This week ACIP—CDC’s external advisory group of scientists—met to discuss all vaccines. This was part of their regularly scheduled meeting (i.e., these happen with or without a pandemic). This morning they focused on COVID-19 vaccines.
This discussion was much anticipated because it follows the VRBPAC meeting in which the FDA discussed the future of boosters in the U.S. We had a lot of unanswered questions following that meeting.
Overall, I was pleasantly surprised on the range and depth of data presented today. There were a lot of golden nuggets.
Here are your Cliff notes.
Vaccines continue to be safe
Reassuring data on the safety of COVID-19 vaccines was presented. I won’t go through all of it because there was a lot, but I will highlight one thing: temporal scan results. I hadn’t seen this before, and it’s pretty cool.
The CDC looks at real-time adverse events and maps them over time. They have a system that finds abnormal clusters. This helps because random events happen all the time. These clusters are designed to be very sensitive; they cast a wide net to find the smallest of signals. This comes with a trade-off, though—we may see things that happen by chance alone.
This is what may have happened with the stroke signal found after bivalent vaccine among those over 65 years. They saw a cluster, but then the cluster receded. The other monitoring systems didn’t find anything.
This is just another example of how many people and how much data go into ensuring these vaccines are safe.
Vast majority of COVID hospitalizations are “for” COVID-19, still
Critical data on hospitalizations “for” (primary reason) and “with” (coincidental) COVID-19, by age and over time and chronic conditions, were presented. I also hadn’t seen this data before. The vast majority of COVID-19 hospitalizations (80-90%) for those under age 5 years or over 50 years are “for” COVID-19. This hasn’t changed over time. So, yes, COVID-19 is still a problem.
Among adults hospitalized for COVID-19, 96% had at least one underlying condition. Among kids hospitalized, 49% had no underlying health conditions. Among those with underlying health conditions, the driving force differed by age: prematurity for those under 2 years and asthma for those 2-17 years old.
Risk-benefit for adolescents still favorable, but getting tighter
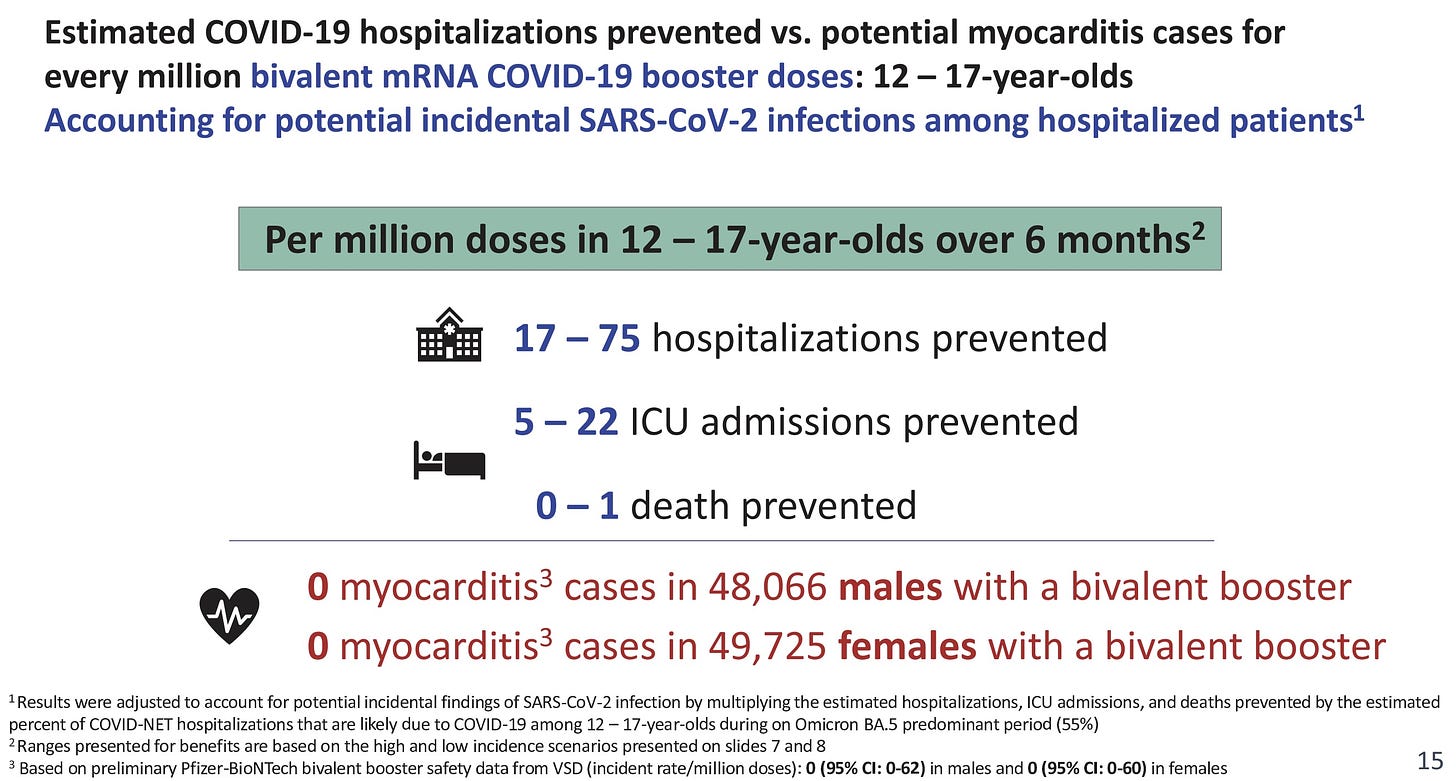
There has been a LOT of chatter around whether the benefits of COVID-19 vaccines still outweigh the risks for adolescents, in whom myocarditis is a rare but real risk. The CDC ran a risk-benefit analysis on bivalent boosters. I’ve been waiting on this for a long time. It didn’t disappoint.
Per 1 million bivalent vaccines given to 12-17 year olds:
Benefits: 17-75 hospitalizations “for” COVID-19; 5-22 ICU admissions “for” COVID-19; and 0-1 deaths prevented
Risks: 0 cases of myocarditis
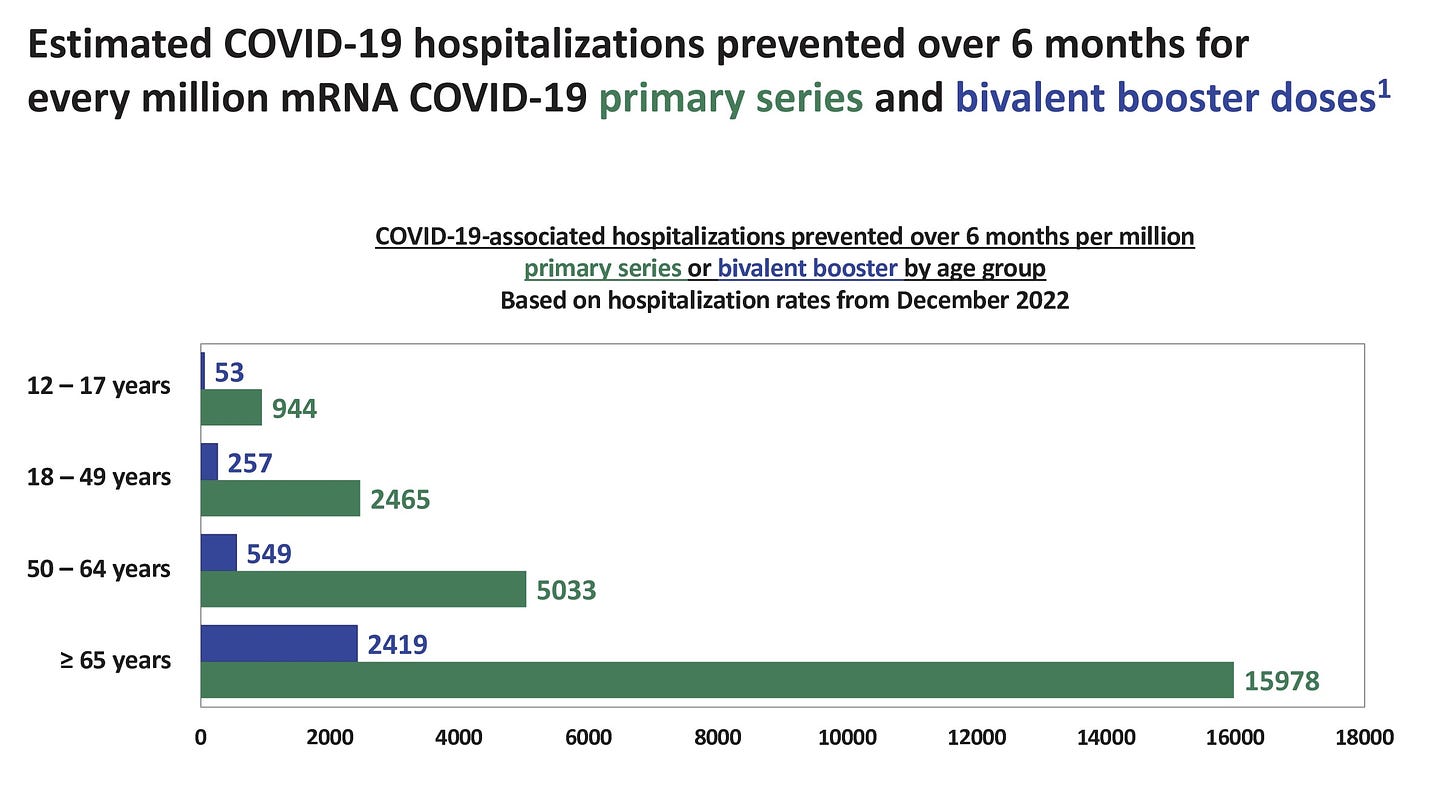
So benefits still outweigh risks, but it’s getting tighter compared to the primary series.
Look at the small print in the slide above. No data is perfect, so the “true” number of myocarditis cases could range from 0-122 (males=62 and females=60). This means 122 myocarditis events per 1 million doses is a worst case scenario. This means there could be future scenarios in which risks outweigh benefits for adolescents.
BUT, keep in mind two things:
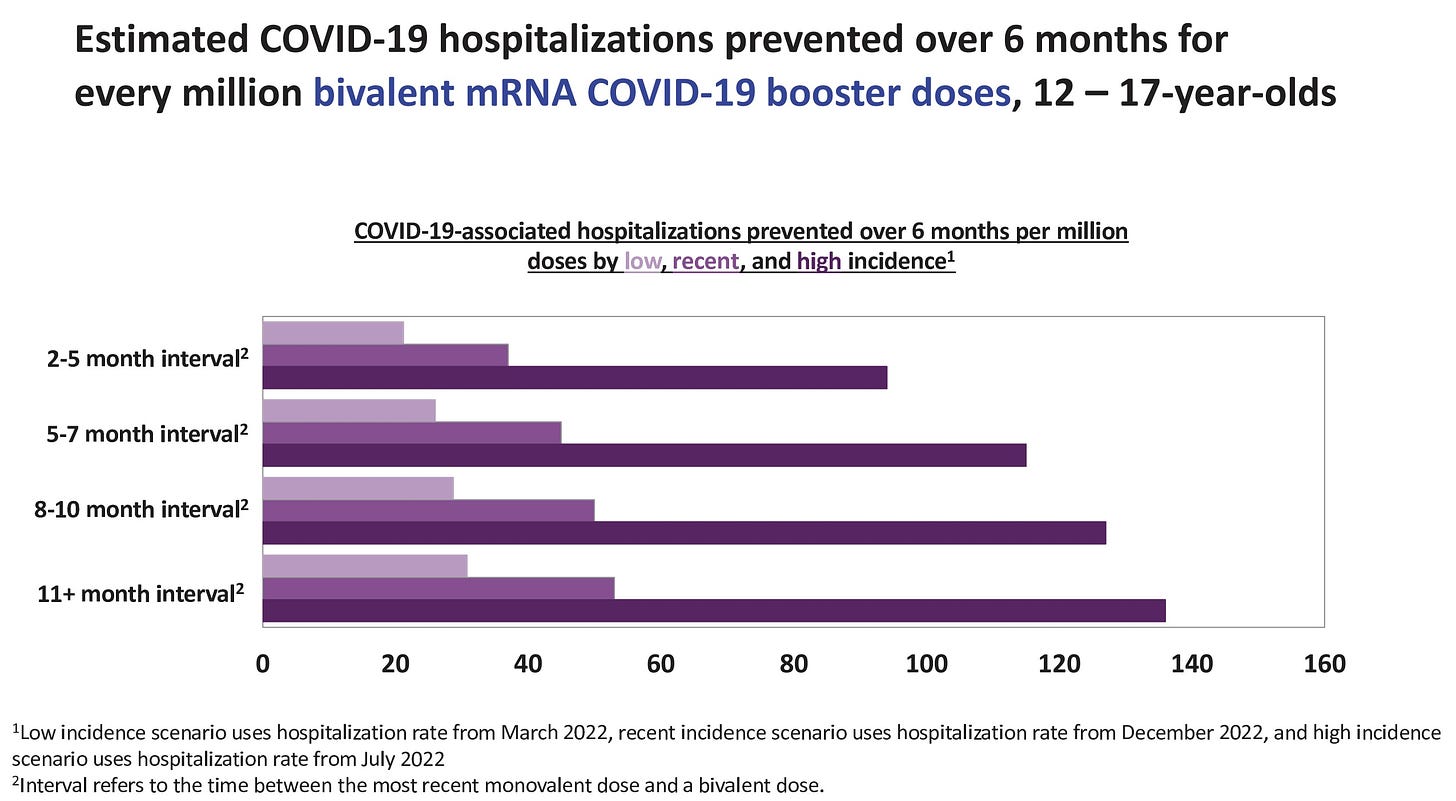
These data are based on a snapshot in time. Specifically, the numbers above are based on what we saw this winter, which was a relatively quiet time for adolescents and COVID-19. If we see a future surge, on the other hand, the benefits would immediately increase. Increased time between doses also increases benefits. We can see that in the slide below.
The benefits described above are limited to severe disease; other benefits may include prevented infections, long COVID-19, days of work missed, reduced transmission, etc.
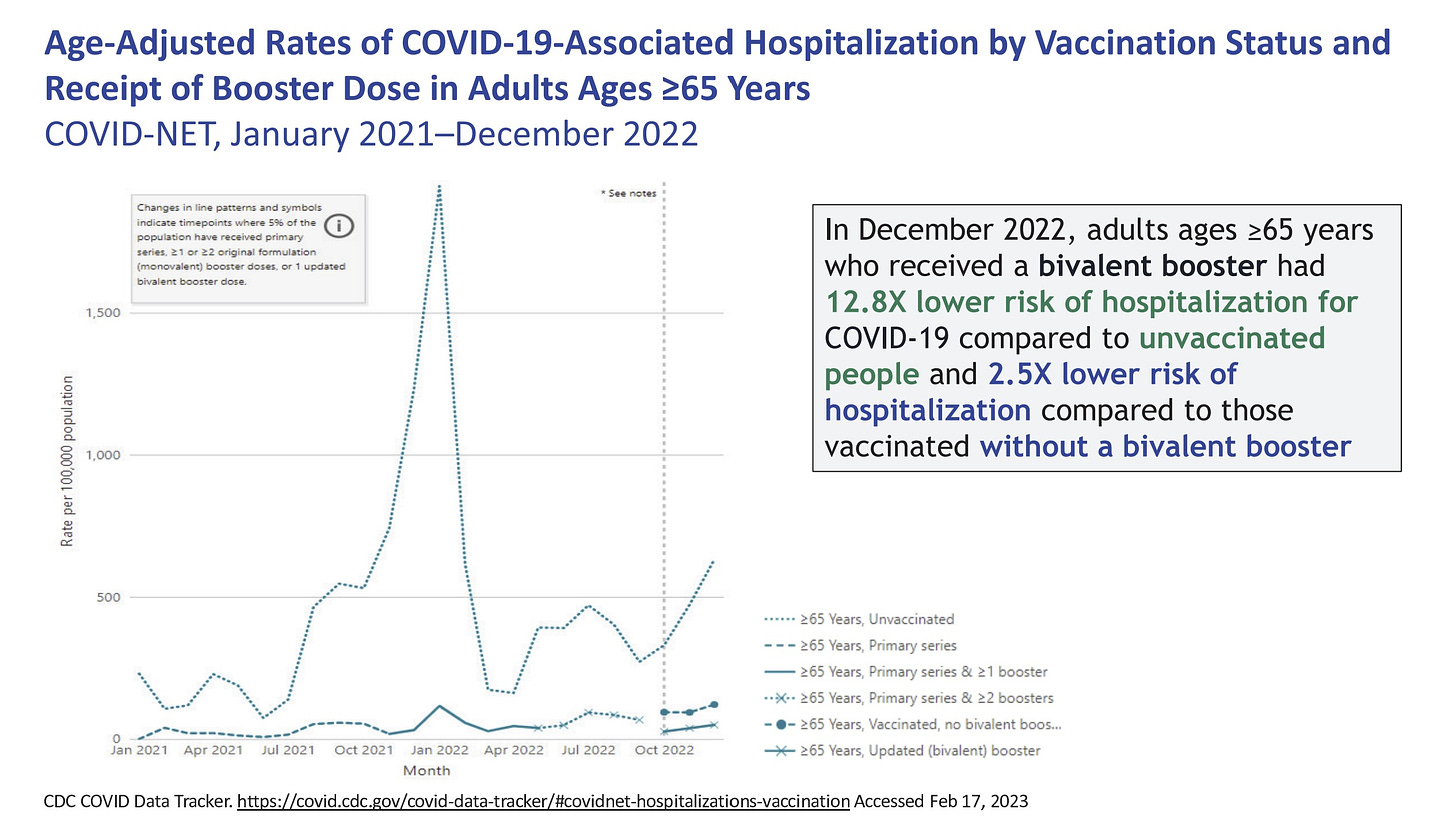
The CDC conducted risk-benefit analyses for all other ages, too. There is no question that vaccines still greatly outweigh risks for adults, especially for those over 65 years.
Everyone gets one shot per year
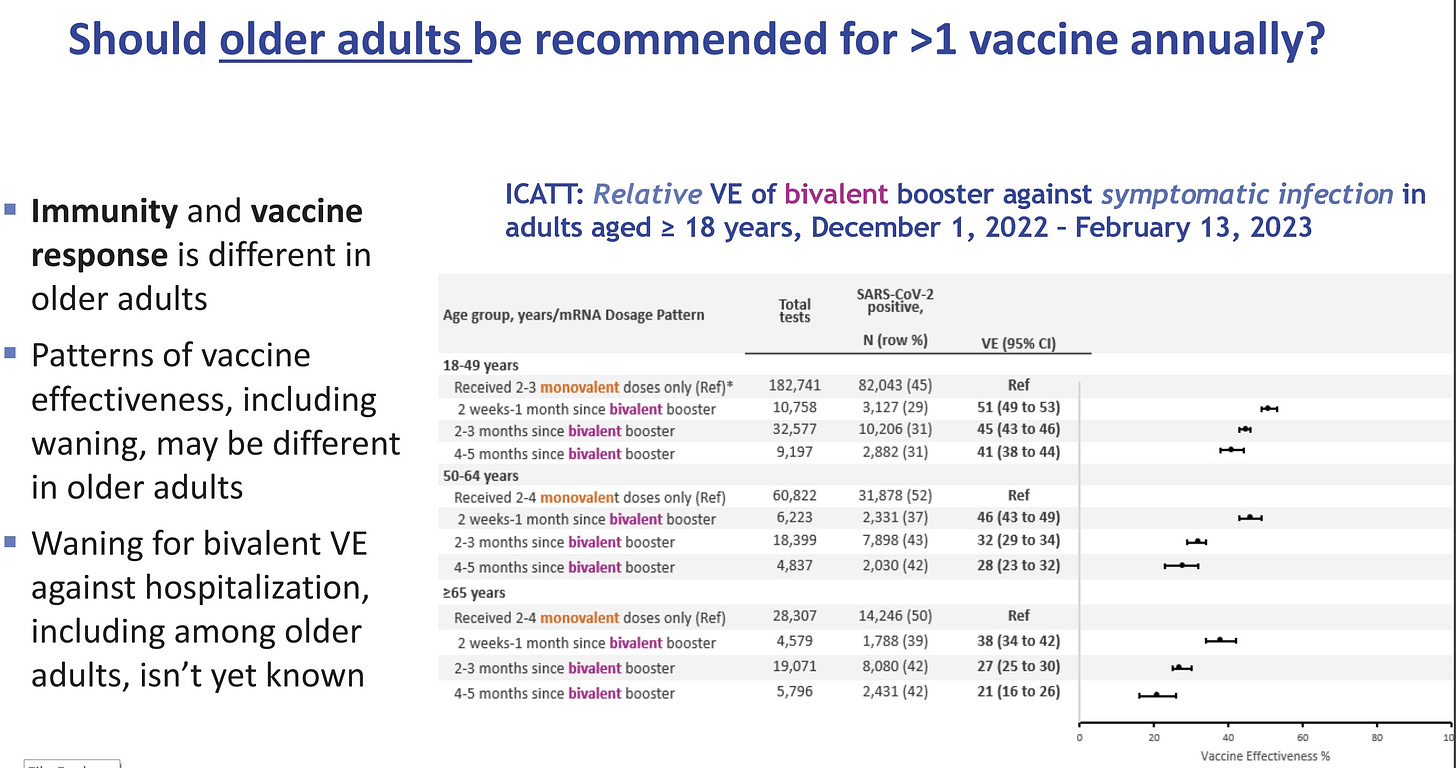
Older adults who were vaccinated in September are coming up on 6 months post-vaccine. Do they need another vaccine? Or do they wait until fall like everyone else?
Data on protection against infection by age was presented. It’s clear that this protection wanes and more so among older adults.
But bivalent vaccines continue to be very protective against hospitalizations. (There has not been enough time to see waning).
CDC further clarified the goal of the vaccine program: Prevention of severe disease.
Because of this, ACIP decided there was “insufficient evidence” to suggest older adults need another bivalent dose at this time. They did say this could change in the future based on three things:
Hospitalization rates among those who got the bivalent start to increase
Other signals of waning vaccine effectiveness of bivalent vaccines
SARS-CoV-2 significantly mutates
They did a similar evaluation for immunocompromised. And came to the same conclusion.
So, as of now, everyone will be eligible for one shot a year. We will need to be flexible, as this may change. Is this the right call? Time will tell.
Bottom line
Today’s meeting was super helpful. But we have to find a way to get data and analyze it more quickly in the U.S. It will help combat misinformation, improve confidence in vaccines, and improve confidence in public health overall. This should be our number one priority.
Have a great weekend, YLE
“Your Local Epidemiologist (YLE)” is written by Dr. Katelyn Jetelina, MPH PhD—an epidemiologist, data scientist, wife, and mom of two little girls. During the day she works at a nonpartisan health policy think tank and is a senior scientific consultant to a number of organizations, including the CDC. At night she writes this newsletter. Her main goal is to “translate” the ever-evolving public health science so that people will be well equipped to make evidence-based decisions. This newsletter is free thanks to the generous support of fellow YLE community members. To support this effort, subscribe below:







Enormously grateful to Dr. Jetelina, yet once again, for her dedication to and brilliance at clear public-facing communications. Here’s what take from this, for those of us who need to stay clear of infection (older, immunocompromised):
>the data do not seem to support the idea that one booster per year is sufficient for us. I recognize that the CDC’s approach is focused on avoiding hospitalization, but as an older couple, who, like we did, got a rough case of Covid that was debilitating for a month+, said, “who wants to be this sick?”
>this also suggests to me that older and immunocompromised folks will continue to be sidelined much more than others in the ability to live some semblance of even Covid era normal life, even though we are a VERY large and growing group.
Am I missing something here? If anyone else has a thought on this, I would welcome it.
“CDC further clarified the goal of the vaccine program: Prevention of severe disease.” Sure glad we didn’t just have “prevention of severe disease” for polio, small pox, measles, etc. I am disappointed with that low bar goal. It should be to develop better vaccines that can eliminate this damaging disease.