.
Outdoor transmission
There is no shortage of anecdotal evidence of outdoor transmission with Delta, especially in shoulder-to-shoulder activities like festivals. In Melbourne, two playgrounds and one skate park were exposure sites, which has fueled a stark debate about shutdowns in Australia. Importantly, these events seem to be largely crowded. Any time you’re close enough to breathe in air from someone else’s breath you have a chance of being infected. Being outdoors continues to be much less risky than indoors. Indoors can accumulate aerosols a whole lot more than outdoors. Think about it like smoking cigarettes. If someone is smoking cigarettes indoors, there is far more buildup over time than someone smoking outdoors.
Testing
With Delta, cases are going to happen in schools. Even if mitigation measures are in place. This virus is far too transmissible and contagious to not expect this. So, we need to identify cases proactively to stop the possibility of superspreader events. Schools need plans in place for testing, contact tracing, quarantining, and reporting. This includes supporting kids that are in quarantine through distanced learning. Your local health department will not have the bandwidth to do this, especially if you’re in a hotspot. There are great playbooks out there, though, to help guide testing strategies. Some states, like Texas, actually have frameworks. Rockefeller had a great playbook on this too.
Layered approach
The one thing that is incredibly clear is that we need a layered approach for Delta. Combined interventions (i.e., natural ventilation, masks, and HEPA filtration) are the most effective in schools (≥30-fold decrease in transmission). The more layers we have, the less chance virus gets through the Swiss cheese to your kid. This is an ever evolving landscape and we need to adapt and advocate accordingly.
Love, YLE
Next Tuesday night (August 31st at 830pm ET), I will be talking at a free event along side pediatricians Dr. Christina Johns and Dr. Eric Weinberg about Delta and schools. While we’re presenting, we have have an army of pediatricians answering audience questions in the chat; parents find this feature incredibly useful. I think last time the physicians answered more than 300 questions in real time. Sign up here if you’re interested in joining.








Have you seen the NYMag article “The Science of Masking Kids at School Remains Uncertain?” And if so do you mind addressing it/giving your thoughts? I’ve seen it shared a lot recently. Thanks!
One last comment- what is your analysis of this recent CDC paper- this scares the heck out of me. https://www.cdc.gov/mmwr/volumes/70/wr/mm7035e2.htm?s_cid=mm7035e2_w. THis school did everything in terms of mitigation, but a single infected teacher can still infect 12/24 kids who were wearing masks, with open windows, distanced and with a hepa filter, and only with occasionally taking his/her mask off.