The respiratory illness storm ravages on. And it’s only November. Here is where we are with the “triple threat.”
RSV
Cases of RSV continue to skyrocket. Data shows we are testing a lot, though, as test positivity rates are not as high as in 2021. This is likely attributed to increased knowledge, which is good news. In addition, there are hints that RSV is peaking. With RSV, antigen test positivity rates usually peak before PCR, and that’s what we are seeing now. Cases may soon follow.
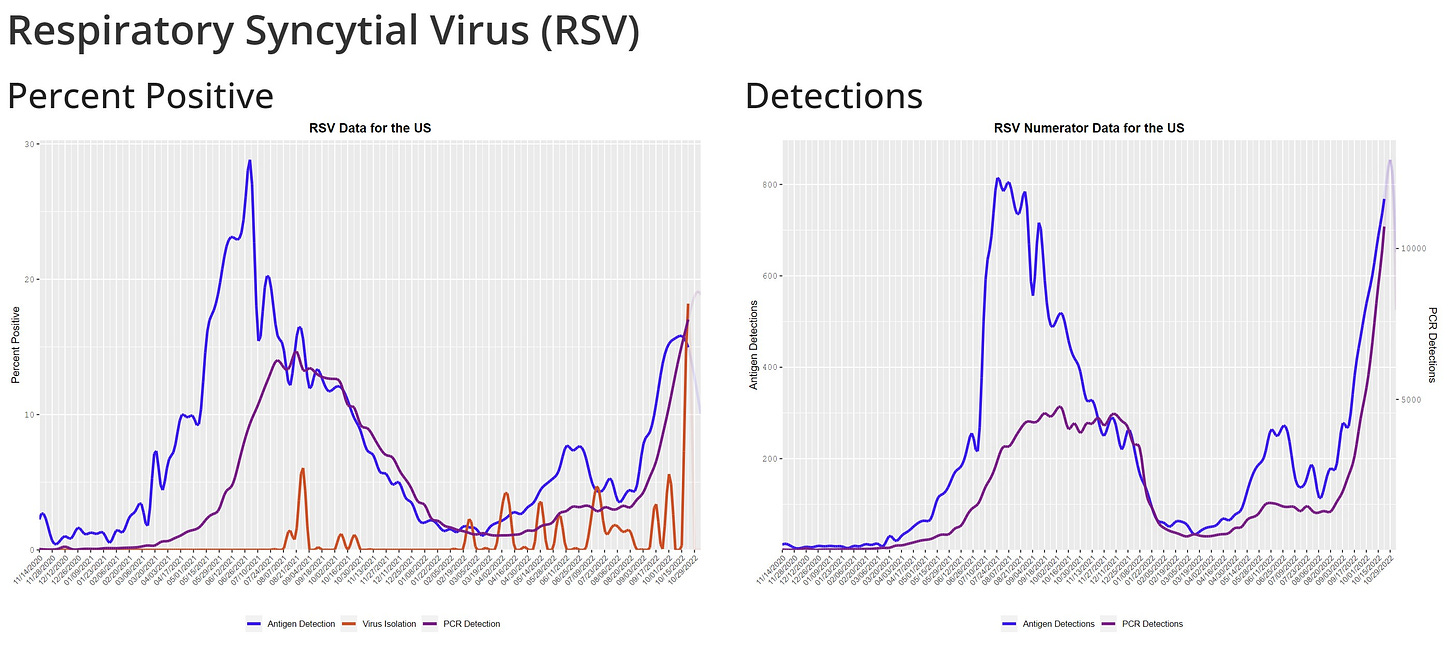
Historically, the RSV season lasts 5 months. It will be interesting to see how the holidays impact RSV patterns, though. Typically RSV peaks in January, but because it has arrived so early, we are in new viral dynamic territory. There’s no doubt that social networks will change next week due to Thanksgiving. For example, we will see family that we don’t typically see. This will open up new pathways for transmission, and RSV numbers may therefore continue to rise.
Influenza
Flu is right behind RSV and coming in hot; it’s earlier and steeper than previous pandemic and non-pandemic years.
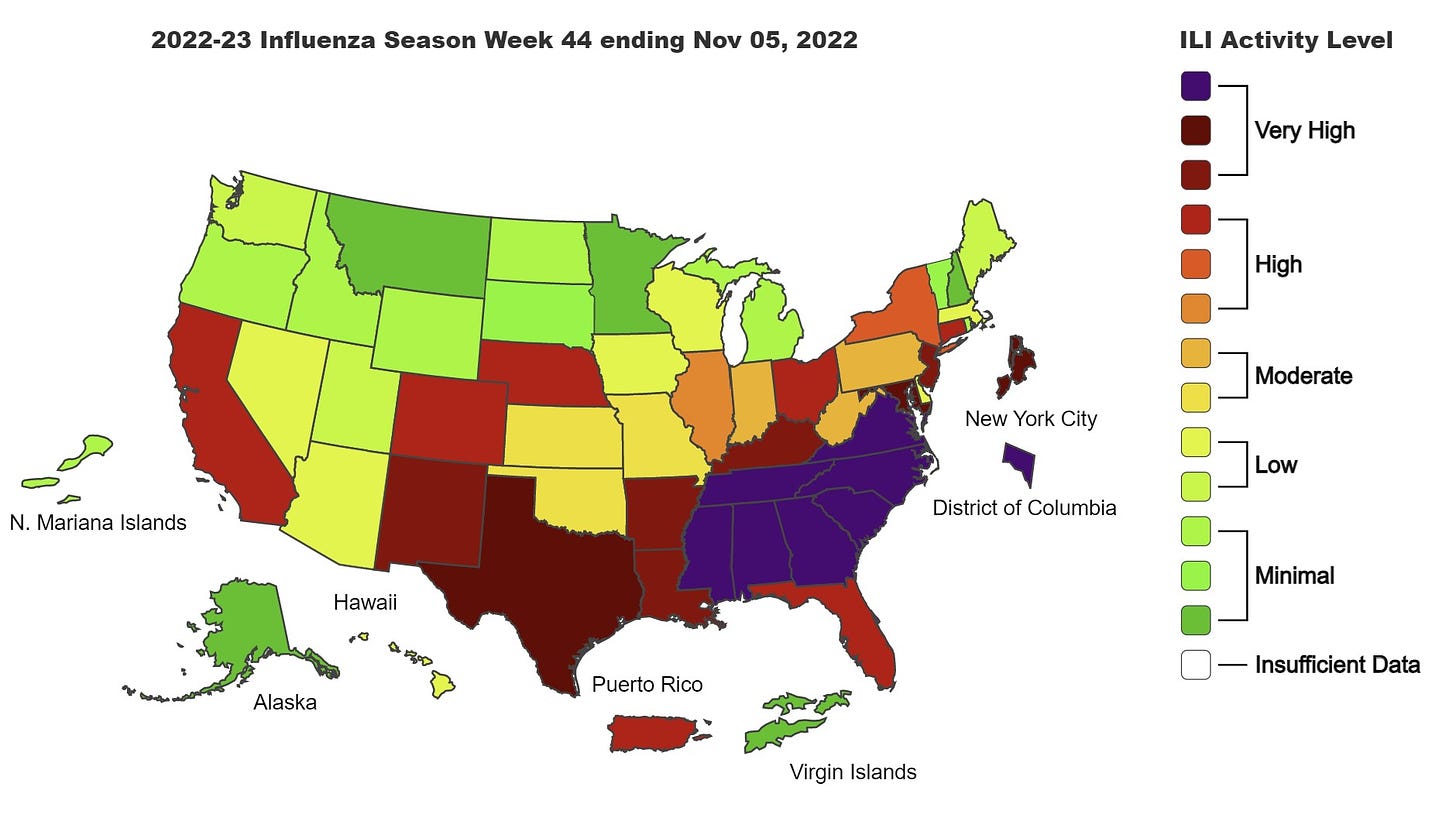
We certainly see regional variability of the flu. A number of states in the South and the Atlantic seaboard, for example, have the highest activity level color that CDC records—purple in the map below. (The first time CDC used a purple color was in Louisiana in 2019, when they added it to the scheme due to very high levels.) This is causing flu surveillance at Johns Hopkins, for example, to go off the charts as seen below.
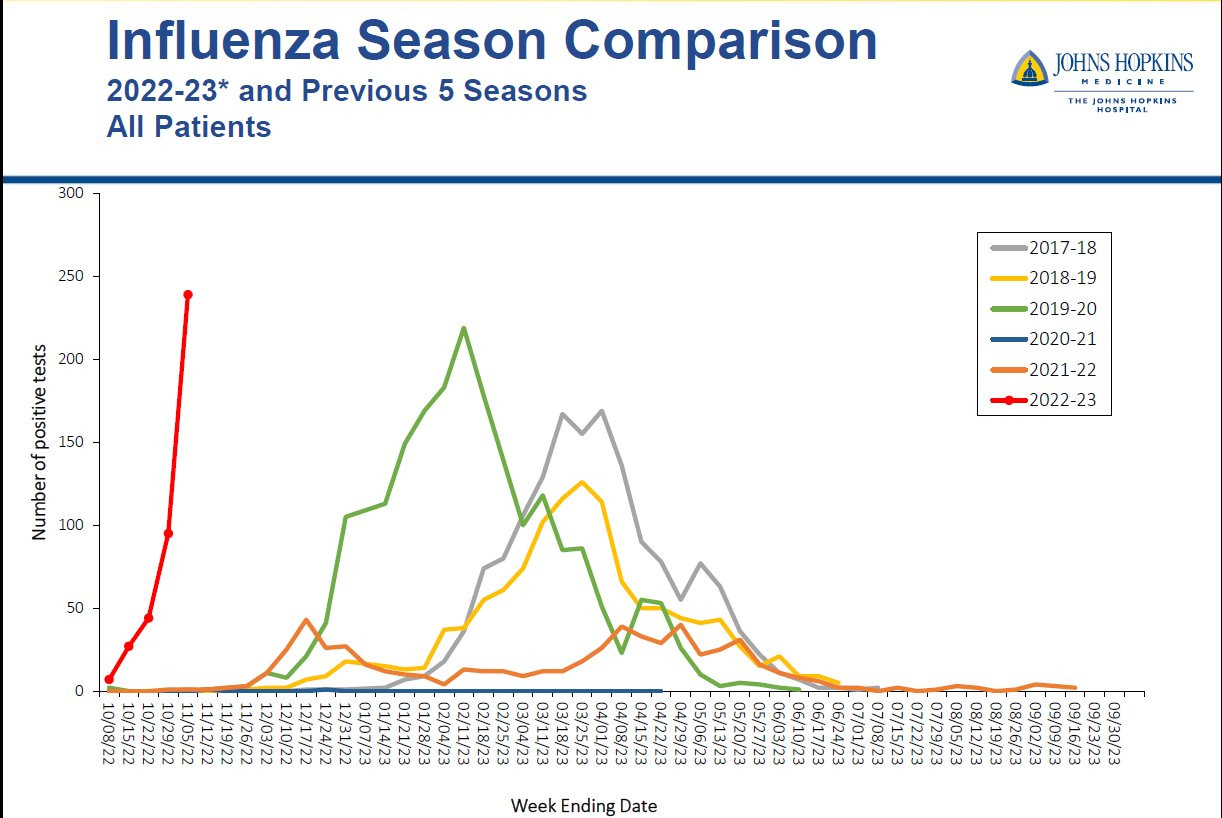
There is good news from the Southern Hemisphere among countries that just concluded their flu season. Chile, for example, found the flu vaccine is a good match for the current strain. They are reporting a 49% efficacy rate. But only 28% of Americans are vaccinated against the flu. This is almost 10 percentage points lower than pre-pandemic rates, which is frustrating.
COVID-19
Interestingly, for the first time during the pandemic, there are more than 300 subvariants circulating, and not one is dominating globally. This isn’t stopping the virus from causing waves, though. SARS-CoV-2 is currently creating two global hotspots: Western Pacific and Southeast Asia. In South Korea, for example, we see an increase in cases and hospitalizations due to the variant soup (lots of lines of color in the figure below are increasing, as opposed to just one or two lines of color that we’ve historically seen).

Other areas across the globe are starting to tick upward, including admissions in South Africa and Western Europe. Similarly, these upticks are not due to one variant but rather a mix of Omicron subvariants, waning immunity, weather, and behavior change.

The real headscratcher is that the U.S. wastewater continues to plateau, but given previous patterns, a wave should have started by now as BQ.1 accounts for more than 50% of cases. A lot of eyes are on the West, too, as a new Omicron subvariant—BN.1— is growing.
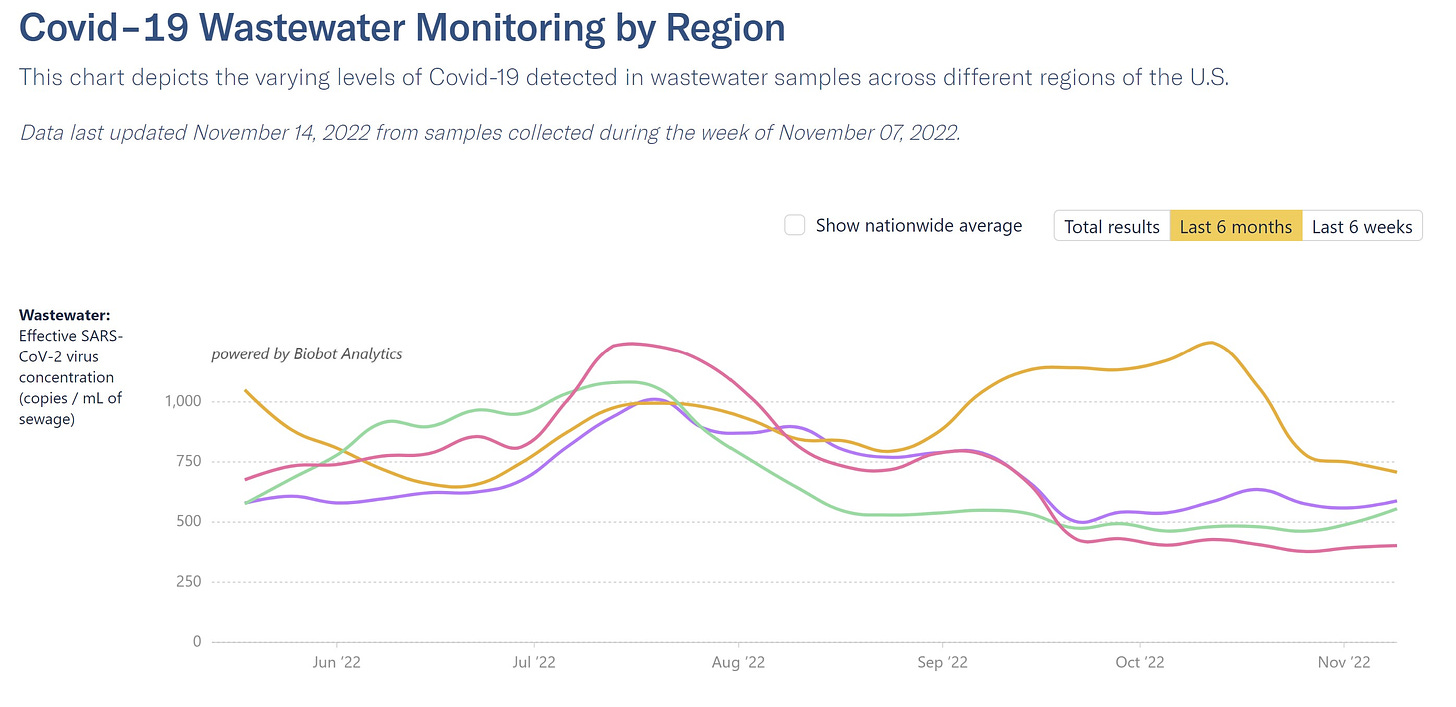
Given trends in Europe, it is still very likely that the U.S. will have a COVID-19 wave. But, overall, this could be a good sign that we finally have an immunity wall that is challenging the movement of COVID-19, regardless of labs showing subvariants can partially escape immunity. We need to hold off on sweeping conclusions—like whether this pandemic is over— until this winter plays out.
Implications
The convergence of these diseases has three important implications:
Impact on hospital systems. The hospitals, and in particular pediatric hospitals and emergency departments, are hanging. by. a. thread. Every pre-pandemic winter, pediatric hospitals were overwhelmed. This year the unique combination of circumstances is creating terrible strain, which has many implications, including the quality of care for everyone. We need to fix this on a systematic level.
Risk of co-infections. Someone can be infected with two viruses at the same time. In fact, the first death from RSV and flu co-infection was reported in a child under 5 years old in California.
Lessons not learned? I had hoped we would have applied lessons from COVID-19 to other diseases, like masking, staying home while sick, and getting vaccinated. Unfortunately, it doesn’t seem like this is happening. After 2.5 years of a pandemic, the public (and leadership) is just in a different state of morale, and the willingness to take preventative steps seems to be lower.
Bottom line
“Normal” viruses are continuing to show their muscle, and the seasonal virus repertoire now includes COVID-19. We are very concerned going into winter, as this situation is already applying massive pressure to hospital systems. Time will tell how the next few months play out.
Love, YLE
“Your Local Epidemiologist (YLE)” is written by Dr. Katelyn Jetelina, MPH PhD—an epidemiologist, data scientist, wife, and mom of two little girls. During the day she works at a nonpartisan health policy think tank, and at night she writes this newsletter. Her main goal is to “translate” the ever-evolving public health science so that people will be well equipped to make evidence-based decisions. This newsletter is free thanks to the generous support of fellow YLE community members. To support this effort, subscribe below:





Thanks for the great summary. My wife and I still mask, still wash our hand with alcohol after being in stores. We are still exercising the same level of infection risk minimization as we did in 2020. Are we stupid or have some psychological addiction to feeling ourselves to be at risk? Emphatic no's to both questions. The pandemic is still here, declining leading indicators notwithstanding, could very suddenly jump in severity, has a huge zoonotic pool to breed further mutations that escape our monitoring and early warning systems, and having killed millions of us, still retains the capacity to kill millions more. In our opinion, the risk still justifies taking the minor precautions we do.
And that's not even counting RSV which at our age is a very real danger.
I know everyone is very pandemic weary and interest in infectious diseases is probably dropping off. But consider this: the people who are losing interest, some not inconsiderable fraction of them, have the luxury of going into "back to normal" thinking because large numbers of us did take the pandemic seriously and flattened the curve. [minor spelling correction edit just now,]
I can't but feel we are stuck in this loop:
"We are seeing these surges because of the measures we took in 2020"
So...
"We need to take the measures we took in 2020 to reduce what we are seeing today"
Can you see why the public has "moved on"? (by that I mean, the 10% ceiling we hit for boosters, the near zero masking rates, the largely return to "normal" in schools, business, etc).
Were it not for reading Twitter and Substack, I don't think I would even realize Covid or Twin or Tripledemics are a thing still. Even Facebook has moved on (no one adding "I got my 4th dose" frames, picturing themselves in masks, etc like the old days). It's not something making the news, not in local papers (Plain Dealer for me). Even the weekend edition of the WSJ's only reference to Covid on the front page was a small blurb "China eased pandemic controls, as the country's leaders seek to lessen the pain of stringent zero-Covid policy that has exacted a heavy economic toll and stoked growing public resentment".
And I want to go back to something you said last week in the RSV is "Back:FAQ" from last week in your commentary on Immune Debt:
>"The pandemic delayed first infections of common viruses, like RSV, due to shut downs, social distancing, masking, etc. We saved thousands of lives doing this until we could get a COVID-19 vaccine. This was the right call."<
A comparison of Excess Mortality - a topic that used to be frequently invoked early in the pandemic - appears to contradict this statement. (I consider Excess Mortality the gold standard of outcome, anyone reading this and disagrees, please discuss with me below.)
If this was true, then we should see correlation between vaccine update, stringency of shutdowns, adoption of masks and excess mortality. Countries like Sweden, Denmark, and Finland which had kids in school nearly the entire pandemic, didn't mask young children, had low mask use relative to the rest of the world, should have poorer outcomes than countries like South Korea, Germany, Israel.
Yet the opposite is true.
Sweden has the second lowest excess deaths the entire pandemic after Norway. Zero excess deaths under the age of 65. South Korea meanwhile is poised to become one of the leaders in excess deaths - already in the first 30 weeks tracked of 2022 they have 215,000 deaths when trends predicted 170,000.
Let that sink in. South Korea, the beacon of masking, vaccination, GPS contact tracing, CCTV surveillance, and icon of "Doing It Right" now has the highest excess mortality in the world.
How can we argue "we saved thousands" doing something, when we can clearly see countries not doing that same thing didn't pay a consequence and even had better outcomes?
Katelyn you have done an incredible job writing, communicating, and building this blog/community the last two years.
I trust your dedication to the scientific process, but I urge you listen to Carl Sagan:
"Science invites us to let the facts in, even when they don’t conform to our preconceptions. It counsels us to carry alternative hypotheses in our heads and see which best fit the facts. It urges on us a delicate balance between no-holds-barred openness to new ideas, however heretical, and the most rigorous skeptical scrutiny of everything-new ideas and established wisdom….. When we are self-indulgent and uncritical, when we confuse hope and facts, we slide into pseudoscience and superstition."
From the data I look at, it appears that multiple hypotheses have failed and continue to fail, but whether it is due to politics, or pride, or hubris, many public health officials are unable to accept they were wrong and update their priors. Don't get dragged down by them. We have entered a phase of gaslighting (see: "we never said the vaccine kept you from getting the thing you are getting vaccinated against" - again, you are one of the few to not be trapped by that like Walensky, Fauci, Bourla, etc) to denial.
All of these hypotheses - masking, social distancing, closing schools, selecting which business can be open, plexiglass at checkouts, Halloween candy chutes for trick-r-treaters... all of this was built from observational studies, models, and opinion pieces - the lowest tier of science. There is no shame in conceding that many of these hypotheses failed real world stress tests and experiments. It's not like these ideas were built from decades of repeated RCTs undergoing critical appraisal. We should have no obligation to continue to support and back claims which have been falsified, less we fall for the sunk-cost fallacy.