After two years of politicized masks debates and antigen tests gaining traction, ventilation and filtration is finally gaining the spotlight it deserves. Improving indoor air is a powerful mitigation tool that has been underutilized throughout the pandemic. Some of the best public health interventions are those happening in the background: institutional-level interventions that work passively and invisibly on the individual level.
Sick building syndrome
The built environment’s impact on health was first documented in 1791 by an English physician who exposed children suffering from tuberculosis to sea air and sunshine in England. During the 1918 flu pandemic “stale air” was thought to be a breeding ground for viruses, and open air treatment hospitals were opened throughout the country.
In the 1970s, this concept grew beyond treatment techniques and “sick building syndrome” was officially recognized. This is a phenomenon that occurs when people’s health problems, like fatigue, itchy eyes, and headaches, are linked to time spent in a building. There are many causes of sick building syndrome, including chemical contaminants from inside (like carpets, copy machines), contaminants from outside (motor vehicle exhausts, plumbing vents), biological contaminants (mold), and… inadequate ventilation.
Since then, countless infectious disease outbreaks have been linked to indoor spaces. For example, a measles case study in China found that crowded office buildings were prone to large-scale outbreaks. In a seminal study, scientists infected participants with the flu and found transmission was much higher in poorly ventilated hotel rooms than in a research facility with much improved air flow. Another study found ventilation accounted for ∼50% of total removal of aerosol droplets of the flu in residential settings and ∼80% in public settings.
SARS-CoV-2
In the beginning of this pandemic, most were concerned about droplets of transmission, but scientists quickly learned that aerosol transmission was a main driver. The problem was that the WHO, CDC, and the public took a long time to shift perspectives. In July 2020, 239 scientists wrote a letter to the WHO indicating their concern about aerosol transmission. But it wasn’t until April 2021 that the WHO and May 2021 that the CDC changed their guidance to recognize airborne spread as a key mode of infection.
The difference between droplets and aerosols are size and its implications. Droplets are large (50-100 micrometers), and so they are heavier. Droplets can travel up to 6 feet, but then they fall to the ground due to gravity. This is why the famous 6 foot rule was implemented. People spread droplets by coughing and sneezing.
Aerosols, on the other hand, are much tinier (<5 micrometers) and lightweight, so they can become suspended in air and float. There are 100 times more aerosols than droplets. And you don’t need to sneeze or cough. These can be spread by just talking. Lab studies have shown that aerosols can stay in the air for up to 16 hours. So, hypothetically, a sick person doesn’t need to be in the room with you to transmit the disease. They could be in the room before you and left particles everywhere.
Research has shown that ventilation and filtration can do a lot for SARS-CoV-2:
A study last summer found that open windows in classrooms can have up to a 14.1 fold reduction in COVID19 transmission. This was highly dependent on the time of year (summer, spring, winter), number of windows, and how frequently those windows are open.
A Johns Hopkins study found that HEPA filters were responsible for a 65% drop in COVID-19 transmission.
Another study found that one HEPA filter is as effective as two windows partly open all day during the winter (2.5-fold decrease in transmission). Two HEPA filters are even more effective (4-fold decrease in transmission).
And, most recently, a data analysis in Italy found ventilation in schools can reduce the risk of infection up to 82%.
The NYT did a great job visualizing the impact of an open window and a fan/air cleaner below.
What can we do?
Individuals should advocate that their schools and workplaces improve ventilation. And, most importantly, that it’s done right. Unfortunately an investigation found that more than 2,000 schools across 44 states installed unproven devices during the pandemic that even had the potential of being a pollution source themselves. Here is a great 5 step guide to checking ventilation rates in classrooms.
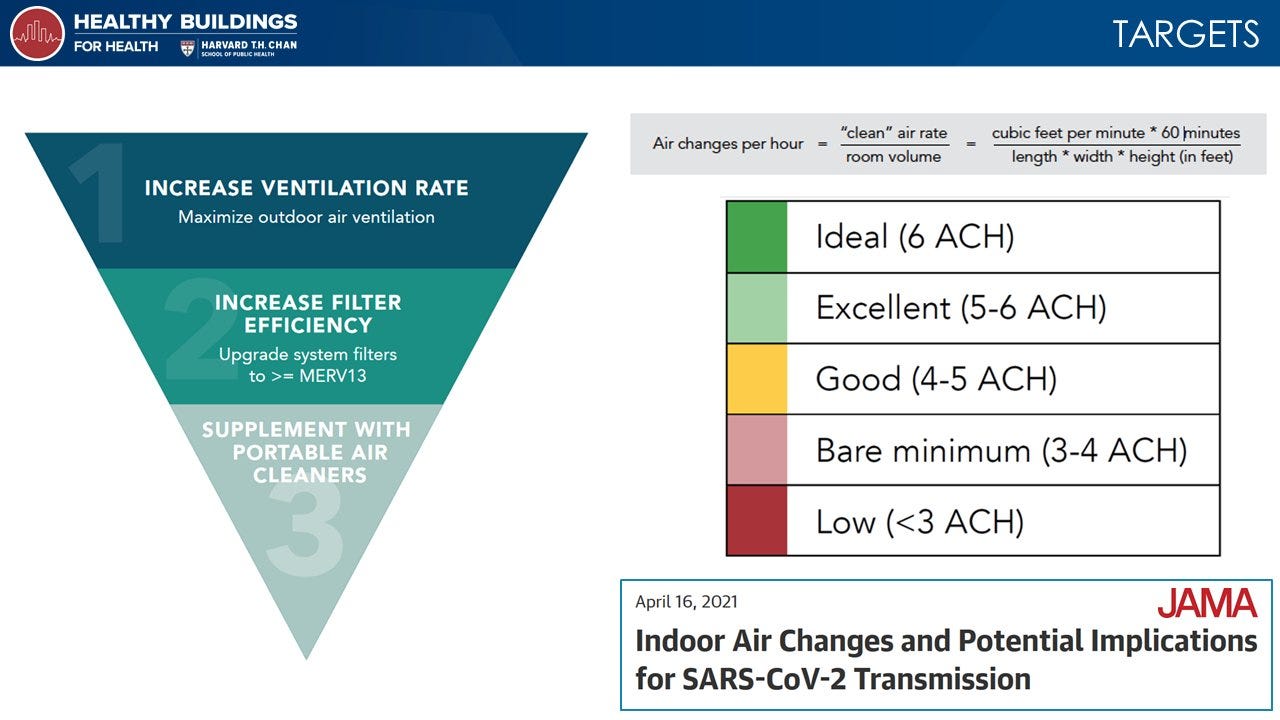
As a JAMA article pointed out last year, there are two things that building managers should focus on:
Improving air ventilation by bringing in clean outdoor air. Indoor air moves less than outdoor air, so viral particles hang in the air in greater concentrations. Ventilation can disperse viral particles.
Enhancing filtration to remove viral particles from indoor air. This is a great tool to supplement #1 or use if adequate ventilation isn’t possible (like opening a window is impossible).
This can be achieved by targeting 4-6 air changes per hour (ACH) in small volume, indoor spaces, like classrooms, homes, or work areas. (The 4-6 ACH threshold aligns with standards in hospitals as infection control strategies). As outlined in Harvard’s Healthy Buildings for Health website, though, the more ACH the better.
Improvements can be done three ways:
Outdoor air ventilation, like opening windows;
Recirculating air that passes through a filter with at least a minimum efficiency rating value 13 (MERV 13) rating; or
Passage of air through portable air cleaners with HEPA (high-efficiency particulate air) filters.
But, like every mitigation measure, ventilation is not perfect. This is especially true when transmission happens in droplet form (if you’re 6 feet from someone). But this is where a mask comes into play. The physical space really matters too. For example, places where people aren’t wearing masks uniformly, like restaurants, or places with high density should increase target ACH’s. Places with high ceilings, like gyms, should use another metric (not ACH) to measure adequate ventilation.
Pandemic preparedness
Last September, “improved indoor air quality” was included in the American Pandemic Preparedness Plan. This month, the Environmental Protection Agency launched the Clean Air in Buildings Challenge, which includes a practical guide for business and homeowners to create an action plan for cleaner indoor air. Yesterday there was even a 2.5 hour webinar hosted by the White House Office of Technology and Science Policy about this topic. Over the decades, we’ve worked so hard on improving the water we drink that it’s now time for policy to focus on improving the air we breathe.
Bottom line
We are far better off when we layer all mitigation measures. This is an individual-level responsibility (like wearing masks, using antigen tests to break transmission chains), but also an institutional-level responsibility for businesses, schools, and churches. Preparing buildings now will not only help with SARS-CoV-2 but other health problems for decades to come.
Love, YLE
“Your Local Epidemiologist (YLE)” is written by Dr. Katelyn Jetelina, MPH PhD—an epidemiologist, biostatistician, professor, researcher, wife, and mom of two little girls. During the day she has a research lab and teaches graduate-level courses, but at night she writes this newsletter. Her main goal is to “translate” the ever-evolving public health science so that people will be well equipped to make evidence-based decisions. This newsletter is free thanks to the generous support of fellow YLE community members. To support the effort, please subscribe here:






So, how can you know if have good ventilation? A CO2 meter will tell you this! CO2 from exhaling builds up in the air. Ambient air is 420 ppm (should be 280, but fossil fuels...) Great ventilation is 600 or lower. Good up to 800. Acceptable up to 1000.
I have an Aranet4. It fits in your pocket. Runs for a year on 2 AA batteries. Has app that connects to your phone via Bluetooth.
Some things I've found... my local supermarkets runs 800-1000 depending on the crowd. Big box home improvement stores about 600. Hotels... 1000-2000 in the rooms, but those aren't "shared air". Airports - 600s in common area like security, 900s in gate lounges. On plane >1000 - but this air is 100% HEPA filtered.
Home HVAC systems rarely have any external ventilation - beware! Your house may have the lowest air quality of anywhere you go.
An cheap DIY alternative to a portables HEPA filter is the Corsi-Rosenthal box. You can make one our of a box fan, MERV 13 furnace filters and duct tape. Higher clean air delivery than many portable HEPA filters. Google it and you'll find tons of instructions and videos.
We can all thank the "aerosol warriors" for finally winning this battle. They had a hard, upstream battle before the medical community accepted what these engineers knew.