Well, we currently have three public health emergencies across the globe and in the United States: COVID-19, monkeypox, and polio. Here is a State of Affairs for all fronts. Buckle up.
COVID-19
In most countries, BA.5 is beginning to wind down. This is a welcome reprieve given that in the past four weeks we lost 62,892 people worldwide, including 15,100 Americans. Japan, however, is still getting hit hard and is experiencing the highest number of deaths since the beginning of the pandemic. Notably, Australia has had sustained, high rates of death during their winter season. Cumulatively, deaths in both countries remain far below the U.S., though.
In the U.S., all metrics (reported cases, test positivity rate, hospitalizations, and wastewater) remain high but have clearly peaked and well into their descent. This is happening in every region of the U.S.

What’s next? One Omicron subvariant, called BA.4.6, is taking hold in the U.S. It doesn’t have a mutation on the spike protein, but another mutation is giving it a slight advantage, causing a very slow take over. We don’t think this will cause a wave, but BA.4.6 may become dominant.
We continue to see SARS-CoV-2 mutate at a remarkable rate. Just like we watch weather patterns for hurricanes, we have mutation surveillance for SARS-CoV-2. Another Omicron subvariant, BA.2.75, is on the horizon. We are seeing in India and Australia that it can outcompete BA.5 and BA.4.6, but we don’t think it will cause a Category Four hurricane. It will likely take over in the U.S., but relatively slowly, causing a small blip on our radar. Another possibility is that, for the first time, we see two subvariants co-circulating at the same time. Unfortunately, global surveillance has decreased, and the number of sequences shared per week has fallen by 90% since last winter. This means we are largely flying blind as to what new variants are popping up and what we may see in coming months.
What happens next is also dependent on behavior, as this changes going into fall/winter (schools open, people head inside with cool weather, groups gather for holidays). This combined with humidity and waning immunity is largely why we see seasonal patterns of other coronaviruses and the flu. We think one day we will see seasonality with SARS-CoV-2, but it is not yet predictable.
The next month or two will likely be quiet on the COVID-19 end. This is especially true is a substantial amount of people get the Omicron booster (more on this in a future post). We will have to wait and see how COVID-19 takes us into winter months. This is quite difficult to predict; I’m holding my breath.
Monkeypox (MPX)
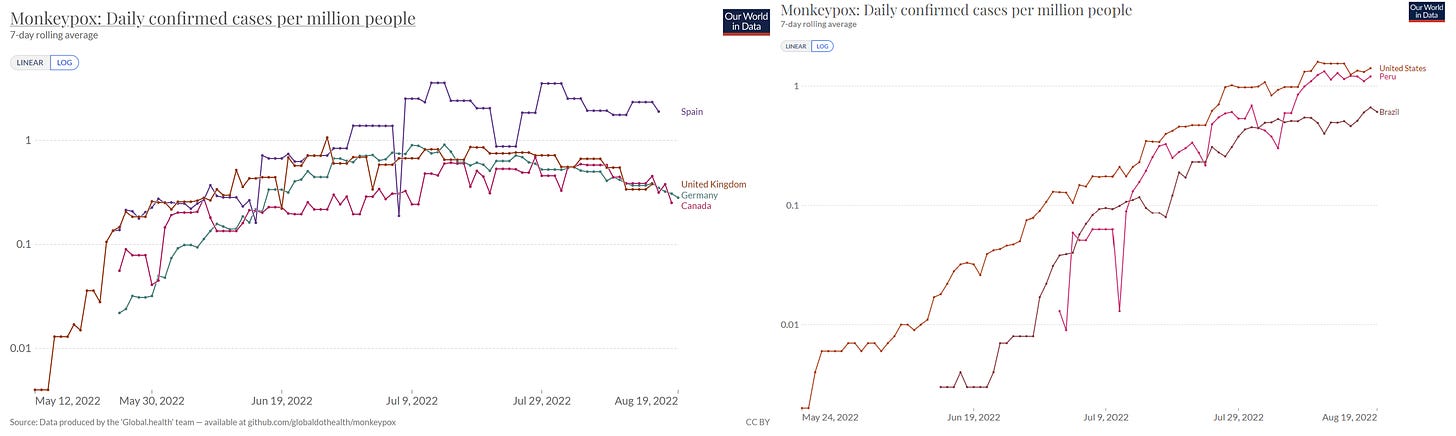
MPX is becoming the tale of two stories. Some countries have successfully slowed the virus, particularly in the U.K., Germany, Canada, and Spain. Other countries show continued acceleration, like the U.S., Brazil, and Peru. The latter two are particularly concerning given their high rate of untreated HIV. It’s no coincidence that Peru has had 1 death in 300 cases (which was someone with HIV) while the U.S. has had zero deaths per 14,000+ cases. The outbreak started later in these countries, so I’m hopeful deceleration is coming soon.
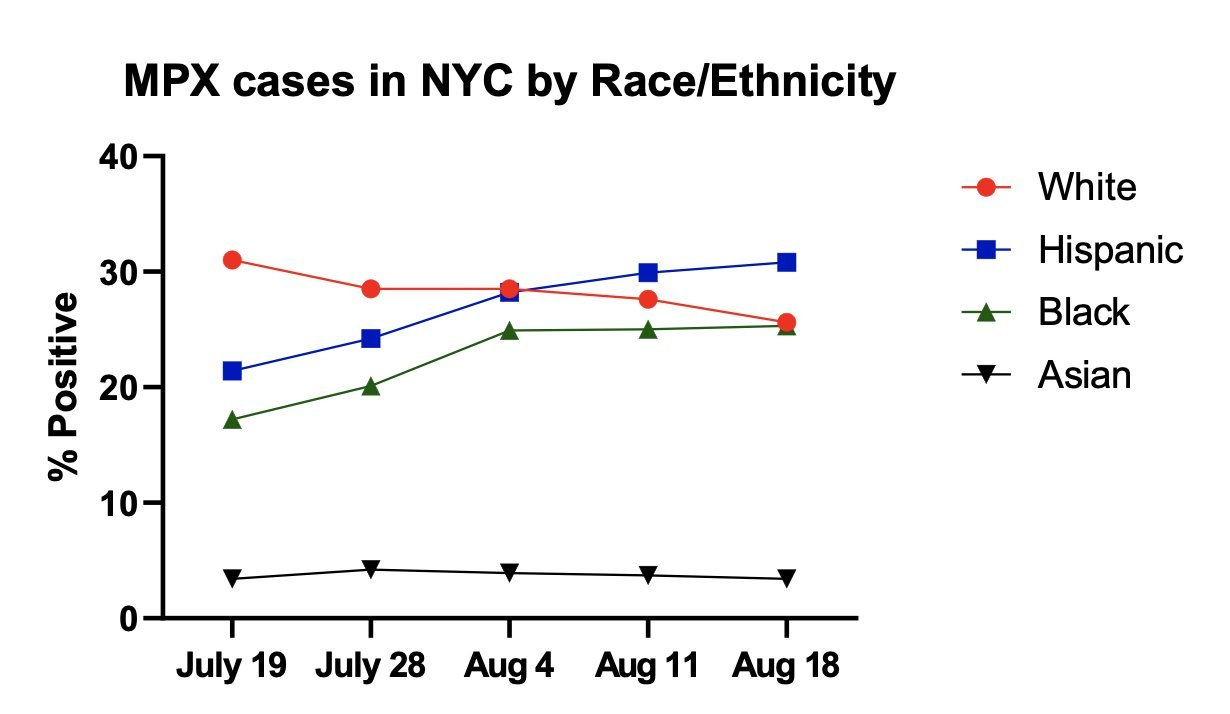
In the U.S., there are positive signs that MPX is slowing in specific cities and among specific groups. For example, cases in NYC seem to have plateaued. However, this is driven by a decrease in cases among non-Hispanic White people, as MPX cases among non-Hispanic Black and Hispanic people continue to increase. Unfortunately, Black and Hispanic people are disproportionately less vaccinated for MPX than White people. Health inequity continues to ravage our communities.
Vaccines, behavioral changes, treatments, and the blood, sweat, and tears of on-the-ground advocacy teams have directly caused the deceleration. We don’t know which factor, though, is the dominant driver of the change. This is important to know as it has implications for containment. For example, if deceleration is driven mostly by behavior change, MPX will be difficult to contain (as people will eventually go back to their normal behaviors). If deceleration is due to vaccines, containment would be more possible. We are still eagerly awaiting data on the effectiveness of the MPX vaccines.
Surveillance data from the U.K. shows that MPX continues to spread in one tight social network: men who have sex with men (96.7% of cases with data are men who have sex with men). But the latest report did note: “there does seem to be some increase in unlinked female cases. This is currently not significant at the 5% level but continues under close surveillance.” In other words, the numbers are not a concern yet but are creeping up. All eyes are on this signal to see if sustained transmission will extend beyond the current networks.
Polio
London and New York continue to show community transmission of polio. Wastewater surveillance shows polio has been spreading for months (if not longer), and we have detected numerous genetic strains. This means more than one individual is shedding polio virus; the outbreaks aren’t contained. This has prompted the U.K. Health Security Agency to recommend a polio booster for all children ages 1-9 years old in London. In NYC, this recommendation hasn’t come down yet, but I guarantee these conversations are happening behind closed doors.
Last week, the CDC published a deep dive on the young man with paralysis in NYC. The report soberly stated that “even one case of paralysis indicates a public health emergency.” This is because for every one paralysis case, there are hundreds of less severe infections (asymptomatic or flu-like symptoms).
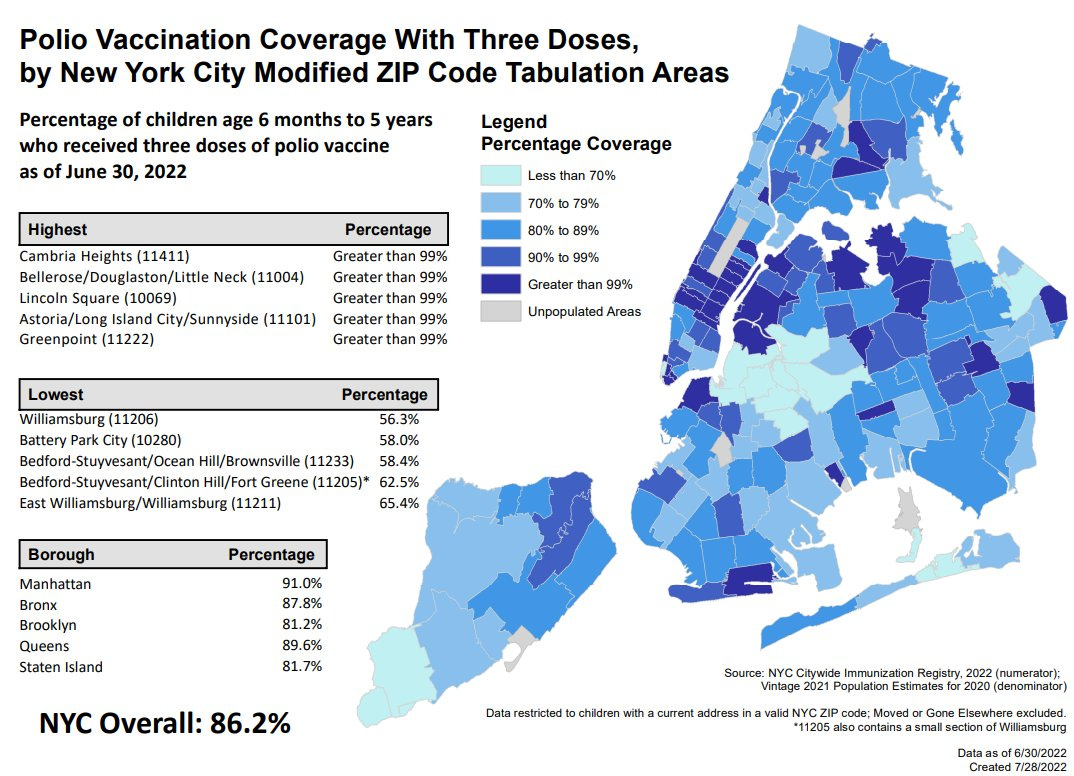
This is very concerning because there are substantial pockets of unvaccinated people. For example, in NYC only 86% of children are fully vaccinated for polio, and some counties, like Rockland County, dip down to a staggering 37% of children vaccinated. (WHO recommends a 95% vaccination coverage to control the virus.) We may see more paralysis cases.
If you and/or your child are fully vaccinated (which is either three or four doses, depending on state), you’re fully protected against polio paralysis. However, you can spread polio and possibly get flu-like symptoms. If you can’t remember if you were vaccinated or can’t find records, you should get vaccinated. Unfortunately, an antibody test will not tell you if you’re immune to polio, as other enteroviruses show cross-reactivity.
Bottom line
There is a substantial amount of disease spreading in our communities. This will likely get worse this winter. The best thing you can do is to keep up with all vaccinations. Also, spare a thought for your public health workers, as the past 2.5 years have been absolutely exhausting, and it doesn’t look like this will let up any time soon.
Love, YLE
“Your Local Epidemiologist (YLE)” is written by Dr. Katelyn Jetelina, MPH PhD—an epidemiologist, biostatistician, wife, and mom of two little girls. During the day she works at a nonpartisan health policy think tank, and at night she writes this newsletter. Her main goal is to “translate” the ever-evolving public health science so that people will be well equipped to make evidence-based decisions. This newsletter is free thanks to the generous support of fellow YLE community members.







Please, please continue to emphasize masking. The threat of severe disease is still significant for some populations, and long Covid remains a real risk.
Katelyn, I had the Salk injection and the attenuated virus on the sugar cube as a child.. Do ypu feel that I am probably protected against paralysis, or do you feel that I should get the current polio vaccine series? Also, had scratch smallpox vaccine as a child. Do you feel that I am protected against severe monkeypox? I am 75. Please address these questions. Thank you for all you have done to educate as all.