Global pandemic
Global deaths due to SARS-CoV-2 are continuing to plummet and closing in on levels we only saw at the beginning of the pandemic. Although we are hopeful this continues due to increased vaccination and infection-induced immunity, many eyes are on four specific areas across the globe:
South Africa. The BA.4/5 subvariant leader continues to report exponential growth in cases and hospitalizations, although decoupling between the two metrics continues to widen. Death counts are at their lowest levels since the beginning of the pandemic and, thus far, high levels of BA.1 Omicron immunity are keeping deaths down. It will be important to continue to watch, as death counts are lagged.

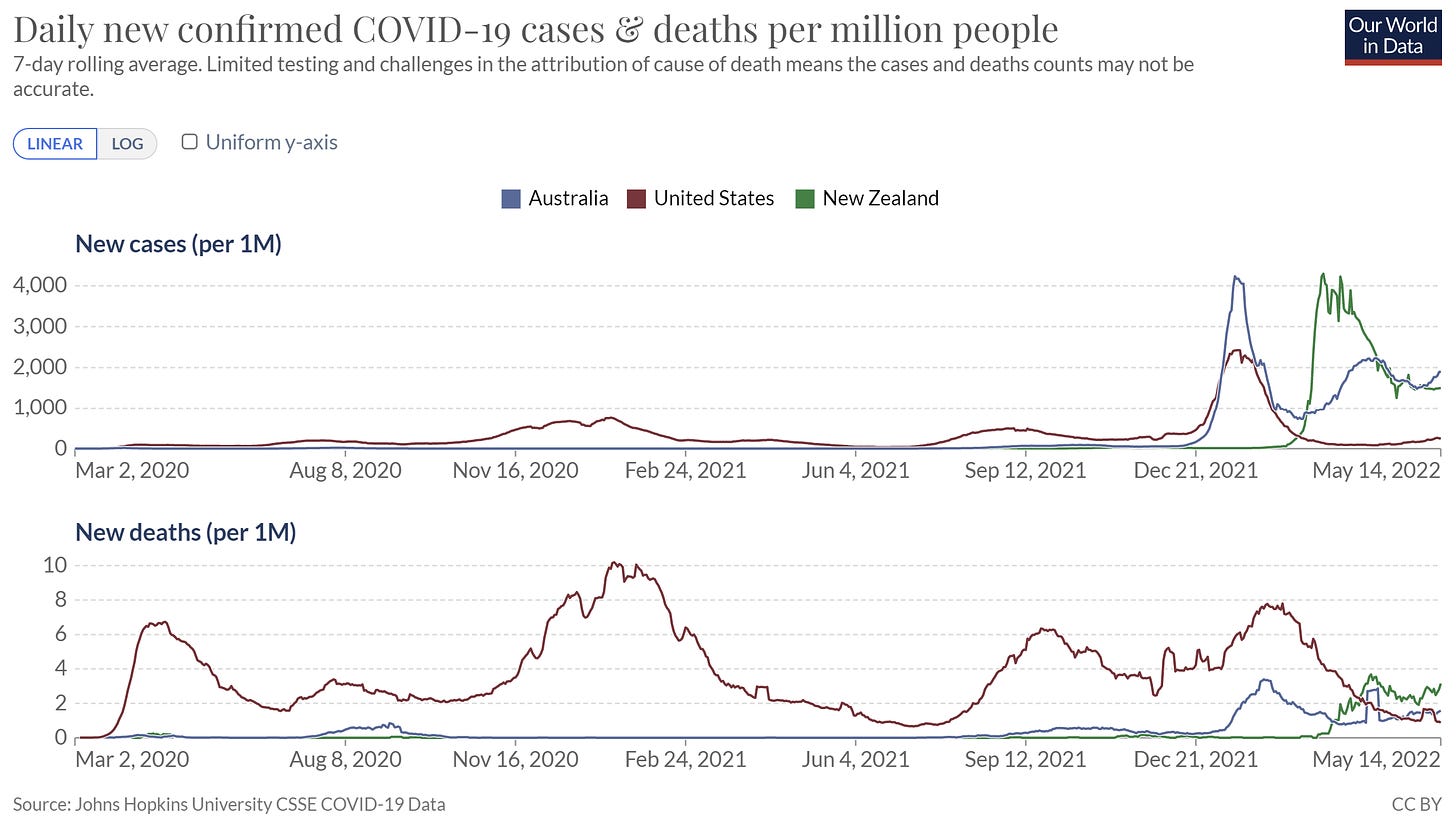
Australia and New Zealand. Two other Southern Hemisphere countries entering the winter season, Australia and New Zealand, are getting hammered with infections. Deaths have begun to increase, but thanks to their successful vaccine campaign during lockdown, cumulative deaths remain incomparably low. (Side note: We are seeing the comeback of flu down in Australia, which is always an early sign of what is to come in the fall for the U.S.)
North Korea. A humanitarian crisis is about to unfold in North Korea. On Saturday, state media reported 500,000 cases of unexplained fever in recent weeks and 26 deaths. Unfortunately, we expect mortality to skyrocket as they have one of the lowest vaccination rates in the world (due to refusal of vaccines offered by China) and a fragmented and underfunded hospital system. It will be tough to know the true toll in coming weeks due to limited testing capacity and what I will assume to be very little public reporting.
China is doubling down on their zero COVID policy. With only 30% of the older population fully vaccinated, the country recently went into lockdown in the face of Omicron. But they didn’t take this time to deploy a massive vaccination campaign. In fact, their vaccinations are decreasing. A recent Nature article found that if they lift their zero COVID policy without vaccinating, there will be over 1.5 million deaths and ICU demand 15 times greater than capacity. Together, this is making their long game unclear, disruptive, and dangerous.
United States epidemic
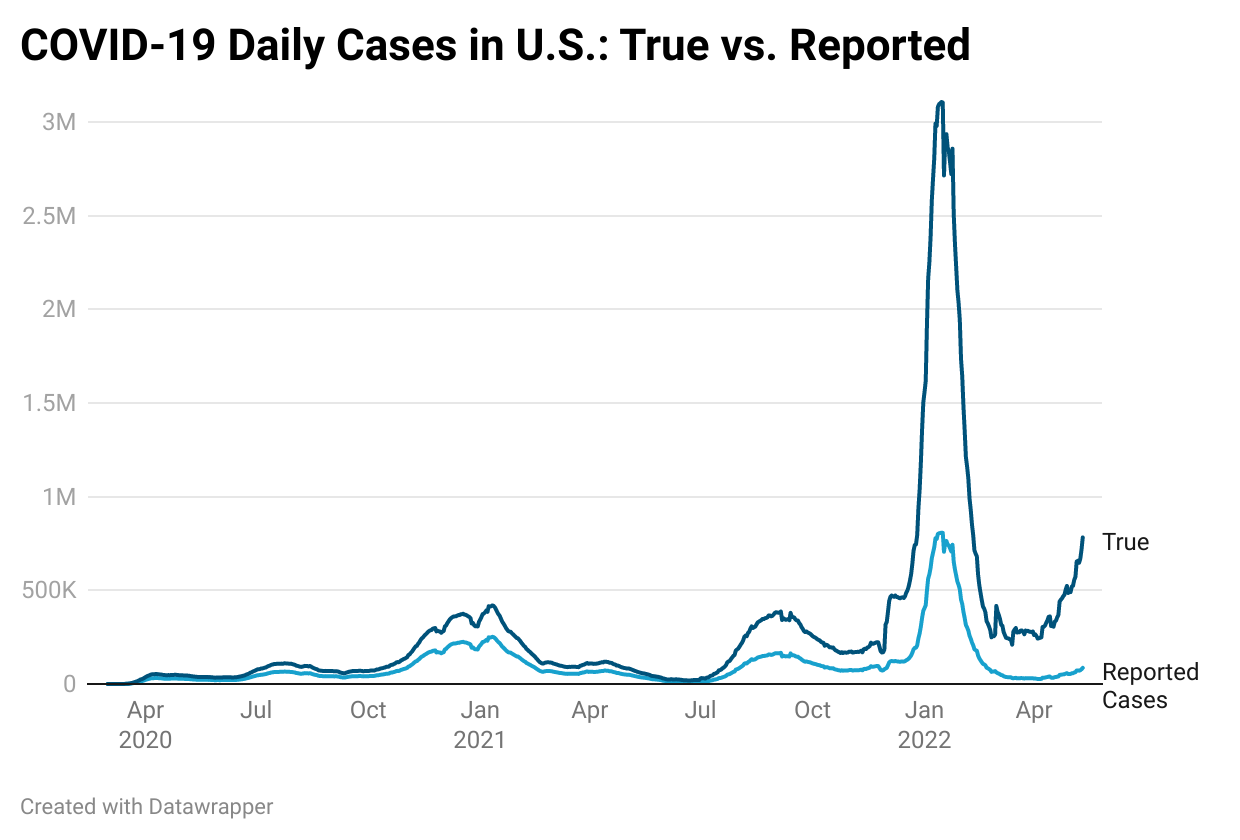
In the U.S., we are clearly in an infection surge right now, although you wouldn’t really know it due to underreporting, lack of communication, and pandemic fatigue. Using rough estimates, I plotted “true” case estimates against reported case numbers in the graph below. While we’re not close to the Omicron peak, we are already higher than the first two waves.
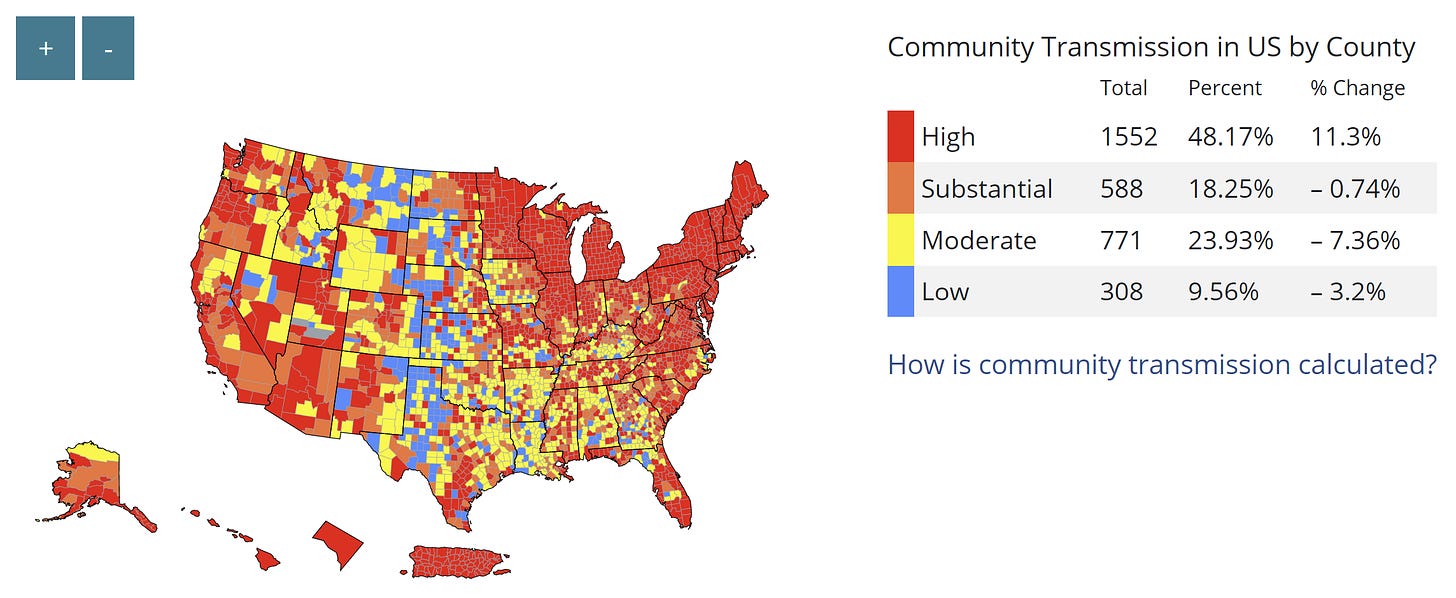
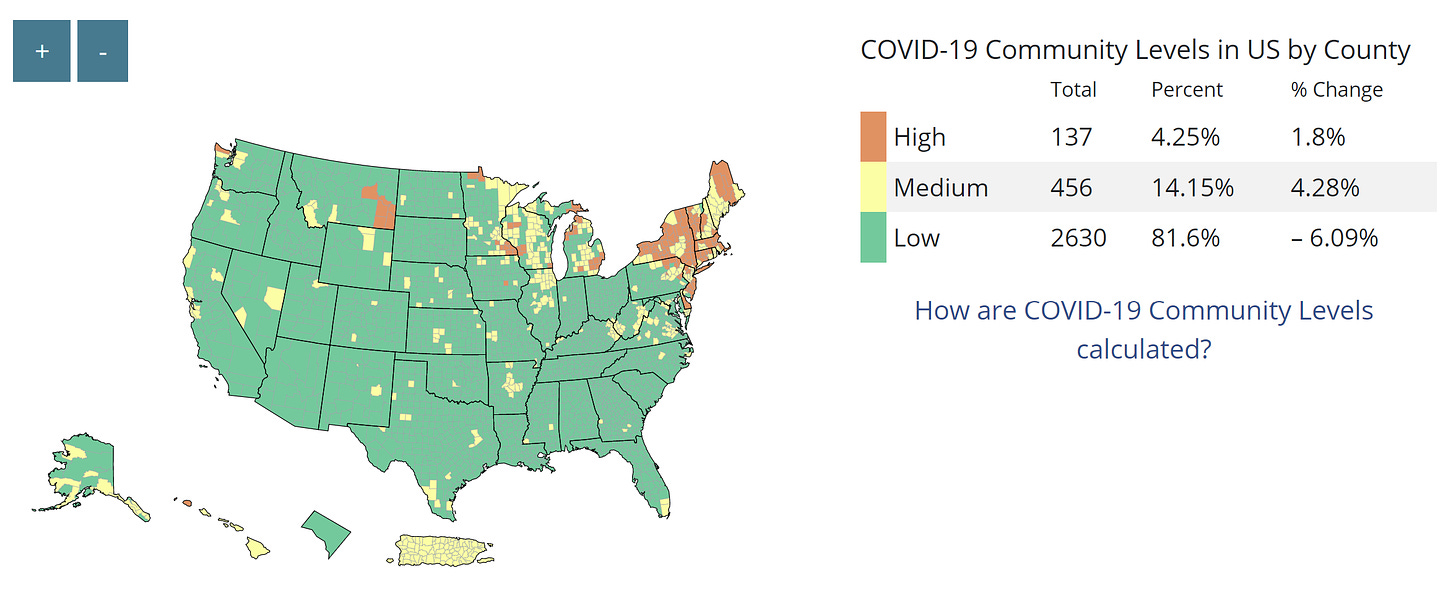
Another perspective is the old CDC transmission map, in which we have “substantial” or “high” transmission (more than 50 reported cases per 100K) across 66% of counties. This strikingly contrasts with the new CDC community map, which shows only 4% of counties need to mask because hospitals will not reach capacity within 3 weeks.
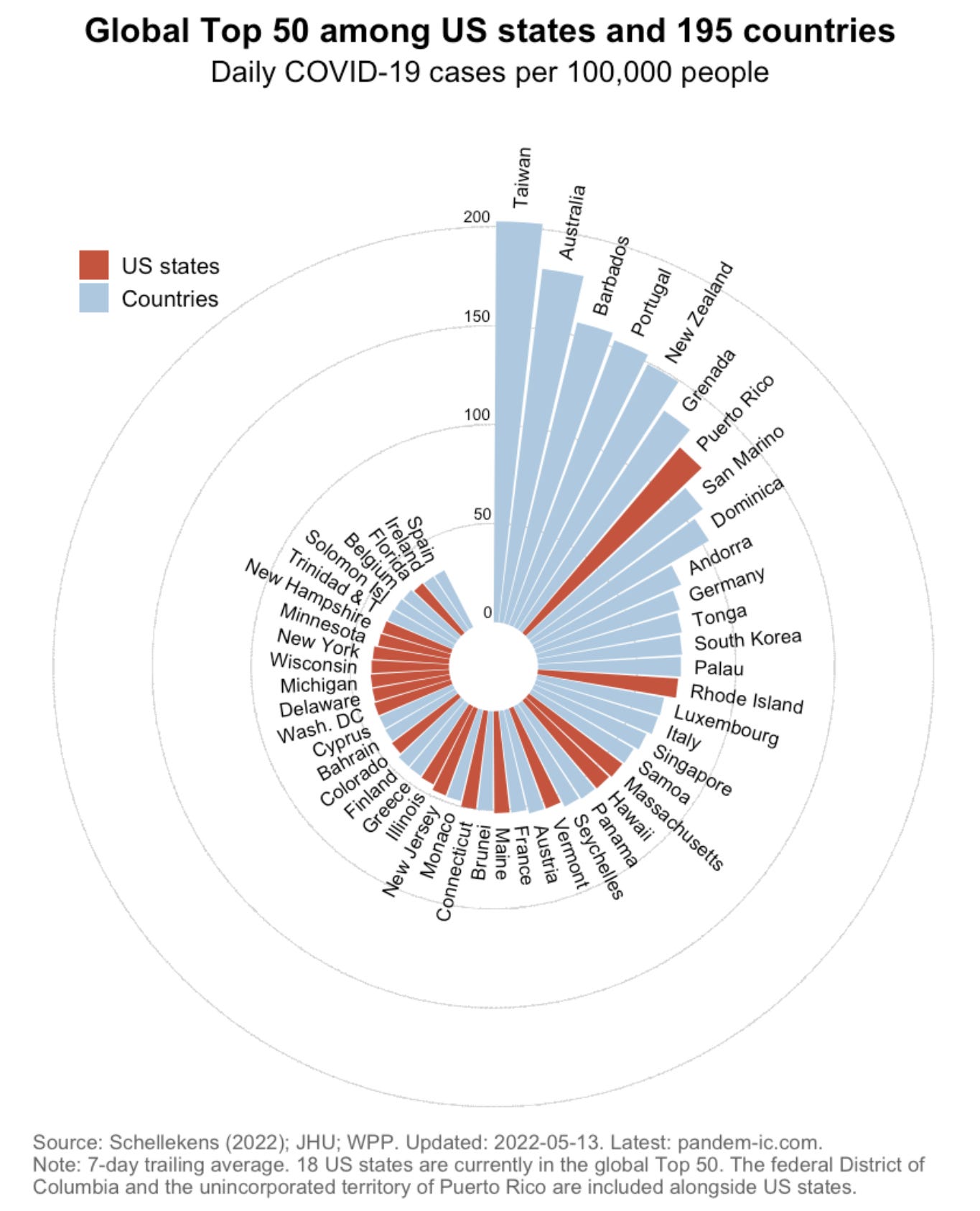
Cases are increasing in all states. If we assume uniform testing behaviors (and thus underreporting) across states, our case leader is Puerto Rico, which is getting hammered with infections but recently reached their peak. This is followed by Rhode Island and Massachusetts. Interestingly, if we compare U.S. states to 195 countries, 18 of them would currently be among places with the highest new cases per capita in the world.
Case accelerations are not regional, but occurring across the country. The acceleration leader is Mississippi (+224%) followed by Missouri (+211%), Utah (+169%), South Carolina (+152%), Arizona (+134%), and Louisiana (+131%). To me, the lack of regional patterns is a sign of a true national wave.
The current surge is at least partially due an increase in reinfections, as Omicron is getting better and better at dodging our first line of defense. The CDC's last update on reinfections was in January, but the story is very clear among local jurisdictions tracking this data closely. In Colorado, for example, 82% of reinfections have occurred since Omicron with the majority among unvaccinated. Starting in March 2022, North Carolina reported an increase in reinfections. In Indiana and Idaho, reinfections account for 12-18% of reported cases.
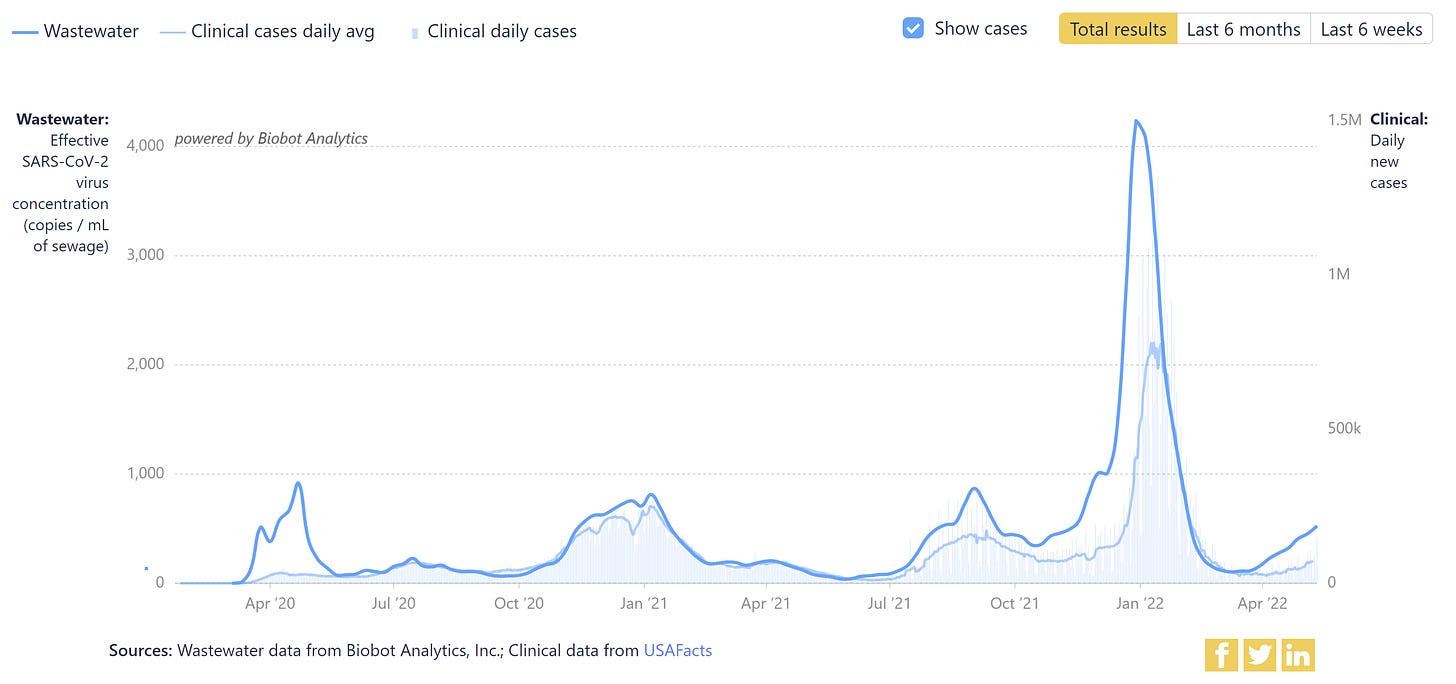
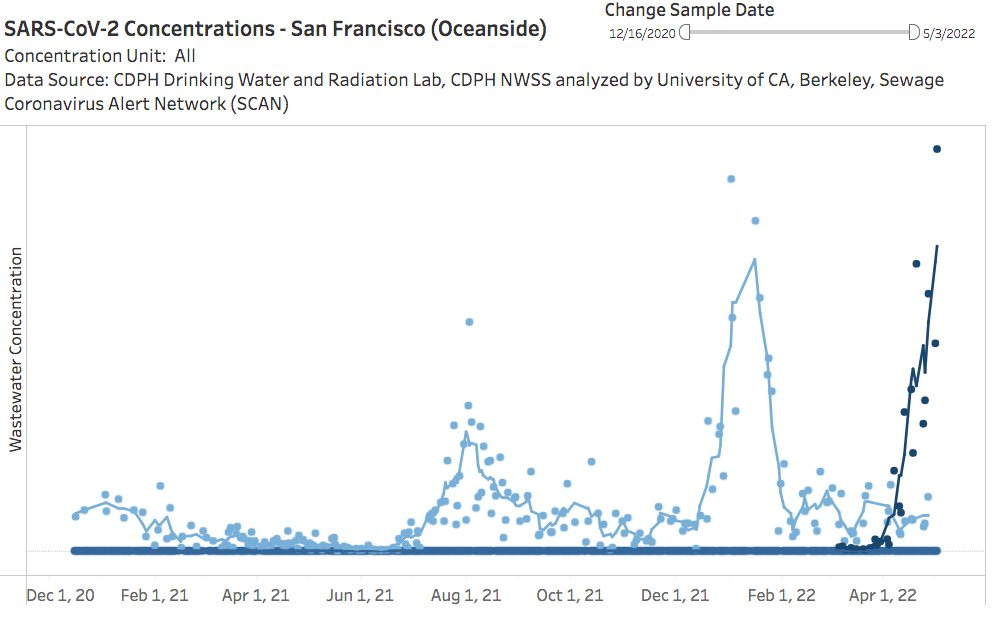
Increasing case counts are reflected by wastewater surveillance systems across the nation (see first graph below). On a local scale, San Francisco wastewater levels are skyrocketing. In Boston, wastewater finally found a consistent pattern and is on the upswing due to BA.2.12.1.
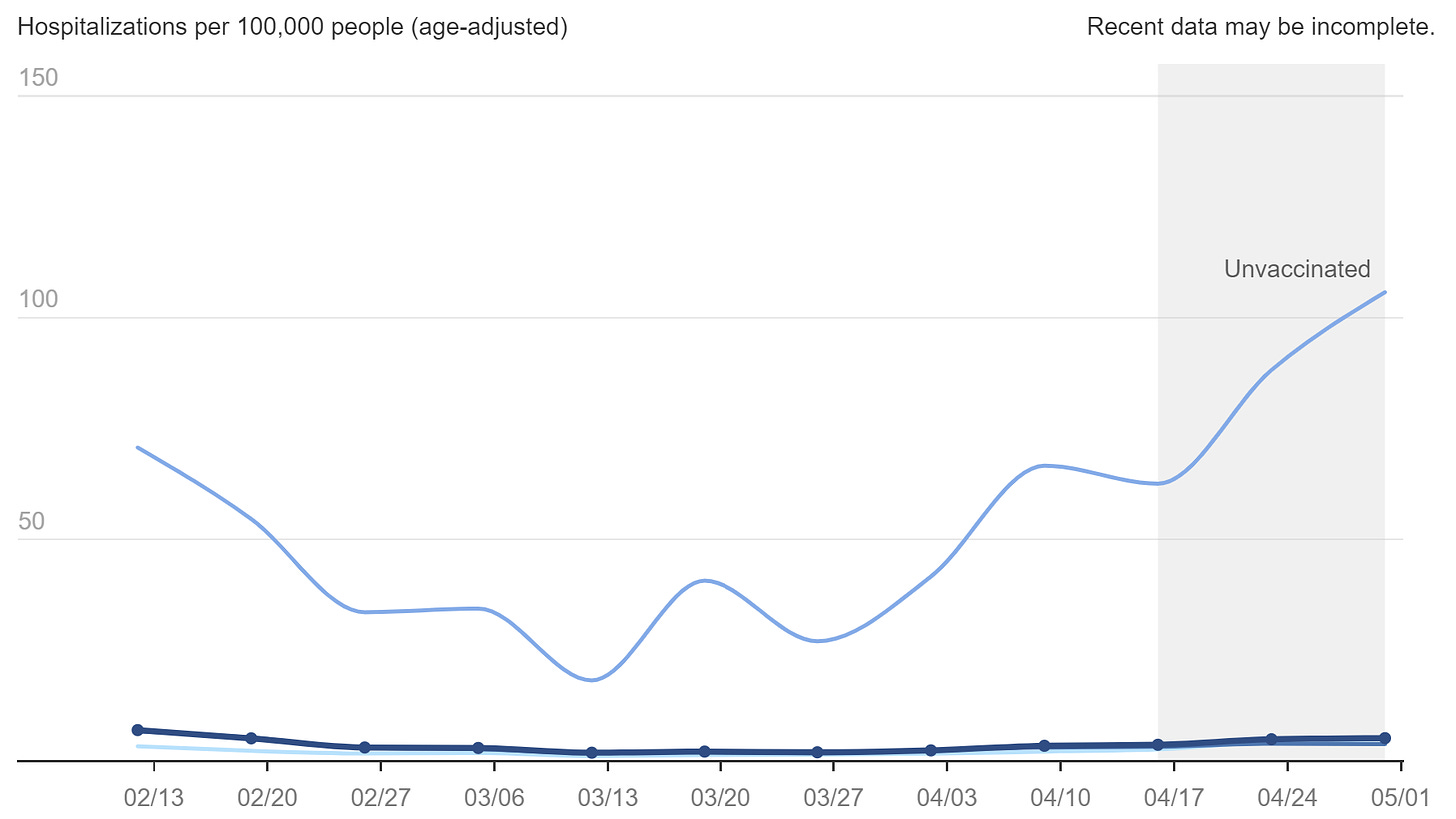
Hospitalizations are also increasing with a +23% change in the past 14 days. It will be very interesting to see how the rate soon changes (or doesn’t change) as hot spots move to less vaccinated parts of the U.S. As seen in the graph below from New York City, there continues to be a large discrepancy between unvaccinated and vaccinated.
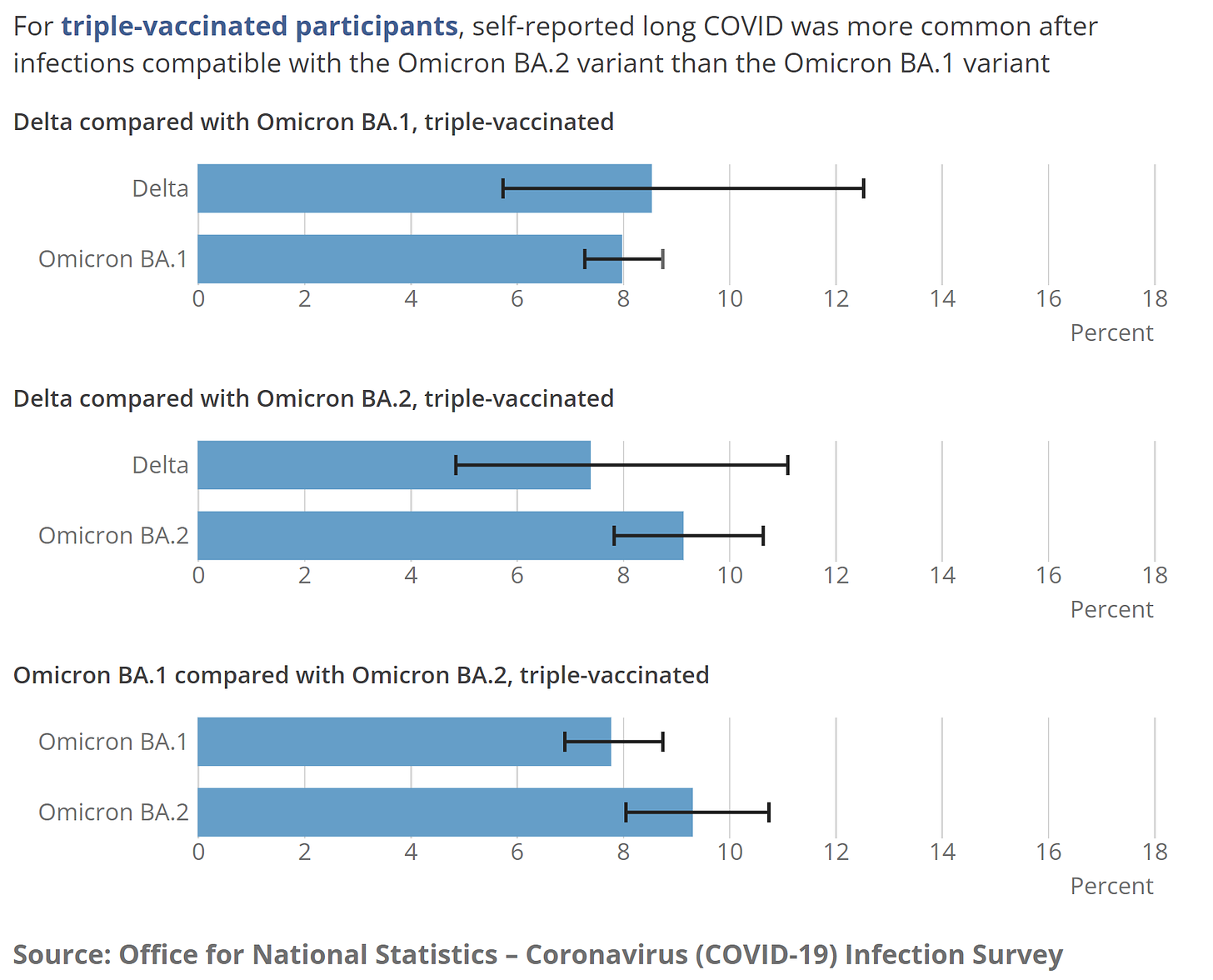
Unfortunately, severe disease is not the only outcome. While evidence continues to show that vaccinations reduce risk of long COVID by ~50%, the most recent UK Health Security report found even those boosted aren’t spared. Among the triple vaccinated, 8-9% of people report long COVID (at least 4 weeks) after their first infection; 5-6% are reporting activity-limiting symptoms. There doesn’t seem to be a statistical difference between variants.
Bottom line
We are in the middle of an infection surge. If you’re vaccinated and healthy, there is a very small chance of landing in the hospital, but severe disease isn’t the only outcome, vulnerable pockets around you may not be protected by their vaccine, and more cases means more variants. We don’t need to be alarmed, but we certainly can’t be complacent. We need the will and the heart to beat this virus, as it’s certainly not done with us.
Love, YLE
In case you missed it:
Full YLE archive here
“Your Local Epidemiologist (YLE)” is written by Dr. Katelyn Jetelina, MPH PhD—an epidemiologist, biostatistician, wife, and mom of two little girls. During the day she works at a nonpartisan health policy think tank, and at night she writes this newsletter. Her main goal is to “translate” the ever-evolving public health science so that people will be well equipped to make evidence-based decisions. This newsletter is free thanks to the generous support of fellow YLE community members. To support the effort, please subscribe here:





I am an internist in Chicago. I am getting more Covid-positive calls in my practice than at any other time in the pandemic. I am somewhat surprised that this wave is not getting more attention, though I completely agree with your reasons why. Most of my patients are confirming their Covid status with home testing only so there is no good way to keep track of the numbers. Does it really matter what the numbers are? Because of Long-Covid and the yet-unknown potential for long-term disability, sadly, I think they do.
We are basically living in two realities. One is in which life has returned to "normal" and COVID is seen as more of a catching a bad flu. Talking with friends, they are seeing in their local groups/lives people testing positive and getting out and about because they don't feel that bad, so the whole "quarantine" at home is out the window as well. The other is that in which people are proactively looking at numbers and making decisions on masking etc.
What is concerning is the long covid issues. There insurance companies were already reporting higher disability claims last year. The number of infections is so large, that long covid that impacts every day life will be relatively large and that is going to impact everything from employment to health care, to government benefits, to insurance rates increasing.