The dreaded and much anticipated triple-demic is finally here—for the first time RSV, flu, and COVID-19 are rising together. And it’s not looking pretty. Here is the current state of affairs.
Overall
Every Friday the CDC updates their “influenza-like illness (ILI)” data. This is a database in which providers tally patients that presented with ILI—a fever and a cough and/or sore throat—at their office. So these numbers include everything (flu, RSV, COVID-19, etc.) and are a general indication of the climate of respiratory of health in the United States.
Last Friday Twitter covered my reaction to the latest data pretty clearly: Holy crap. There are a lot of sick people in the United States right now.
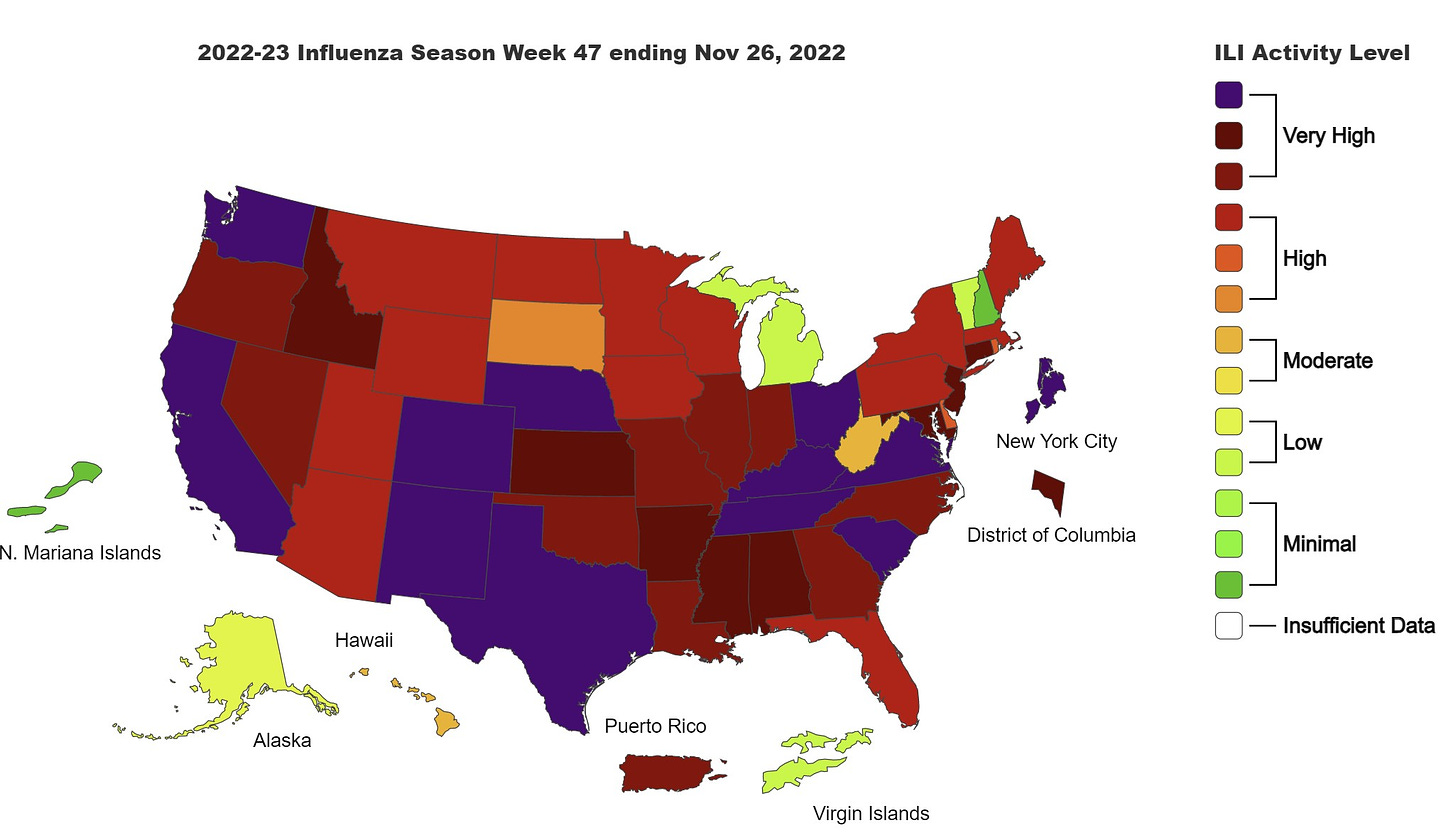
This level is truly unprecedented; we’ve never seen such high levels of ILI activity at this time of year. The map above is typically green (see below for this time in previous years). In fact, notice that before 2019, we didn’t even have the dark red/purple colors.

Yesterday, the CDC Director said: “hospitalizations are the highest now than they have been in the past decade.” This is truly concerning given a backdrop of burnt out healthcare workers and low staff levels.
While ILI surveillance gives us a picture of symptoms overall, we do have some (imperfect) surveillance for specific diseases.
RSV
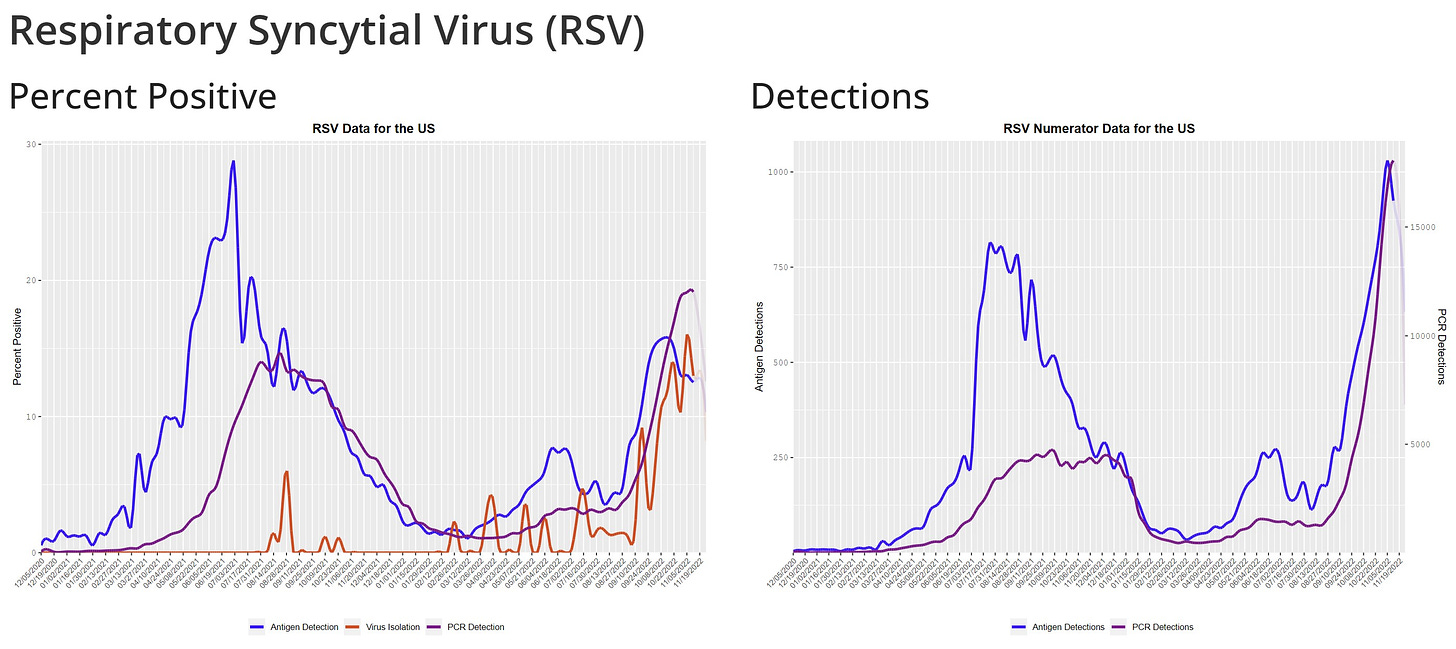
RSV continues to rise. We may be seeing the first signs of peaking on a national level (bottom right graph). This is expected given that test positivity rates have already clearly peaked (bottom left graph). There are certainly regional differences, as the South has clearly peaked (at least so far—Thanksgiving activity may change this) and West hasn’t slowed down yet.
Flu
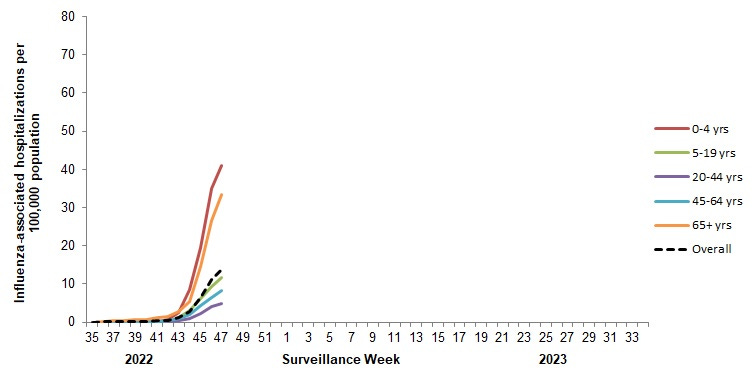
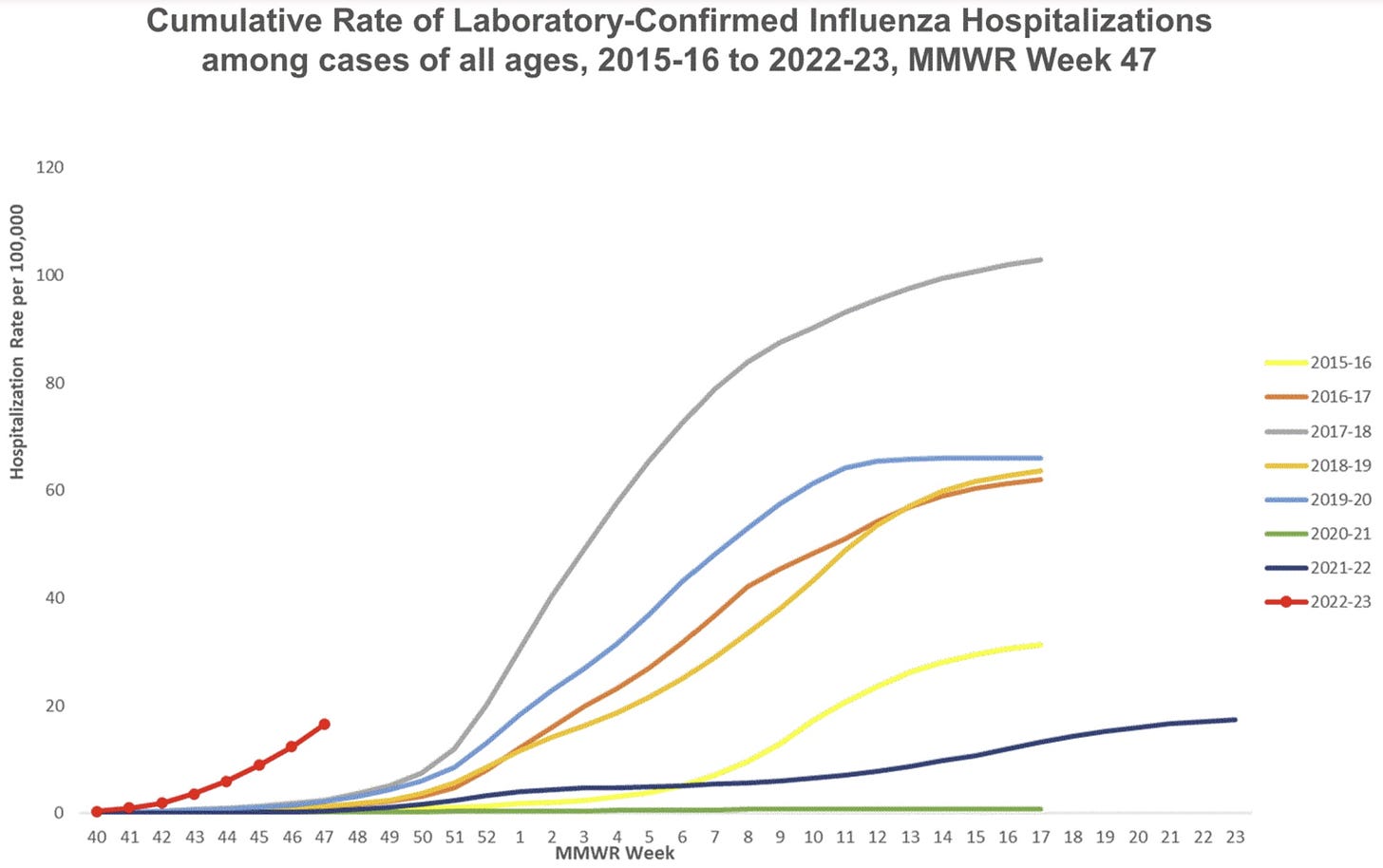
Flu cases are increasing and increasing fast. Flu hospitalizations are lagged (much like COVID-19) but increasing. Flu season outbreaks typically start in schools (hitting healthy children). Then the virus takes time to get to older adults. We expect hospitalizations to continue to rise in weeks to come.
In Canada, hospitalizations by age are clearly tracked. The highest risk for hospitalization is in those under 4 years old and those over 65 years. This likely reflects U.S. patterns, too.
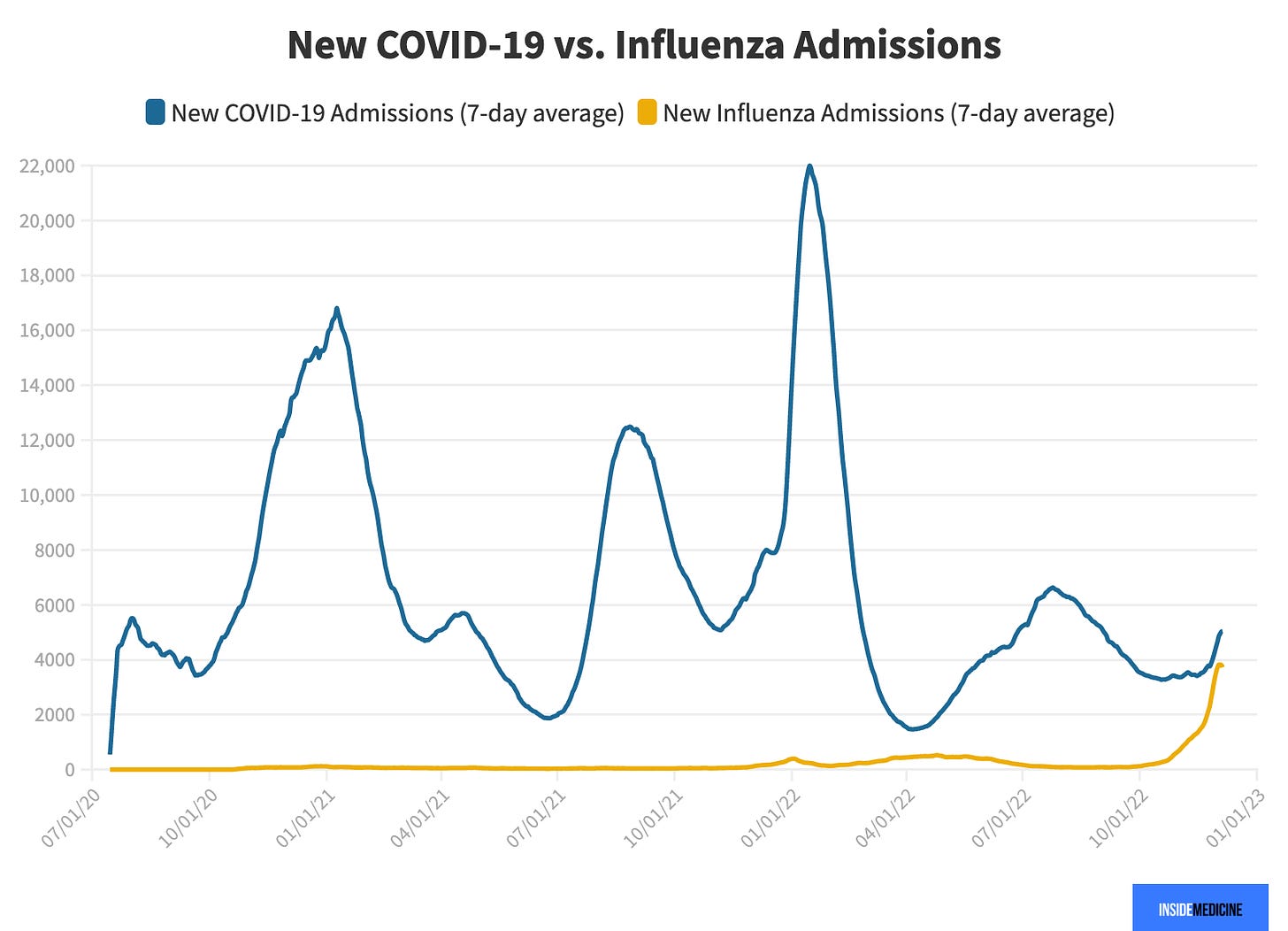
As Inside Medicine reported, for the first time during the pandemic, flu hospitalizations overtook COVID-19 hospitalizations last week. This may be a one-off occurrence since COVID-19 hospitalizations are increasing now, too, but it is noteworthy.
We don’t know if this will be the “worst flu season we’ve ever seen.” The Southern Hemisphere (Australia specifically) had a high number of flu cases but moderate levels of hospitalizations. Epidemiologists are crossing our fingers that this is what the Northern Hemisphere will see, too.
COVID-19
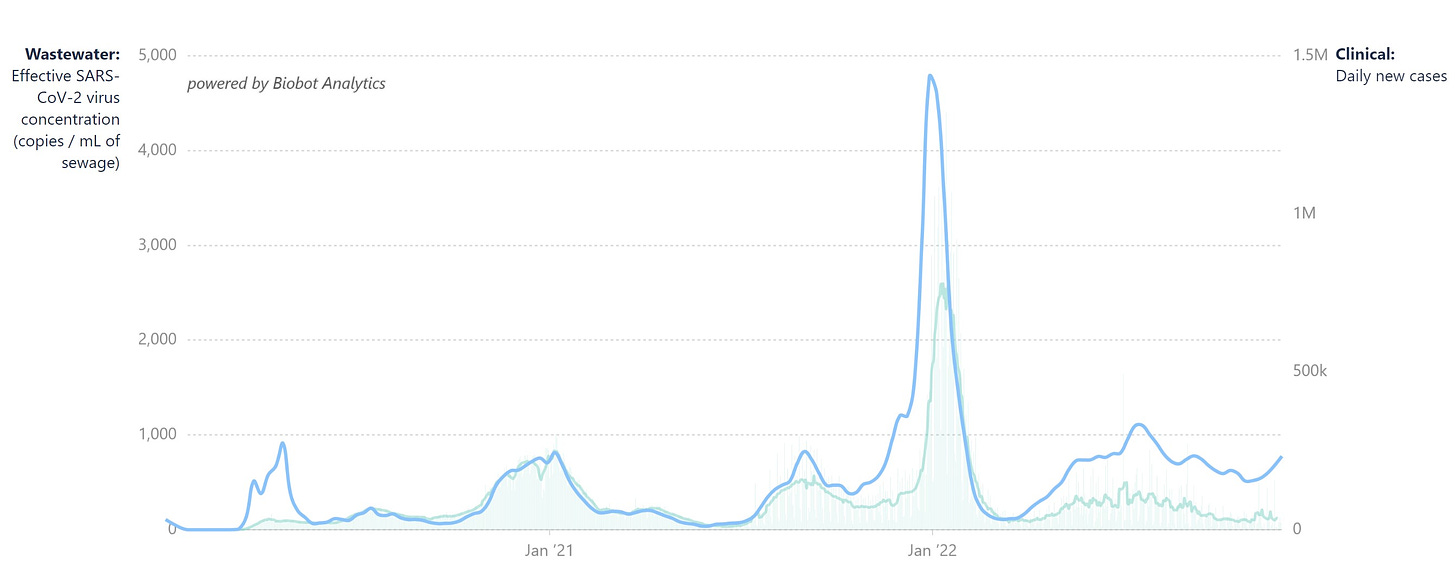
COVID-19 is on the rise across the globe due to the combination of seasonal changes, behaviors changes, and the variant soup. In the U.S., all signs point to the beginning of a wave. For example, SARS-CoV-2 in wastewater is rapidly increasing across all regions.
One major concern is the rapid rise in hospitalizations among older adults, which has exponentially increased 28% in the past two weeks. In many states, like California, the rate of hospitalizations is higher than the BA.5 wave, BA.2 wave, and/or Delta wave.
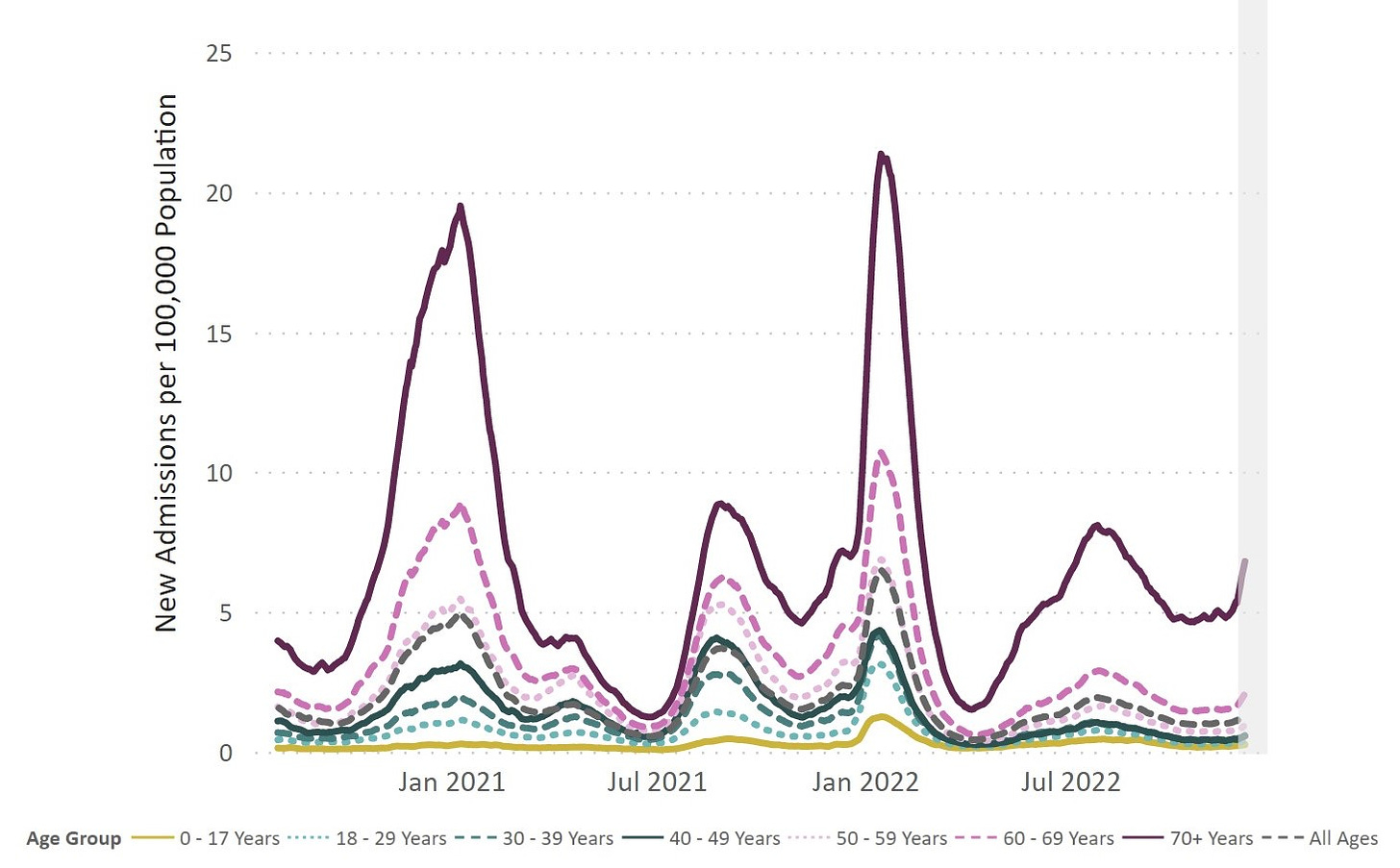
This is partly (or wholly) due to abysmal vaccination rates—only 1 in 3 adults over the age of 65+ have their fall COVID-19 booster. A public health failure. Without a recent booster, many people are technically vaccinated but not protected. I appreciated a recent U.K. public health campaign displaying the best messaging I’ve seen thus far.

Thanksgiving was 1.5 weeks ago, and because of it, many social networks expanded, providing new opportunities for viruses to spread. For COVID-19, it takes about ~2 weeks to see the epidemiological impact of holidays. The recent COVID-19 uptick may be partially explained by a “Thanksgiving effect,” although we are seeing an uptick in other countries that don’t celebrate Thanksgiving. I expect Thanksgiving will springboard us into more RSV and flu, too, but this surveillance is delayed.
Bottom line
This viral season is like no other. I’m running out of adjectives to describe it. (Unprecedented. Worrisome. A pain. Exhausting.) Unfortunately, we don’t know how long this will last or how bad it will get. I’m especially concerned for hospital systems, kids under 5, and adults over the age of 65, as they are at highest risk.
There’s a lot we can do: mask, test before seeing loved ones, get that airflow moving, stay home when you’re sick. The least you can do for a healthy season is get a flu and fall COVID-19 booster. If you haven’t gotten one yet, it’s never too late.
Love, YLE
“Your Local Epidemiologist (YLE)” is written by Dr. Katelyn Jetelina, MPH PhD—an epidemiologist, data scientist, wife, and mom of two little girls. During the day she works at a nonpartisan health policy think tank and is a senior scientific consultant to a number of organizations, including the CDC. At night she writes this newsletter. Her main goal is to “translate” the ever-evolving public health science so that people will be well equipped to make evidence-based decisions. This newsletter is free thanks to the generous support of fellow YLE community members. To support this effort, subscribe below:






Thanks for another informative newsletter! As a public health professional who's lost faith in the CDC over its COVID-19 response and frustrated with how hard it is to find the latest reliable science, I take comfort in reading your newsletter as a trusted one-stop shop. My family still masks in public, is fully boosted, avoids indoor dining when possible (except at school), and tests before we gather indoors with anyone outside our household. In the past two weeks, my partner and one of our four kids had COVID-19. There's growing exhaustion among some in the household about continuing with what they feel are futile prevention measures. I'm still of the belief that we need to continue with prevention for our own sake AND public health. One personal motivator has been avoiding long term health issues associated with COVID-19. It would be helpful to hear your thoughts and the latest evidence on long term health issues stemming from COVID-19 infection. As time goes by and variants emerge, is the data showing we should be more or less concerned at an individual level for someone who is otherwise healthy and fully vaccinated?
I feel this in the primary care office, where it’s like running parallel jobs - one where I’m seeing patients, and the other where my inbox is getting flooded with messages/calls that need attention, many for Covid and Flu.
Oh, and my hospital system warned us that there is a severe national shortage of Tamiflu developing.
Would be nice to have some leadership step up and call for masks until Santa comes, politically poisonous as that might be.