Happy spring! With warmer weather comes a calming of the respiratory season. Hopefully. Viruses are definitely still circulating, but we are seeing some encouraging signs.
A look back
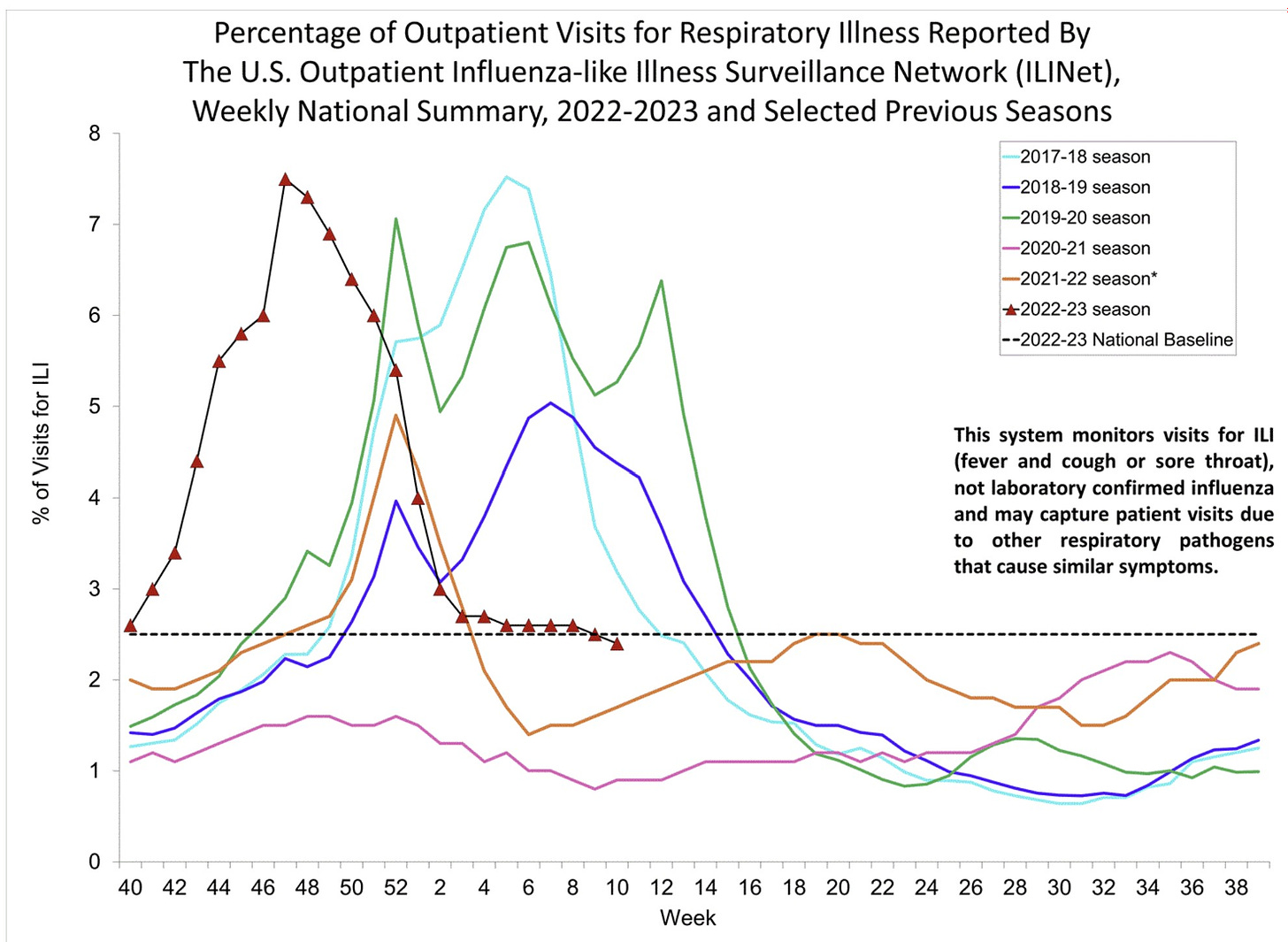
Doctor visits for fever and a cough (i.e., “influenza-like illnesses” or “ILI”) were back to pre-pandemic levels this season, but had some uncharacteristic patterns:
Shifted to earlier in the season;
Descended as quickly as it ascended (ILI usually peters out);
Stalled just above epidemic levels for weeks.
ILI just dipped below epidemic levels.
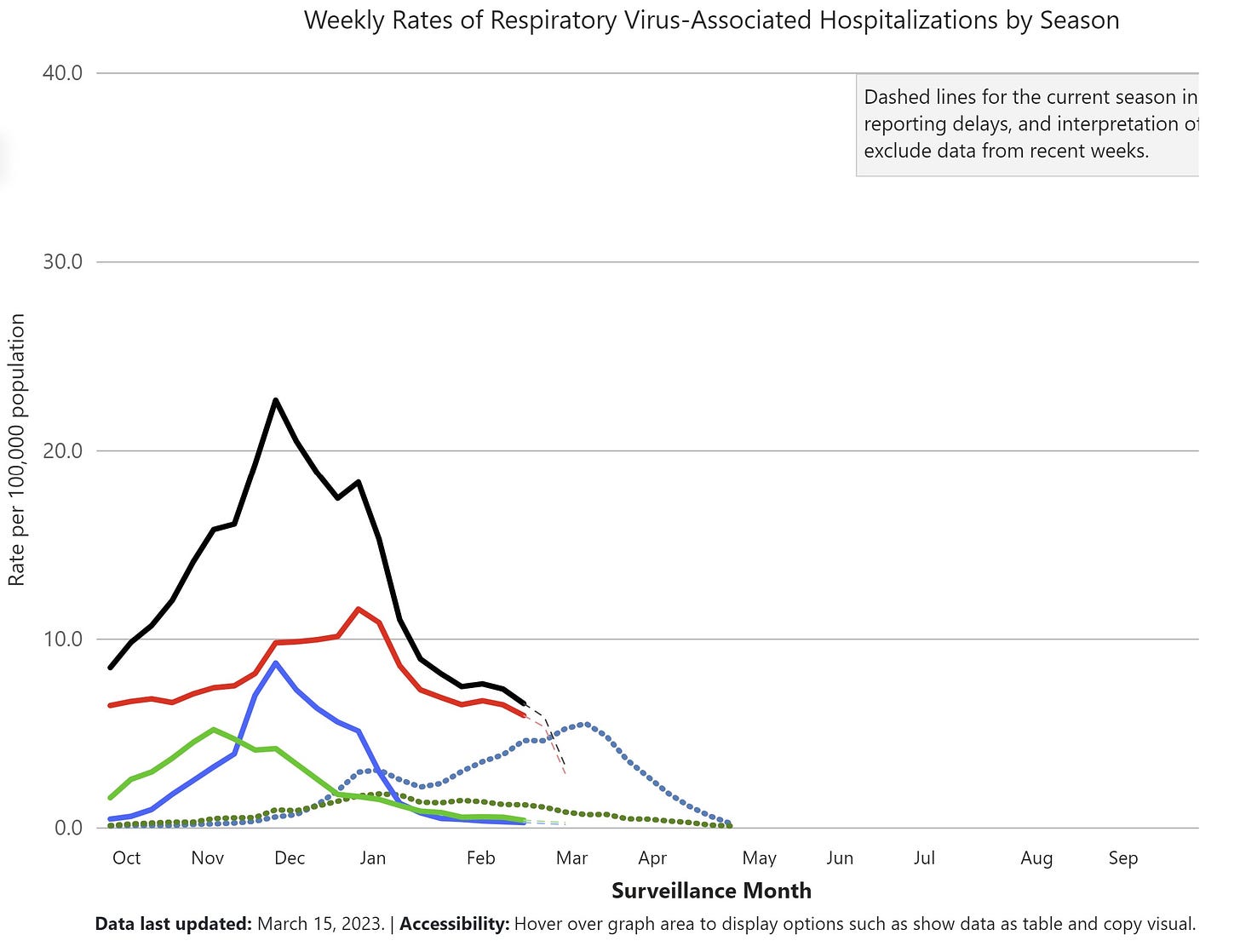
Hospitalizations for respiratory viruses peaked in December, which is ~3 months early. COVID-19 continues to take the lead for hospitalizations. Interestingly, RSV, COVID-19, and flu peaked at different times. This no doubt helped our healthcare systems and makes me continue to wonder if there is some sort of virus-to-virus interaction (RSV pushes flu and then pushes COVID-19, for example).
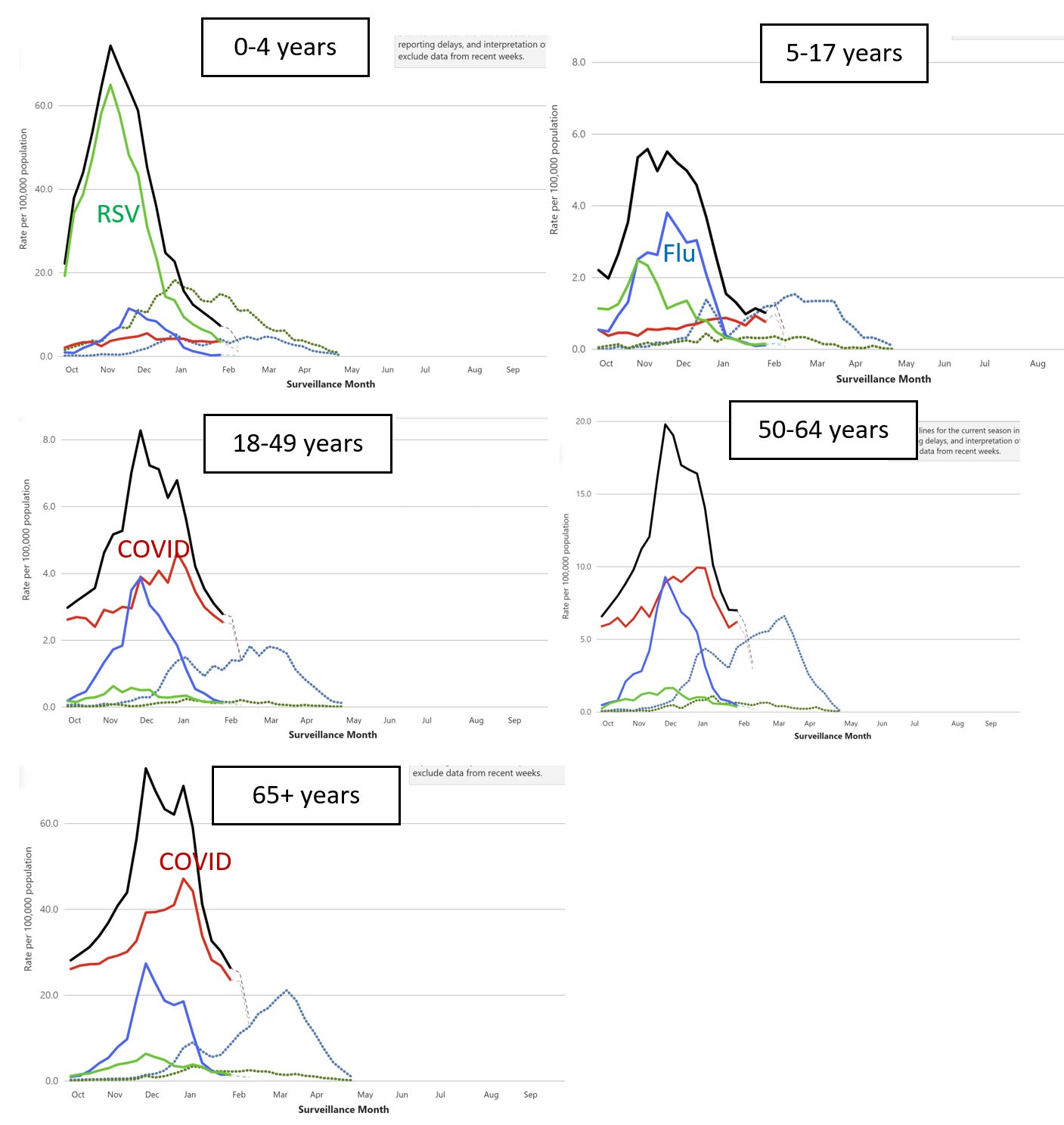
Different age groups experienced very different risks of hospitalization this winter:
0-4 years: RSV was out of control, peaking at 65 hospitalizations per 100,000. This was 244% higher than the 2018-2019 season. (We really need an RSV vaccine for our kiddos.)
65+ years: COVID-19 clearly led hospitalizations.
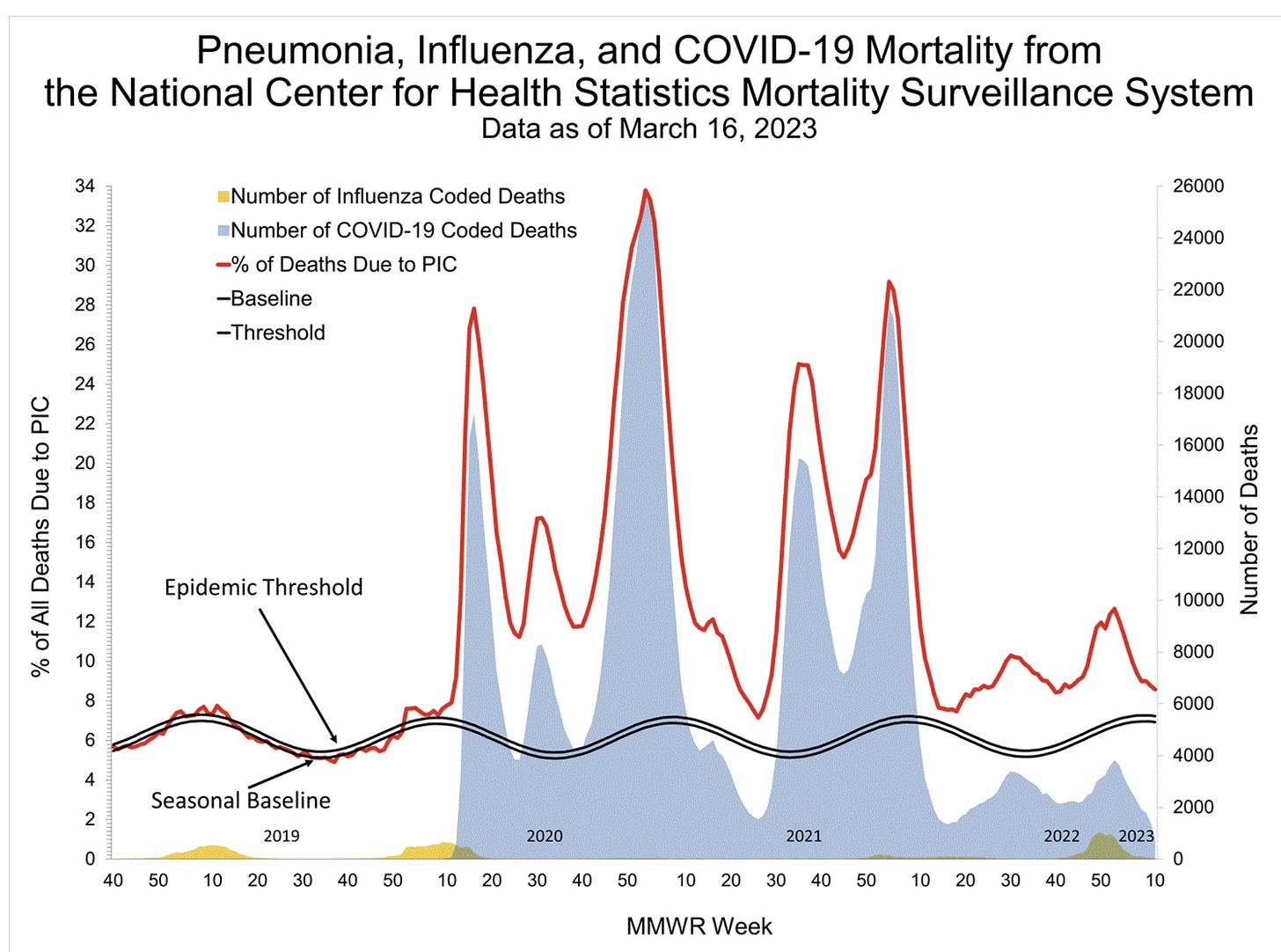
During this respiratory season (week 40-week 10), we lost 64,180 Americans to COVID-19. This number is higher than any pre-pandemic flu season (see yellow in graph below).
Excess deaths (red line below) continue to be above the “epidemic threshold” (black line). We haven’t had a national conversation defining the new baseline. What do we now consider normal given that we have an additional threat in our repertoire? As we move out of the pandemic phase, this black line needs to shift up.
A look forward
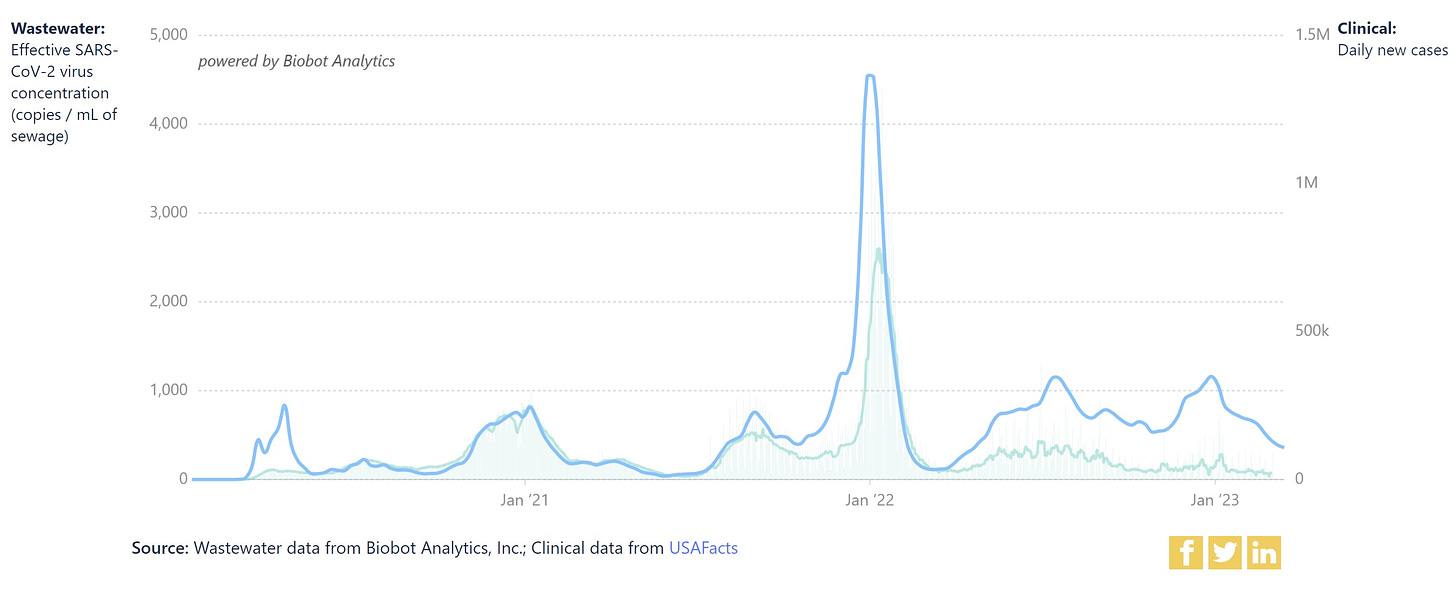
SARS-CoV-2 in wastewater is nosediving. However, levels in the Northeast have started to plateau. If this trend continues, having a high baseline throughout the year would be incredibly inconvenient.
SARS-CoV-2 continues to mutate quickly, as expected. The international community is keeping an eye on two Omicron subvariants:
XBB.1.9- In the U.K., this is causing a slow uptick across metrics, including hospitalizations. In the U.S., the growth advantage of this subvariant is only ~35%. (As a comparison, the original Omicron had a 500% growth advantage causing the tsunami.) In other words, we shouldn’t fret.
XBB.1.16–This has a case growth advantage of ~250% in India (17% increase in deaths). But, it’s hard to tell how much this is due biased testing and/or changing behavior due to the celebration of Holi.
XBB.1.16 could possibly disrupt a quiet spring in the U.S. But, a wave is not only dependent on weather, a new subvariant, or changing behavior, but also the number of susceptible people. This precise number is incredibly difficult to grasp because it depends on a number of factors: Who has been infected, when, and by what variant?
In other words, future waves are getting harder and harder to forecast.
With COVID-19 declining, flu may have the opportunity to start inclining for an out-of-season resurgence, especially since the Flu B strain hasn’t shown its colors yet in the Northern Hemisphere. No signs yet, but time will tell.
Norovirus
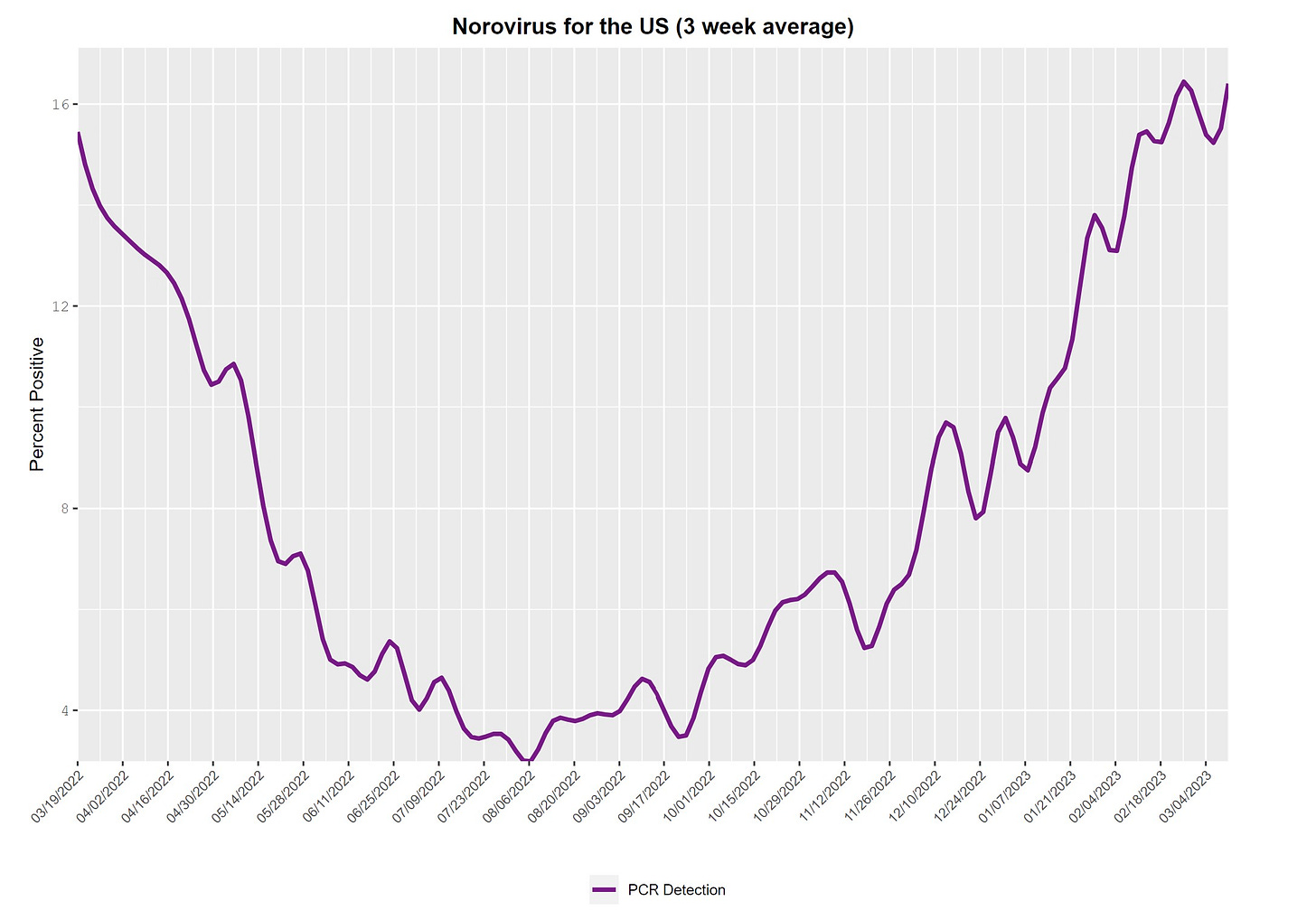
Norovirus wasn’t part of the “triple-demic” winter talk, but positive tests keep going up. It’s not entirely clear how high this will go, but in pre-pandemic times it typically peaked in March. Regardless, wash your hands.
Bottom line
Every pandemic winter has been unique and, thus, created unique challenges. While disease levels may be back to normal, the usual patterns are off. It may be years until we know how COVID-19 permanently changes the landscape.
In any case, reprieve is now here. For parents, flu and RSV are in the rearview mirror. For older adults and immunocompromised people, COVID-19 is declining. It will sure be interesting to watch how the rest of the year plays out.
Love, YLE
“Your Local Epidemiologist (YLE)” is written by Dr. Katelyn Jetelina, MPH PhD—an epidemiologist, data scientist, wife, and mom of two little girls. During the day she works at a nonpartisan health policy think tank and is a senior scientific consultant to a number of organizations, including the CDC. At night she writes this newsletter. Her main goal is to “translate” the ever-evolving public health science so that people will be well equipped to make evidence-based decisions. This newsletter is free thanks to the generous support of fellow YLE community members. To support this effort, subscribe below:


Good as per the reg.
A discussion in a bit on whether to boost, and what to boost with, would be useful. I'm sure you're already thinking it all through.
If we move the pandemic black line up to the
excess death line we will be taking one more step towards normalizing all of the covid deaths. Next step will to collapse all of the covid deaths into respiratory deaths and poof the pandemic will be gone. This is what the CD C is moving towards - hiding the data.
“Excess deaths (red line below) continue to be above the “epidemic threshold” (black line). We haven’t had a national conversation defining the new baseline. What do we now consider normal given that we have an additional threat in our repertoire? As we move out of the pandemic phase, this black line needs to shift up. “