I was hoping for a relatively quiet week. But, as with a lot of people right now, SARS-CoV-2 finally caught up with my little family. I finally got a break at our “hot mess express” house to get a handle on the current state of affairs. This is where we are today…
CDC guidance changed
The biggest news this week was that CDC changed their isolation policy. Their new guidance includes a reduction in the isolation period after a positive test from 10 days to 5 days for asymptomatic individuals regardless of vaccination status. They also changed the quarantine period to 5 days after exposure. Importantly, though, they recommended wearing a mask for 5 days after isolation and quarantine.
The CDC said they changed this due to changing scientific evidence: “The majority of SARS-CoV-2 transmission occurs early in the course of illness, generally in the 1-2 days prior to onset of symptoms and the 2-3 days after.”
I, like many other scientists, have many reactions to this guidance. For what it’s worth, here are some of mine:
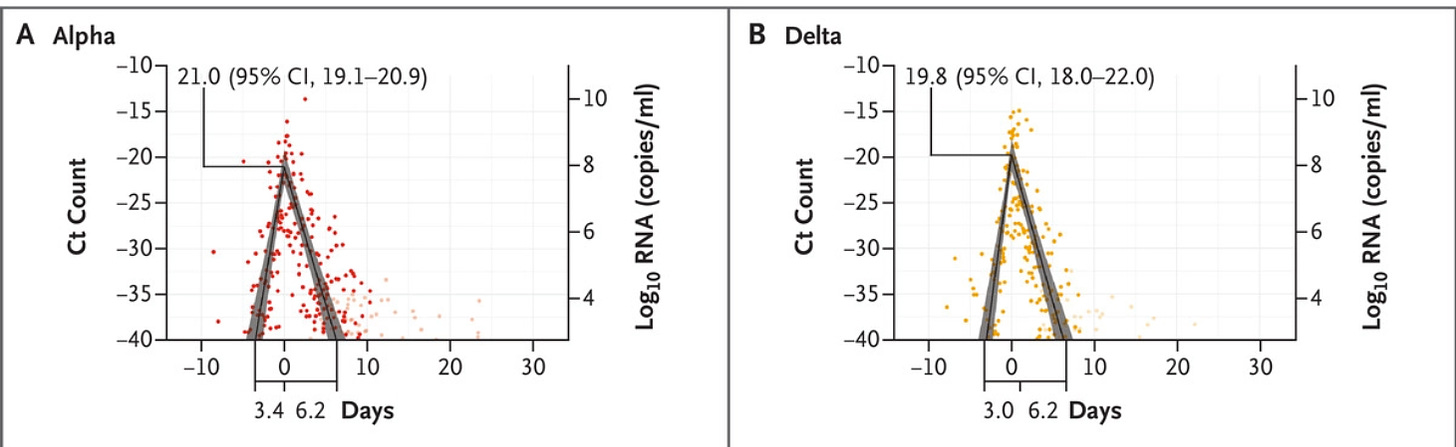
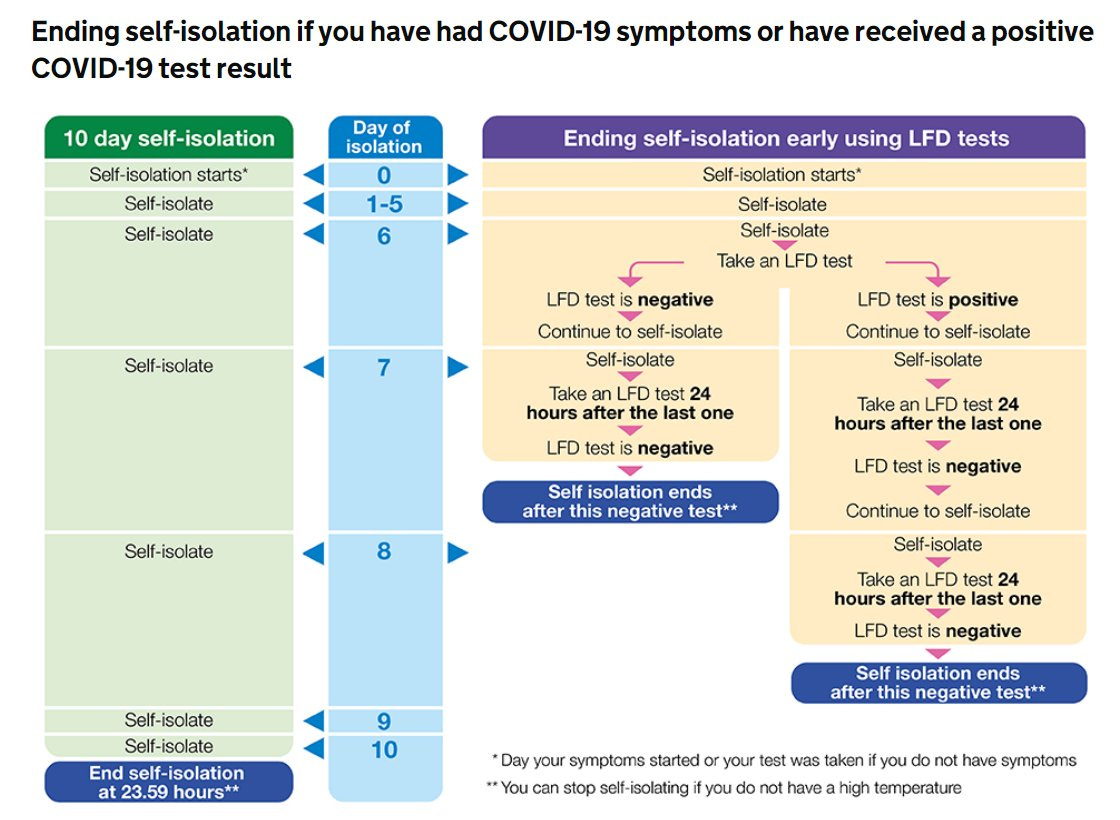
What is the evidence? The CDC didn’t provide the scientific evidence backing their decision, which was incredibly disappointing. If I were in the room, I would have depended on four seminal studies published (here, here, here, here) before Omicron. Together the results suggest a broad range of an infectious period ranging from 3-9 days. One of the studies displayed this data nicely below. In short, the viral load increased to an infectious rate (Ct~32) about 2 days before symptoms until about 4-5 days after symptoms.
Importantly, this range is very different for vaccinated compared to unvaccinated people. On average, viral clearance is about 5.5 days among vaccinated compared to 7.5 days for unvaccinated people (see figure below).
So, the majority of vaccinated people are well on their way to clearing the virus at 5 days. This is especially true among asymptomatic people. Some vaccinated may still have the virus, but if they wear a mask they won’t contribute to an overabundance of spread. The CDC policy makes sense for vaccinated people, at least before Omicron.
Unvaccinated people clear the virus in 7.5 days, which is obviously higher than the 5-day clock with this guidance. Even more worrisome is the broad range of infectious periods for unvaccinated, which ranged from 2 to 14 days (see panel G below). This new guidance may not be a problem if the unvaccinated actually wear a mask 5 days after isolation like this guidance suggests. But I doubt this will happen. The CDC stretched the science for unvaccinated people too far.
Does this policy make sense for Omicron? Importantly, the aforementioned studies were conducted before Omicron. We do not know how Omicron changes viral clearance. A study today found Omicron’s incubation period is faster than before. So, one could postulate that if symptoms arise faster, people test quicker, and their “5-day clock” starts sooner. If viral clearance with Omicron is the same as Delta, then this policy change could lead to significant community spread because people would leave isolation while contagious. The CDC may have evidence (and I sure hope that they do) that Omicron is cleared faster, but it hasn’t been publicly shared yet. This information is critical.
No testing? It’s incredibly odd to me that the CDC decided not to end isolation contingent on a negative antigen test (or better yet two). The viral load (like the studies I mentioned above using “Ct” measure) is not the same thing as contagious virus. Past studies have shown that some people stop shedding live virus very fast. But other people, especially unvaccinated, shed live virus well past 5 days.
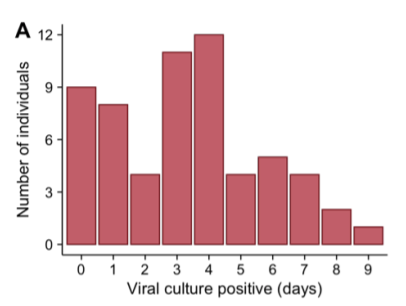
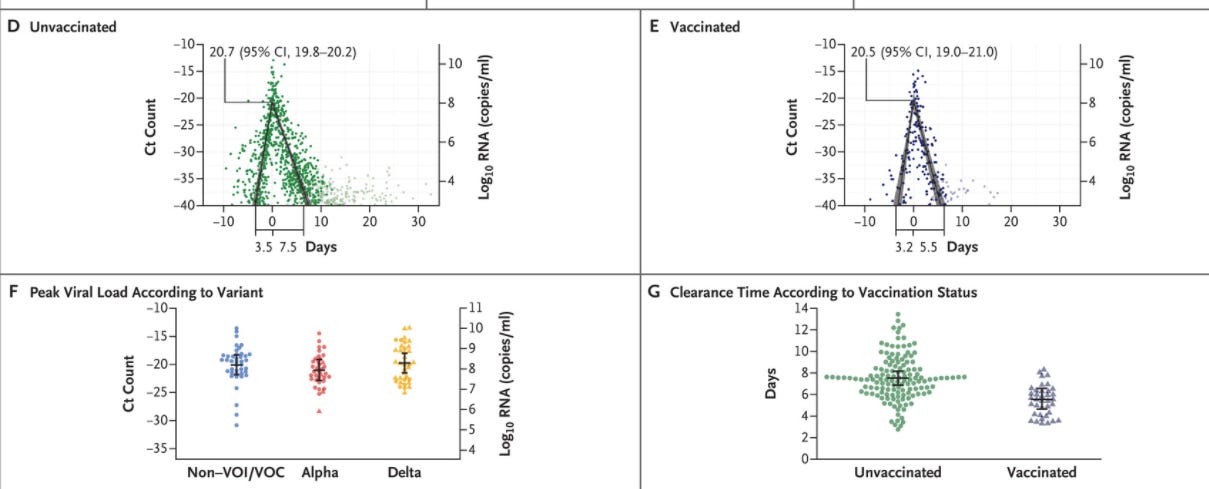
Figure A: The distribution in the numbers of days in which participants tested positive by viral culture on nasal swabs following study enrollment. Ke et al. Study here I’m guessing this decision was based on our abysmal testing supply in the United States. But this is an artificial problem created by not prioritizing rapid antigen testing. This can be fixed. If the CDC put a testing stipulation into place, I’d be far more comfortable with their policy. (For the record, the UK actually has very similar guidance as the CDC guidance, but does require two negative antigen tests. See their policy below.)
I don’t envy policymakers trying balance science with politics and the economy. One thing that the CDC does consistently well is stick to the evidence. (Some would argue they stick to evidence too much resulting in a reactive instead of proactive response.) However, the CDC hasn’t provided this evidence. And the CDC continues to fail on implementation. Guidance based on an honor system crumbles. So, if you’re positive, please use an antigen test to get you out of isolation. If you can’t continue in isolation (because of your job or school), please wear a very good mask.
Prevalence of Omicron changed
The other thing that the CDC changed this week was the prevalence estimate of Omicron in the United States. Previously, the CDC estimated a 75% prevalence of Omicron for the week of Dec 18. Today they changed that estimate to 22% on Dec 18. 22% vs. 75% is a huge difference! I’m shocked that the CDC was off about 1.5 weeks from their estimates. That’s a big error.
We expect these estimates to change a little from week to week. That’s because there’s a 6-week delay with genomic surveillance—it takes time for our tests to be sent to labs to verify the variant type. Because of that delay, the CDC presents projections or “guess-timates” (indicated by the asterisks on the top of the graphs). So, these numbers are meant to change a little. But they aren’t meant to change a lot.
Nonetheless, it looks like Omicron continues to displace Delta: While the number of Omicron cases increase, the number of Delta cases decrease. To corroborate the “real world” data, a lab study this week found that those infected with Omicron can neutralize Delta. In other words, those infected by Omicron are protected from Delta. This is really good news, especially if Omicron is milder than previous variants.
Cases
It’s clear that Omicron is spreading rapidly. Unfortunately, we don’t know the true case numbers right now. We’re flying blind due to disruptions in reporting, testing, and people’s behaviors around the holidays. For example, yesterday the United States reported 472,112 cases due to a backlog. We won’t know the true picture for a week or two.
We also don’t have a good grip on how the increasing popularity of antigen tests are going to change our trends either. Not all of those who test positive for antigen are going to go get a PCR, and these cases will go unreported.
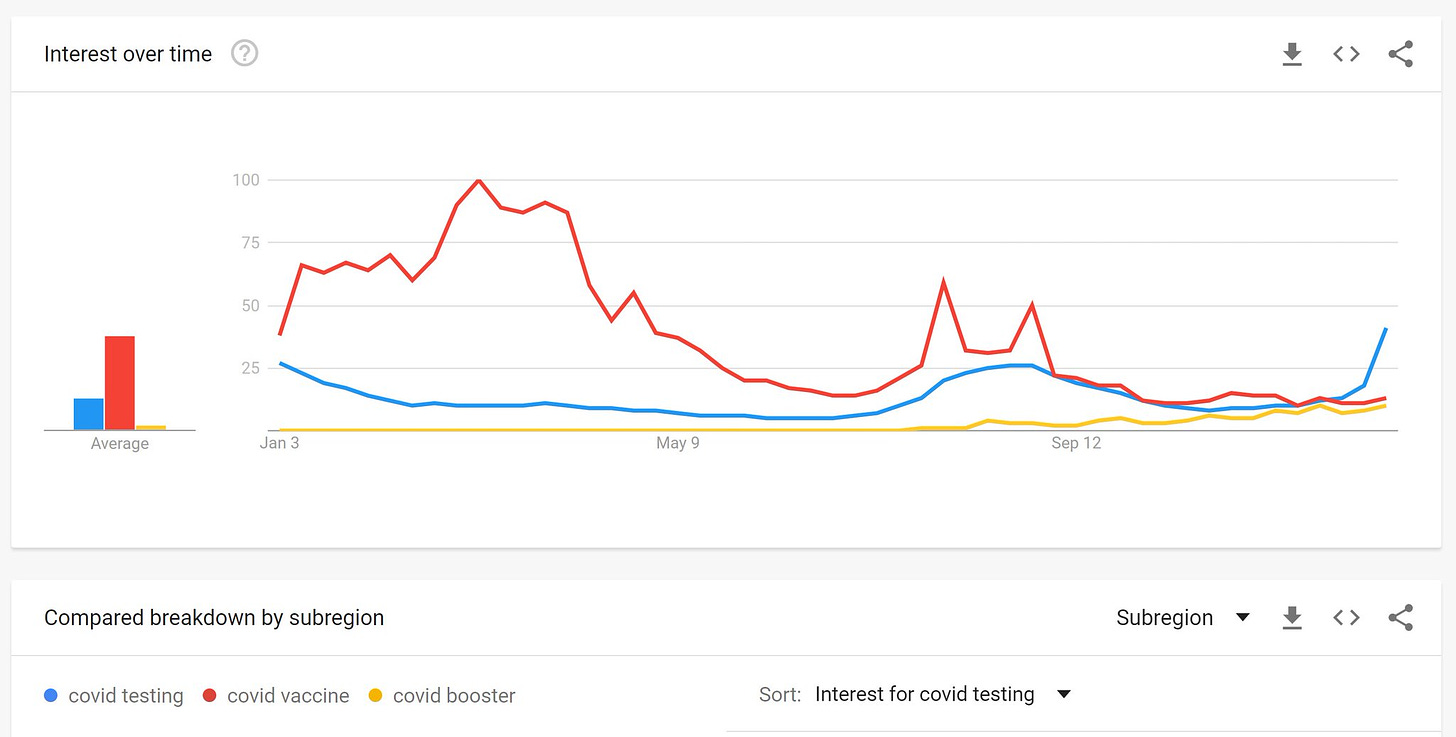
But we do have anecdotal evidence that more and more people are testing: empty store shelves, long testing lines, and, interestingly, in the Google data. The word combination “covid testing” is trending higher than “covid vaccine” or “covid booster” for the first time during the pandemic.
Hospitalizations
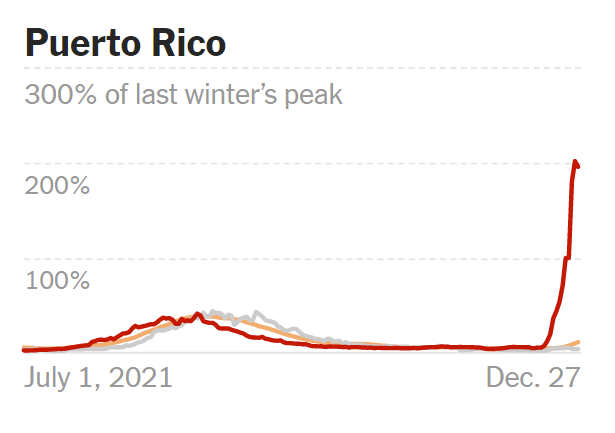
The holidays shouldn’t have a large impact on our hospitalization trends, though. The United States continues to see the decoupling phenomenon we saw in South Africa: Hospitalizations continue to be a fraction of cases thanks to immunity (and maybe because Omicron is less severe too). This is most apparent in Puerto Rico, which has one of the highest vaccination rates in the United States (77% fully vaccinated).
We’re also seeing this decoupling phenomenon in other States, like DC, New York, Illinois, and Florida.
However, even with this decoupling, some states still have very high hospitalizations. For example, Ohio hospitalizations are 105% of what they were for last winter. Even with the availability of vaccinations, hospitals are just as full as last winter.
It does seem clear that those in the hospital continue to be the unvaccinated. The state of New York is doing a great job keeping track of this. But this too is a bit delayed.
Unfortunately, the unvaccinated includes kids. This week the New York State Department of Health released a health advisory warning of a 4-fold increase in pediatric hospitalizations associated with COVID19. Specifically, they said:
Half of the admissions were kids <5 years of age
No 5-11-year-olds who were admitted to the hospital due to COVID-19 were fully vaccinated
23% of 12-17 year-old patients (7 patients out of 30 admissions) were fully vaccinated (compared to 64% fully vaccinated in that age group overall)
We’re seeing a rise in pediatric hospitalizations in the UK too. This shouldn’t come as a surprise because we saw this in South Africa, too. But South Africa found that this is not because Omicron is more severe for kids. Rather it’s a reflection of high community transmission; a wave that is sweeping up all unvaccinated, including kids.
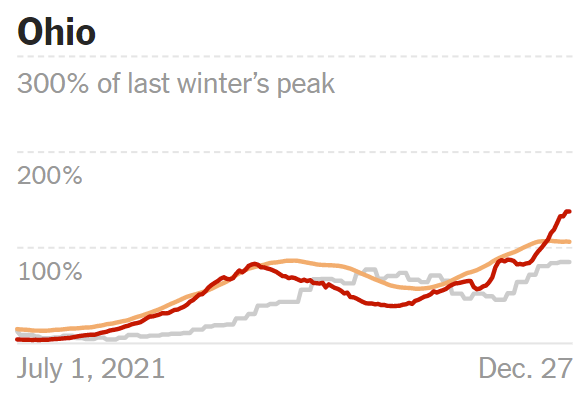
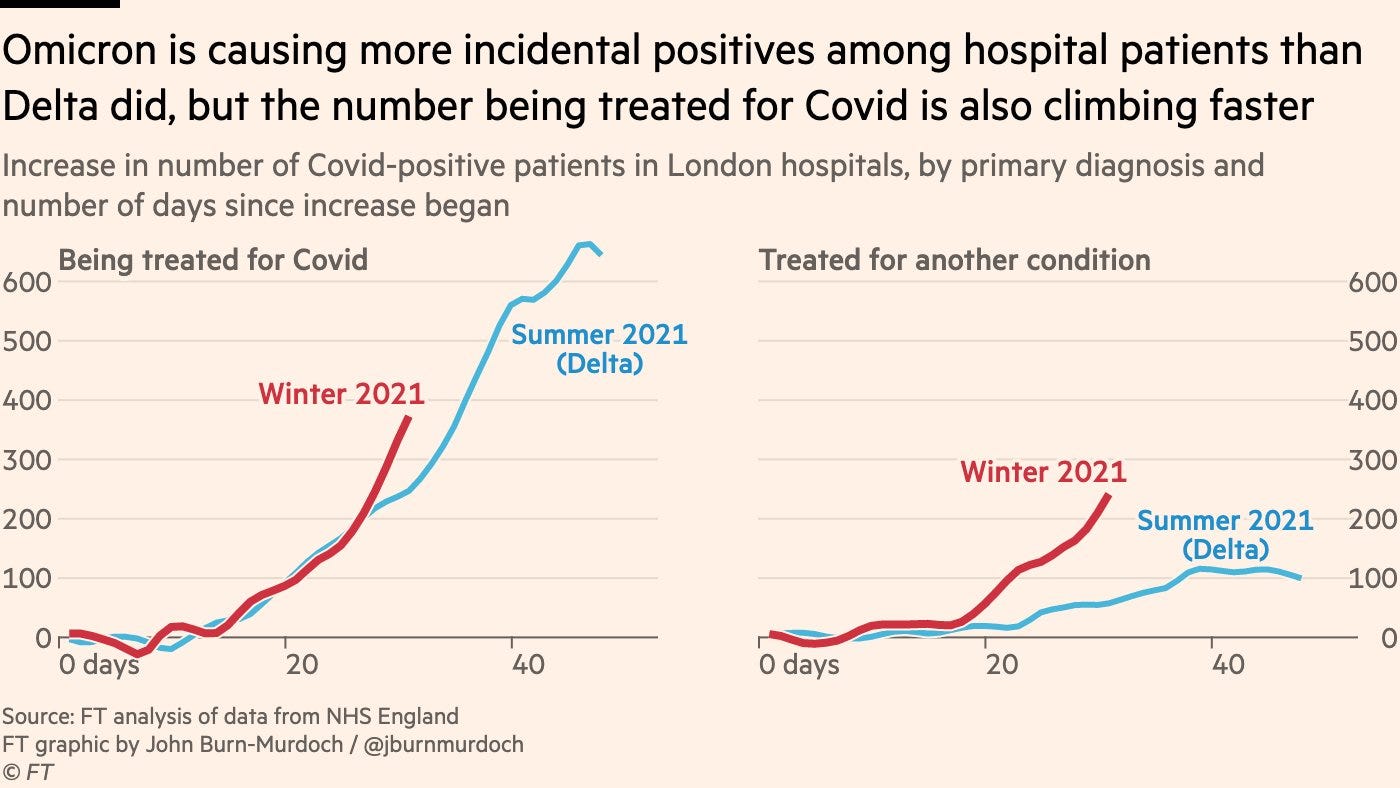
One thing we do not have a good grip on is the rate of hospitalizations “with COVID19” vs “for COVID19” for kids or adults. Across the pond, the UK tracks this metric on a weekly basis. In the latest report, hospitalizations due to COVID19 (left graph) is increasing, but so were hospitalizations among people “with COVID” (right graph).
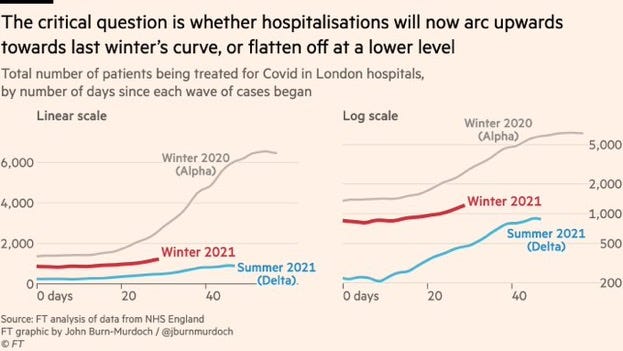
All eyes are really on whether the Omicron wave will reach the hospital system strain of last winter. In the UK, this doesn’t seem to be the case yet; hospitalizations with Omicron are tracking in-between the Delta (summer 2021) and Alpha (winter 2020) hospitalization trends. It’s critical to continue to watch this trend in the UK and the United States.
Bottom line: While case data continues to catch up from the holidays, hospitalization data gives us a good picture of how hospital systems are holding up. Hospitalizations in some states may start getting dangerously high (if they’re not already). Please do you part if you’re positive: isolate, mask, and test…if you can get your hands on one.
Love, YLE
“Your Local Epidemiologist (YLE)” is written by Dr. Katelyn Jetelina, MPH PhD— an epidemiologist, biostatistician, professor, researcher, wife, and mom of two little girls. During the day she has a research lab and teaches graduate-level courses, but at night she writes this newsletter. Her main goal is to “translate” the ever-evolving public health science so that people will be well equipped to make evidence-based decisions, rather than decisions based in fear. This newsletter is free thanks to the generous support of fellow YLE community members. To support the effort, please subscribe here:








First, thank you for your work. You have become an essential info source for me. Please don't take what I'm about to say too badly. From where you are, you can't see what's happening the UK. You can only see what gets published about it.
I live in England adjacent to Wales. Some of my view of the NHS is from family and friends who work in it.
From across the Pond, it may look to you like our NHS is not close to capacity because our case rate isn't as high as it got last year. You may not be aware that the NHS does not have the resources it had in earlier waves. Notice I said resources, not funding. We do not have all our health care workers (HCWs) any more. Many are ill or have been left disabled (and unable to do their work) by the remarkably high incidence of Long COVID or have been exhausted to the point of taking early retirement or resigning or committing suicide. Remaining HCWs seldom have access to the higher grade face masks now being recommended by many experts to fend of Omicron.
Our government said to carry on, dropped nearly all COVID measures 19 July, even told us this month to go ahead with holiday parties. But children under age 12 are unvaccinated. Schools are open with no masks in classrooms, no ventilation improvements (our ventilation is often poor), fully packed classes, no remote teaching any more, and prosecution of parents who try to keep their children out (as some clinically extremely vulnerable friends are trying to do in self-defense). So children get it (often half or more of a classroom at a time), an entire household gets it from each of them, and then everyone they interact with gets it.
People often take lateral flow tests before events and only attend if their result is negative. The false negative rate for those tests is relatively high. With previous variants, one false negative might result in a few people at the event getting COVID. Now, it is common for one false negative to result in all or nearly all attendees getting COVID from an event of just a couple of hours. Our prevalence rate is so high that if you have a gathering of, say, 40 people, statistically you must expect at least one attendee to have the virus.
Some examples of impact on the NHS? The entire Appointments team for a certain hospital was taken out by COVID from their holiday party, despite everyone's LFT being negative beforehand. A hospital tried to force admin staff to feed patients with no one properly trained available to turn to if something goes wrong such as a patient choking. Admin staff are as overworked as clinical staff, so that didn't fly. They're now using untrained volunteers. Even with non-urgent care cancelled, there aren't enough trained HCWs.
Hospitals are not the only part of the system at an extreme. The average wait for an ambulance for a heart attack or stroke was 55 minutes just before the distortions of Christmas break. That's supposed to be just a few minutes. For other critical health matters, it is now common to wait 4 or 5 hours for an ambulance, and then for the ambulance to wait as much as half a day before being able to transfer the patient into A&E (Accident & Emergency). For those who do get hospital care, there aren't enough home health care workers, partly due to COVID and partly due to Brexit. As a result, patients often cannot be discharged when they are ready because they can't be provided with enough support to get by outside the hospital. That blocks beds, which has ripple effects all the way through to ambulance availability.
The NHS is held together by the sheer willpower of those who remain able to work in it. The bit of help from the military is nowhere near enough. Outside the government, the surge of workload shaping up for January after holiday gatherings looks like it will be disastrous.
Dr. Jetelina, thank you. Thank you for digesting all of this information into bites for everyone to understand. I am a Registered Nurse with nearly 20 years critical care and flight nursing and having undergone the H1N1 epidemic and now COVID 19. Your work is important and valuable. As I live in a rural part of Idaho, the pandemic has not "hit here" yet. No masks, vaccination rates are horrendous, it's all a hoax, etc., despite the medical community begging people to heed their advice. The devil is always in the details and for me that is stats, but meaningful and understandable stats - which you provide. While I'm feeding the resident cow, myriad roaming sheep and goats, a flock of pigs, I think about the items you post and the relevance to our community. I wish there is a way to harness your knowledge and expertise to convince the reluctant many to heed the advice. Thanks for all you do and know you impact our medical world.