Happy Halloween! Is this respiratory season getting spooky? (I couldn’t resist.) Here is your State of Affairs.
Influenza-like illnesses
The climate of respiratory health in the United States (coined “influenza-like illnesses by CDC) continues to creep up but still remains below the “epidemic” level threshold. So far, this year seems to have landed somewhere between pre-pandemic years and last year.

Two demographics are specifically seeing increased activity:
The South, with “moderate levels” of respiratory virus activity peppering the landscape.

Kids under 4 years old, with emergency department visits beginning exponential growth for respiratory illness.

Here is a deeper dive into the “big three” viruses.
Covid-19: Plateauing
After a healthy decline, all Covid-19 metrics have plateaued. This follows the previous year’s patterns, as shown in wastewater below.
Covid-19 continues to dominate respiratory hospitalizations and deaths, regardless of plateauing, though.

SARS-CoV-2 continues to mutate. A recent study found that it mutates faster than other viruses, including 2.5 times more rapidly than flu. Two specific subvariants are making the news:
HV.1. This is an Omicron sub-variant taking over. This is a relative of XBB (if you remember, this is the Covid-19 fall vaccine formula) and its mutations represent a small incremental, ladder-like evolution (as we would expect and hope for).
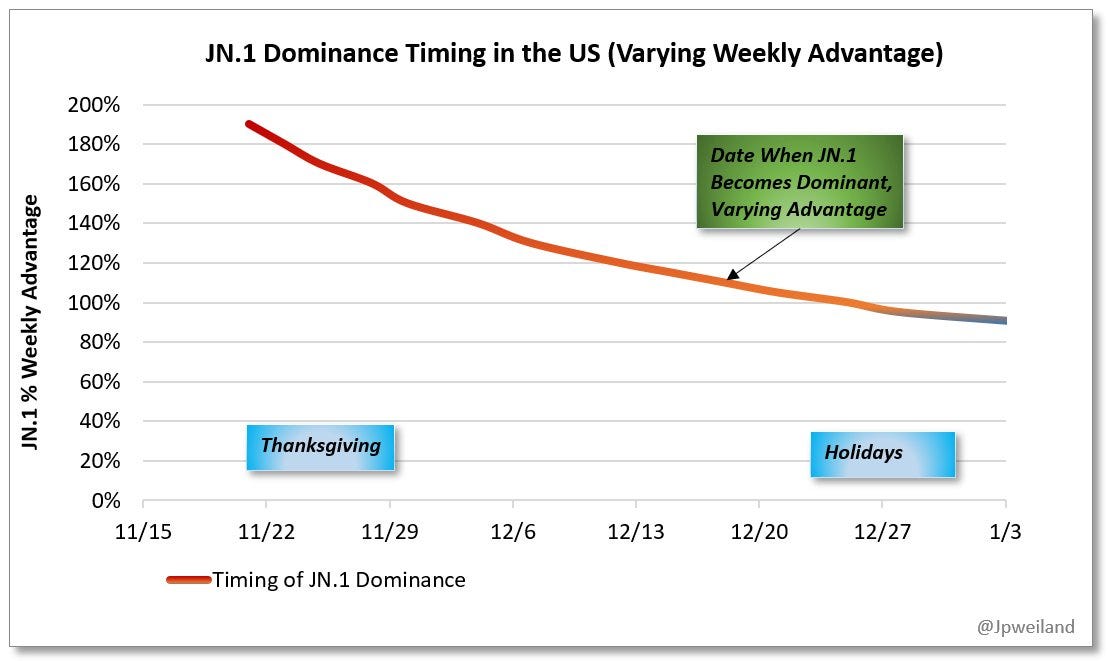
JN.1. The highly mutated variant we discovered a few weeks ago (BA.2.86) has started to mutate and has been given the name JN.1. The estimated percentage of cases is very small—about 0.1%.— but catching the eye of scientists because of how quickly it’s growing in France and the U.K. (between 116-132% growth advantage; as a comparison the original Omicron was 500%). If we assume it can spread as fast in the U.S., JN.1 will reach dominance between November 22 and January 3. This is not great timing, as holidays will help fuel the fire, resulting in a wave. We do not think this will cause a tsunami.
Flu: Low and stable
Not much to report here. Influenza remains at low levels. Hospitalizations, as shown below, are not yet making movement. There have been no influenza-associated pediatric deaths yet.
RSV: Exponentially increasing
RSV, though, is well on its way. Yet again, this is very early in the season compared to pre-pandemic times. CDC predicts this wave won’t get as high as last season, thanks to last year’s immunity wall. (RSV immunity wanes less quickly than, for example, Covid-19). Time will tell.

Three RSV notes:
RSV antibody medication (i.e., monocolonal antibodies) for babies is extremely strained. The CDC alerted physicians that they should ration for the highest-risk kids. Not having an adequate supply is incredibly frustrating, as the potential of this drug was huge, given that this is the leading cause of hospitalizations for those under 5.
RSV vaccine for older adults: Remember V-Safe? The text messages you received for the Covid-19 shot from CDC? Well, CDC adapted it for RSV vaccines. If you’re over 60 and had/getting your RSV vaccine, please sign up! This will help immensely with vaccine safety surveillance.
Questions about how to protect yourself against RSV? Check out this YLE Q&A from last year.
And, some good news
I got the Novavax last week. mRNA vaccines have consistently given me 48 hours of terrible side effects. So, I was crossing all my fingers and toes that it wouldn’t be the case with Novavax. And guess what?! NOT ONE SIDE EFFECT. Heck yes. If you’re in the same boat as me, try Novavax. You may have the same luck.
Bottom line
Respiratory season is heating up. But guess what? We can do things to protect ourselves, like getting vaccinated. If you’re not up-to-date, the time is right now.
Have a wonderful Halloween holiday! I look forward to stealing my girls’ Kit Kats.
Love, YLE
“Your Local Epidemiologist (YLE)” is written by Dr. Katelyn Jetelina, MPH Ph.D.—an epidemiologist, wife, and mom of two little girls. During the day, she is a senior scientific consultant to several organizations. At night she writes this newsletter. Her main goal is to “translate” the ever-evolving public health world so that people will be well-equipped to make evidence-based decisions. This newsletter is free, thanks to the generous support of fellow YLE community members. To support this effort, subscribe below:







Thanks for the epidemiological update. It parallels what I’m seeing in my little primary care world. With the capacity to do rapid tests for Covid, Flu A + B, and strep, I’m really amazed by how much of these three are really out there this Fall. I’ve been seeing that steady churn of Covid that never seems to die, but surprised with a decent number of influenza B cases over the past month. I’ll trust the CDC maps, but I’m glad I got my flu shot a bit earlier.
If you don’t test, you don’t know. For example, 40 something female with sore throat, only gets a rapid strep test at urgent care, but tests positive. Treated with amoxicillin. I see her a couple days later for regular/chronic problems, and she’s not feeling better so I do the above… turns out she has influenza B and Covid! Unusual case but wow. Just because we have one doesn’t mean we can’t have other simultaneous infections. This is the first trifecta I’ve seen though. She’s doing well, thank goodness and vaccines, despite necessary immunosuppressive meds. Added paxlovid to amox, too late to treat flu.
My XBB booster has held up to at least one unmasked Covid exposure so far (bat mitzvah party I couldn’t in good faith mask for).
And yeah, stealing Kit Kats is one of those sacrifices we make so our children eat less sugar themselves. Scientists also suggest that we alleviate the York Peppermint Patty burden for our children’s sake.
👻
Nothing presented indicates we are turning a corner with covid. We’ll know more after January.
Regardless, we should expect covid to be with us indefinitely and that means the decorum of our social gatherings, especially during the holidays, has to change. Meeting with others indoors will always be a risky undertaking as long as we don’t take precautionary measures. How do you get the cooperation of the people your meeting with when there is no customary precautionary standard, such as with a group getting in a car together. No one has to ask anyone else to please fasten their seatbelt. We just do it. Similarly with covid, we need to establish a certain level of cooperation without anyone having to ask for it. It would make a welcome difference in the foreseeable future if social gatherers routinely took rapid antigen tests before coming together. Presently, it appears that we are succumbing to the lowest common denominator of peer pressure. We just cross our fingers and hope for the best.
Instead, we should come up with a hygienic customary practice to keep everyone safer when socializing.