Here's an update on the latest developments in public health: Avian flu and measles outbreaks, the end of the respiratory season, and mpox (monkeypox) brewing on the horizon.
Avian flu: risk remains low
Since the last YLE update, there have been a few important (and optimistic) insights into the current avian flu outbreak:
Lab results came in from a Texas farmer. CDC collected samples and posted results in a highly technical document. (Results were surprisingly fast, which is a nice change of pace.) Here is the plain language translation:
One mutation—PB2 E67K—was found in the virus that infected the farmer. A mutation in this spot indicates that the virus mutated to jump to mammals. This was expected.
There were no other surprising mutations, including no mutations that indicated an increased ability to spread human-to-human.
Antivirals and the H5N1 vaccines we have in a small emergency stockpile will still work. It’s unclear to what extent the seasonal flu shot will provide cross-protection.
Another state with infected cows. It’s time to add Ohio to the list, bringing the total to 15 dairy herds across six states. We will likely see more.
The virus is replicating in the udder. USDA tested cow’s milk, noses, and blood and found the most replicating virus in the udder. This means it’s likely spreading via milking machines, which would be easier to control than in the air. Also, the virus samples across cows look very similar, meaning this outbreak likely happened during one spillover event (from a dead bird).

Chickens are being infected. Two avian flu outbreaks in chickens have now been reported in Texas and Michigan. The largest producer of fresh eggs said it had temporarily halted production and is killing 1.6 million hens and 337,000 baby chickens. Avian flu has also been detected among cats at the farms.
Clinicians are on alert. The CDC warned physicians to be on the lookout for avian flu patients. I don’t know how necessary this is, given that the probability of this happening is small and isolated.
Economy vs. public health debate bubbling up. The wide geographical distribution of avian flu in such a short time period is concerning. It would be incredibly helpful to understand, at the very least, how this is spreading by testing livestock. However, the age-old battle between the economy (concerns about losing livestock exports) and public health (testing livestock) is igniting. I would strongly argue that a healthy economy depends on controlling avian flu.
Measles: Still heating up
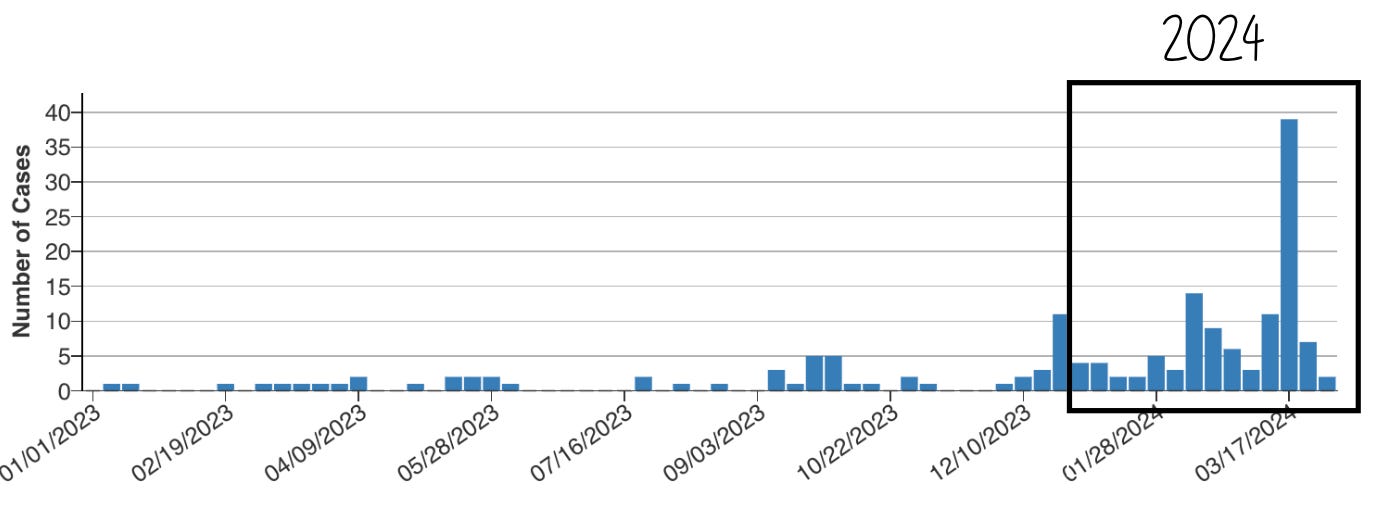
March was a big month for measles. We are up to 119 cases, more than double last year’s total.
CDC has finally started providing data on the severity of these cases:
95% of cases are among unvaccinated or under-vaccinated (only 1 MMR vaccine) people. This tells us that the vaccines are working.
58% of cases are hospitalized. This is high, as typically 1 in 5 cases are hospitalized. This may be inflated due to mandatory isolation, which can be done at a hospital.
The majority of cases and hospitalizations are among those under 5 years old.
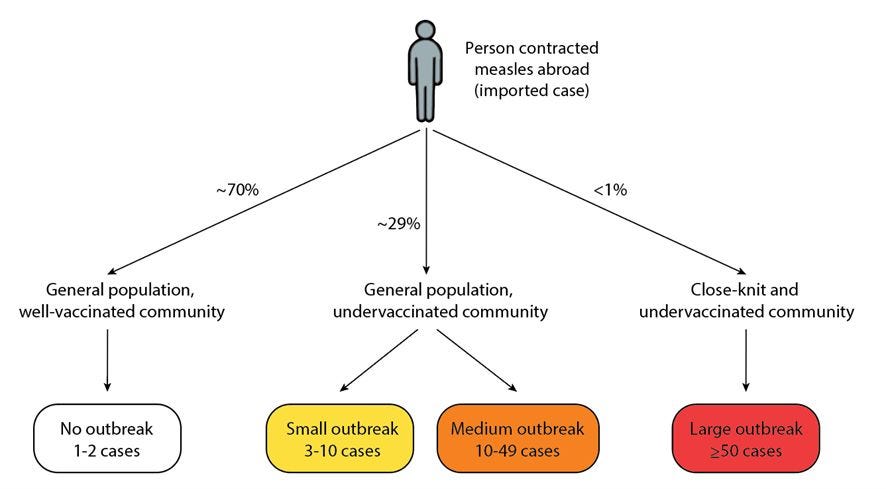
Communities can be categorized into three “groups” of risk, as displayed below. While most (70%) of communities have high immunity, 29% are susceptible to small and medium outbreaks. This means we will likely see more small outbreaks this year. The risk of a huge outbreak remains low, but it’s certainly possible.
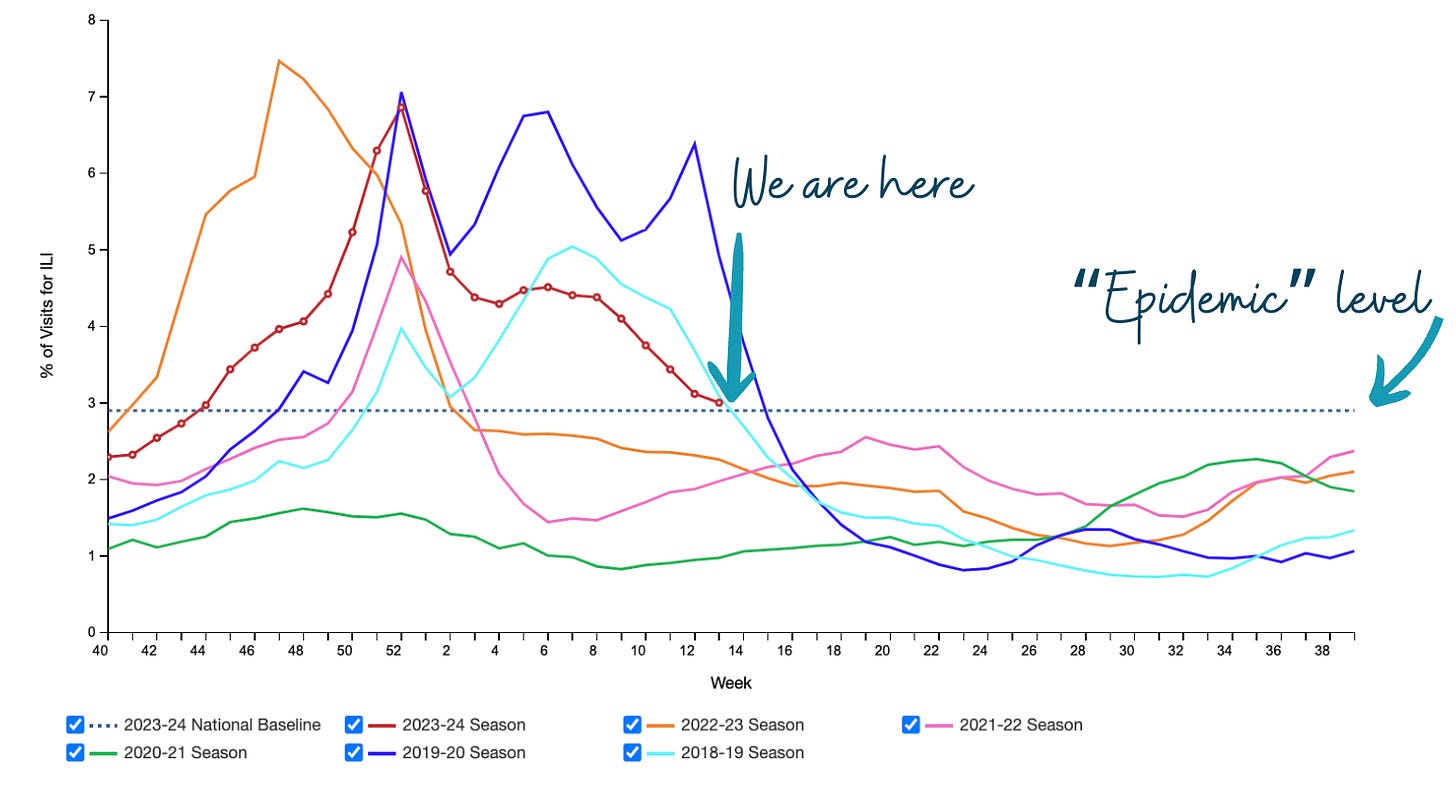
Respiratory season: (nearly) over
The number of people going to the doctor for cough or fever is declining quickly. We are almost at the epidemic-level threshold, which means the respiratory season is nearly over. This means I will no longer be masking. This season lasted about five months—on par with pre-pandemic years.
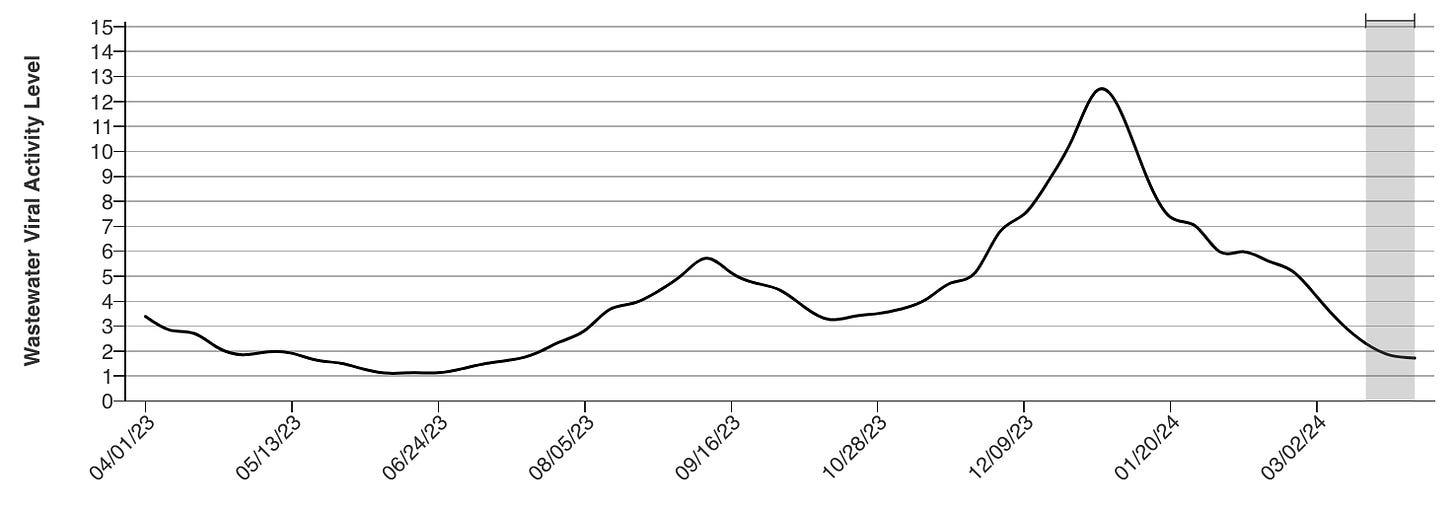
This also means that Covid-19 is nosediving, as seen in the wastewater below. It will likely be back this summer, as this has been the pattern for the past three years. Enjoy the lull for now.
Mpox: Bad DRC outbreak
Remember mpox (formally known as monkeypox)? Well, it’s starting to heat up again. The DRC (Democratic Republic of the Congo) is experiencing a massive outbreak. Importantly, this outbreak differs from the one in 2022 in three ways:
Different strain. The mpox strain causing this outbreak is called Clade I, which is typically more severe. In DRC, 1 in 12 patients are dying.
Transmitted differently. While there are some sexually transmitted cases, it’s also being spread in households, hospitals, and schools.
Kids are getting hit hard. About 2 out of 3 cases are children. And, among those dying, 9 out of 10 are under 15 years old.
The Clade I outbreak in DRC has been isolated thus far. However, this could easily change, particularly because this outbreak is among highly transient communities, testing is suboptimal given limited resources, and vaccines are largely unavailable.
Mpox in the U.S. is heating up, but these are Clade II cases (the less severe strain in 2022). This year we’ve had 664 mpox cases (compared to 307 cases last year).
This will be an important one to keep an eye on.
Bottom line
A lot is happening in the infectious disease world. There is nothing for you to necessarily do right now except keep up to date on vaccines. The government will certainly have to work on transparency, timeliness, trust, and, of course, preparation. Hopefully, we learned a thing or two from the Covid-19 emergency.
Love, YLE
Also, what about that total eclipse?! It 1000% exceeded my expectations; truly a mystical experience. I hope you were able to catch a glimpse. Science is so cool!
“Your Local Epidemiologist (YLE)” is written by Dr. Katelyn Jetelina, M.P.H. Ph.D.—an epidemiologist, wife, and mom of two little girls. During the day, she is a senior scientific consultant to several organizations, including CDC. At night, she writes this newsletter. Her main goal is to “translate” the ever-evolving public health world so that people will be well-equipped to make evidence-based decisions. This newsletter is free, thanks to the generous support of fellow YLE community members. To support this effort, subscribe below:






hi 👋🏼 long-time follower and new subscriber - curious if you’d share your rationale on dropping the masks and what indicators you’ll use to resume masking? I have a hard time gauging the absolute risk of covid with low wastewater levels like this so haven’t dropped the masks yet in my house. I’m terrified of the possibility of severe long covid but I’m also burning out on skipping out on seeing friends, important events, travel, etc. any advice?
The profile you provide for Clade I mpox is very alarming. Please keep us posted.