Today the ACIP met to discuss two important topics: myocarditis and booster shots. This meeting was originally scheduled for last Friday, but then was postponed due to the new federal holiday.
Here is the agenda. Here are the PowerPoint slides. And here are your cliff notes…
Myocarditis
Myocarditis (or inflammation of the heart) has been at the forefront of the adolescent vaccination conversation. For more background, check out my two previous posts here and here. For this meeting, we needed a few key questions answered:
What are the case details?
There are now 484 cases of myocarditis following vaccination among people <30 years old in the United States. Among the 484 patients, 67% (or 323 cases) had been fully investigated by the CDC. Among the 323 investigated cases…
96% (309 patients) were hospitalized
295 of these patients have been discharged from the hospital. 79% had full recovery of symptoms
9 were still hospitalized at the time (2 were in the ICU)
The majority of symptoms popped up, on average, 4 days after vaccination
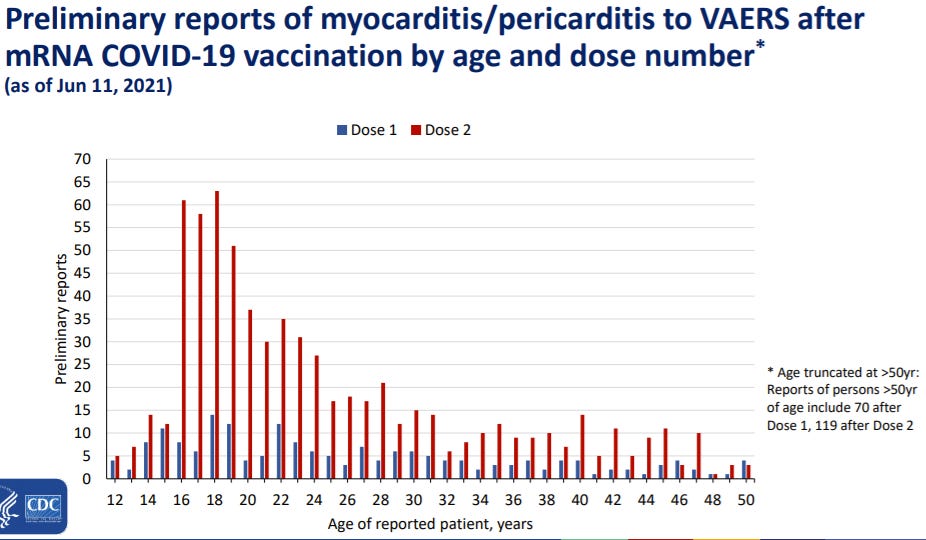
Myocarditis is higher among males and higher after the second dose
What is the biological link?
This is extremely important question to answer, as it could give us an idea of causality (i.e. does the vaccine cause myocarditis). Also, it would give us an idea of long-term impact of vaccine-induced myocarditis.
During this meeting, it was clear that we don’t know why this is happening. But, it’s being actively explored. There were a few hypotheses that were acknowledged during the discussions with some preliminary answers:
Does it have to do with the spike protein? Probably not. The spike protein antibody was negative in some patients.
Is this due to active or prior COVID-19 infection? Doesn’t look like it. Only 10% of cases have had a prior infection.
Is it due to the immune response (also known as a cytokine response)? Especially since this reaction is more common after the second dose? We don’t know yet, but this is a valid possibility.
Why male dominance? There are sex differences between the number of receptors on the heart for males compared to females. Could this play a role? It’s plausible but needs further investigation.
Because we don’t know much, we don’t really know the long term outcomes of these patients. But, among patients that had severe COVID-19 disease (myocarditis with MIS-C), 3- and 6-month follow-ups are looking okay. Which is comforting because this likely reflects healing for vaccine-induced myocarditis.
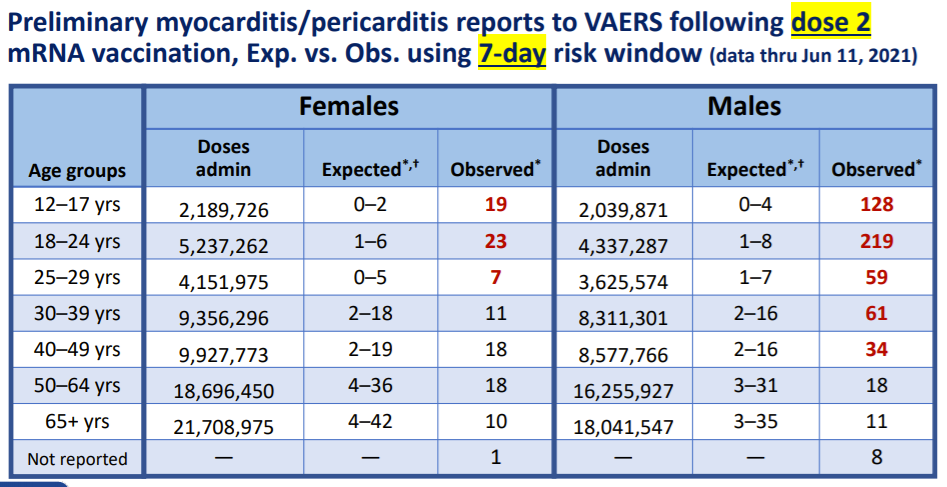
Is the rate of myocarditis after vaccination (i.e. observed) higher than the rate of myocarditis in the background (i.e. expected)?
Yes. The observed rate is higher than the expected rate. So, myocarditis is probably due to the vaccine.
There is good news though. We expect 4-6% of people to die from myocarditis. We haven’t seen that death rate of vaccine-induced myocarditis, which is encouraging.
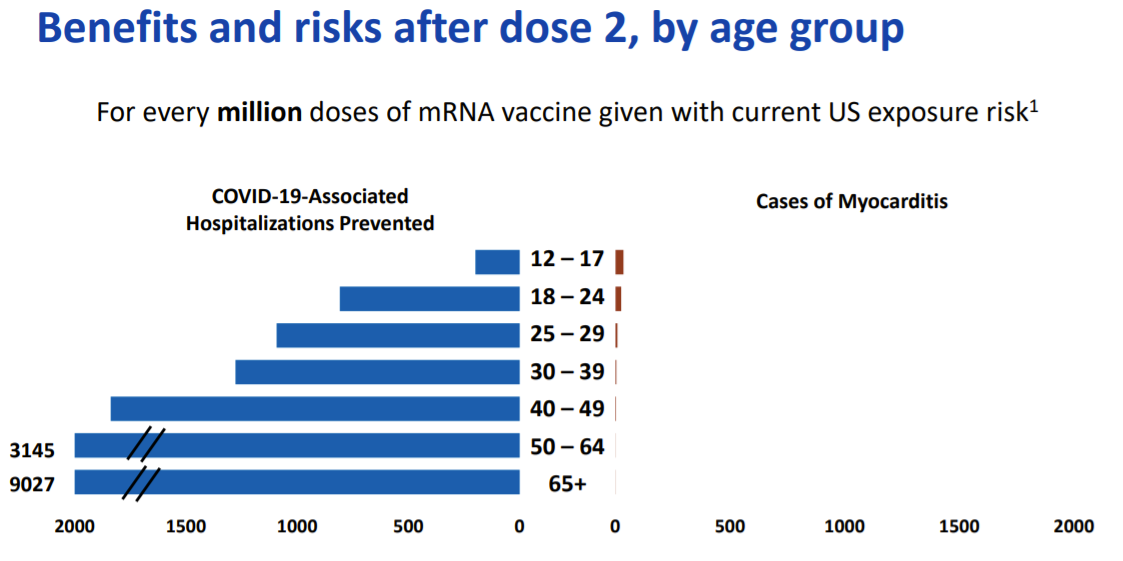
Does benefit outweigh risk?
Yes, the benefits still clearly outweigh the risks for COVID-19 vaccination in adolescents and young adults.
COVID19 is still very much a risk. And there have been 133 million vaccine 2nd doses administered and 636 reported myocarditis cases as of June 11, 2021.
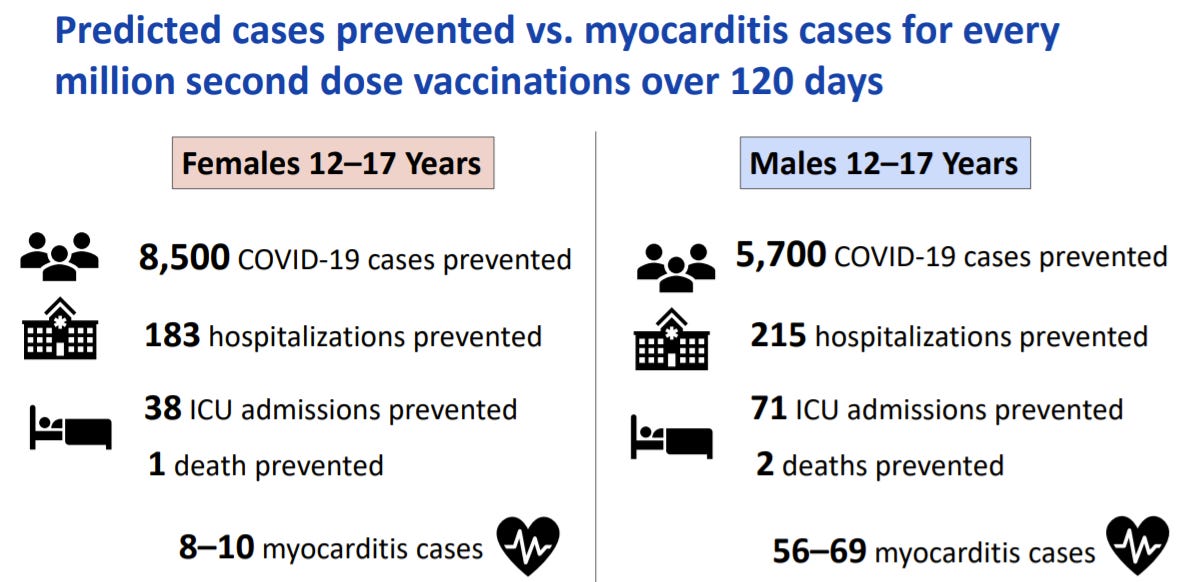
The CDC also ran some future projections. For every 1 million vaccinations among males aged 12-17, 5,700 COVID19 cases will be prevented, 215 hospitalizations prevented, and 2 deaths prevented. On the other side, for every 1 million vaccinations, there would be 56-69 myocarditis cases.
Booster shot
There was one presentation at the end, presented by Dr. Sara Oliver, that summarized the current data of booster shots. There were two questions they answered:
Do we currently need a booster shot? No. Vaccines are working well against all variants (including Delta).
Will we need a booster shot? We don’t know yet. Boosters may be needed for entire population. But they may be only be needed for specific populations (like immunocompromised, healthcare workers, or long term care residents).
We are paying attention. There will be a lot of studies coming out in late Summer and early Fall that will tell us more. But it’s clear that booster doses would only occur after:
Evidence of declining protection against illness, such as declines in vaccine effectiveness, not only waning antibody response
An escape variant
Hope this helps begins to answer some of your questions!
Love, YLE





What happens if we get to a point where the collective risk-benefit analyis says one thing but the individual risk-benefit analysis says something else?