The fall/winter season always means more respiratory sickness—the weather changes, people head inside, and social networks change (school starts, holiday celebrations occur). But the last four years have resulted in very unusual patterns.
This makes predicting this season a fool’s game. But I’ll take the bait and give it a shot.
What makes predicting challenging?
Three main factors:
Many scientists agree that SARS-CoV-2 still hasn’t settled into a predictable, seasonal pattern. BA.2.86 is an excellent example.
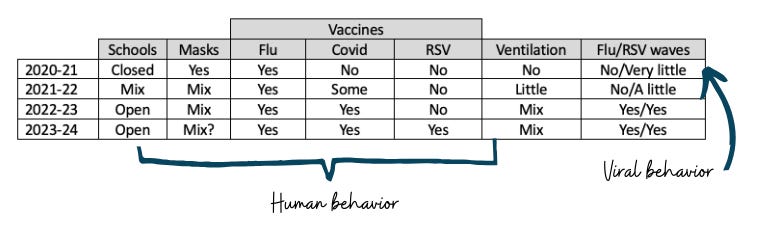
Changing human behavior: The changing immune landscape, new and improved tools, and pandemic fatigue have meant that human behavior has changed drastically from season to season, as I outlined in a rough table below. Human behavior plays into viral patterns.
Perplexing viral behavior: Other viruses’ timing seems to be off. One hypothesis is viral-to-viral interaction—one virus takes over, then subsides, and another virus wave begins due to population-level immunity to the first virus. For example, last year, we were concerned about a triple-demic—all three viruses peaking simultaneously and flooding our hospital systems. Interestingly, they didn’t, which helped immensely. (Viral-to-viral interaction? Maybe—we’ll see what happens this year.)
But I think this season will be the first time we have a repeat in behavior (except for the RSV vaccine availability) and all three viruses present.
So, my guess: this year’s patterns will broadly mirror last year’s.
So what happened last year?
RSV arrived earlier than usual (peaking in early November) and with a vengeance, particularly among children under 5. Our pediatric hospitals were overwhelmed, to say the least.
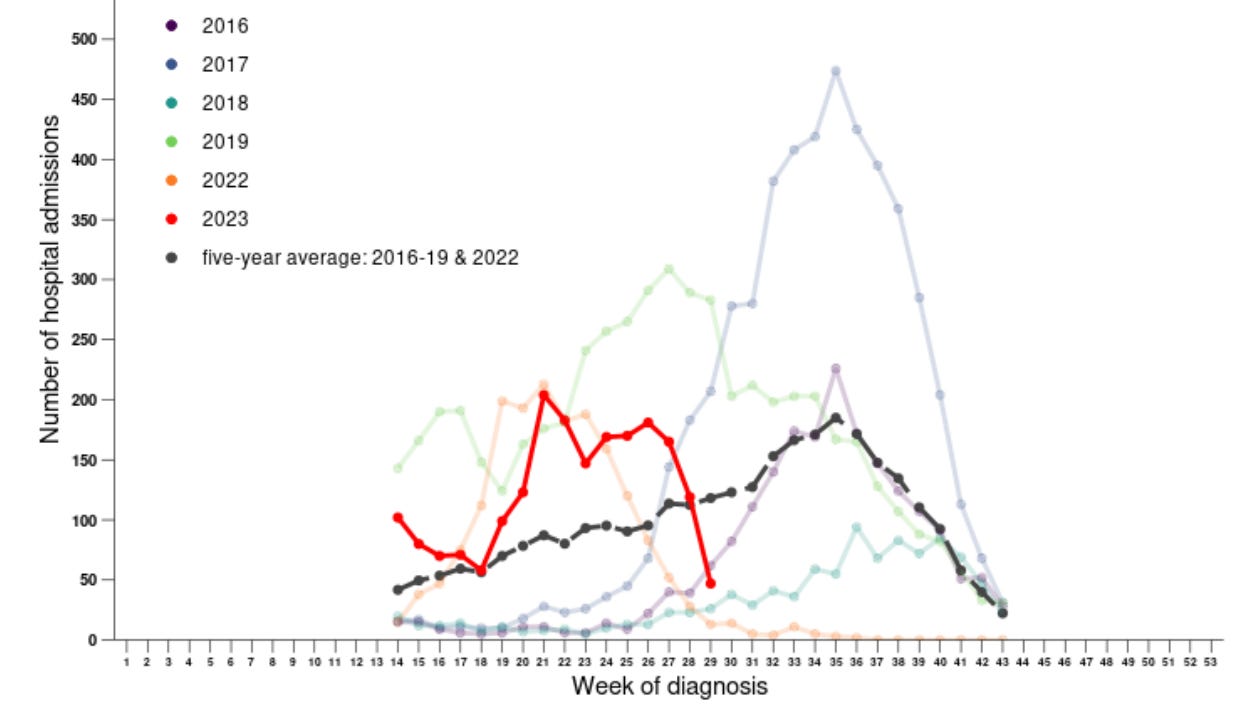
Flu also came earlier than usual, peaking around mid-November. (Pre-pandemic it peaked in mid-January.) But last year’s wave was about the same height as pre-pandemic.
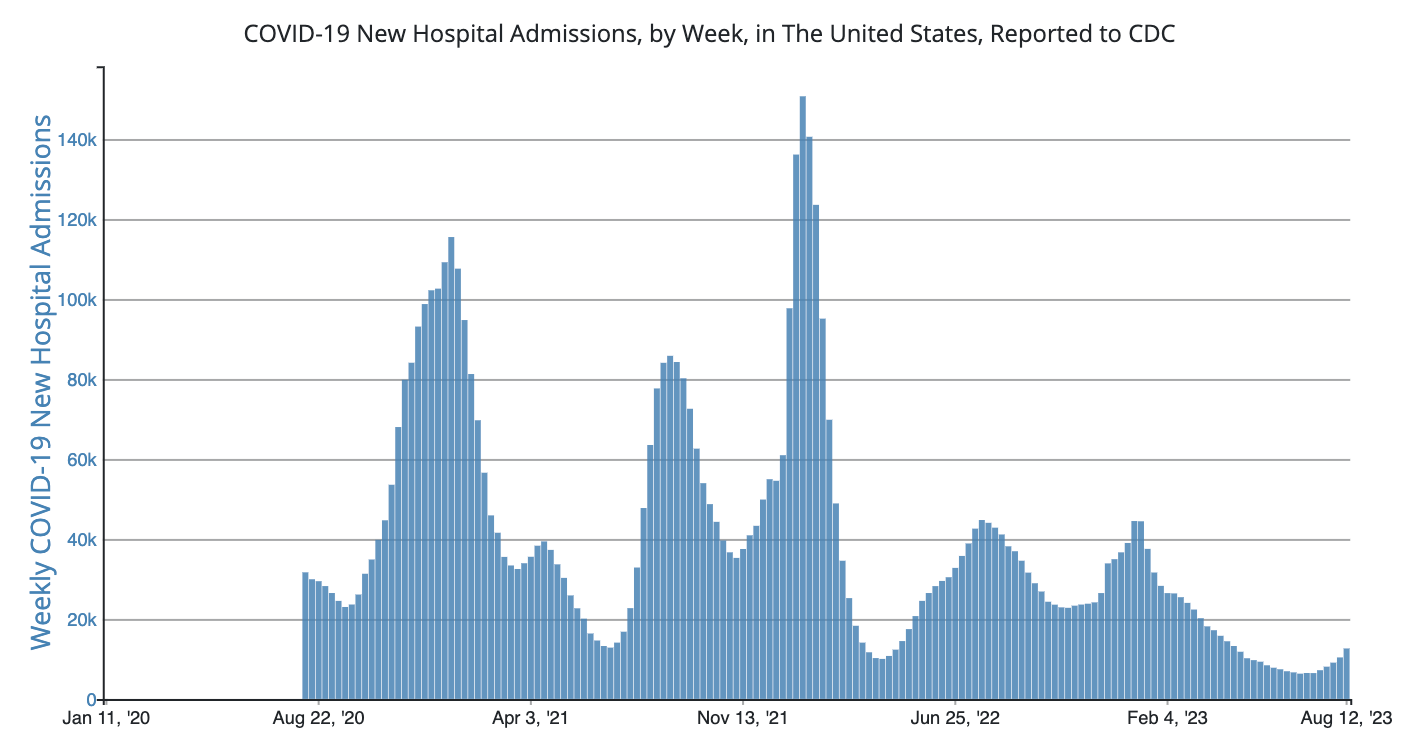
COVID-19 had a middle-of-the-road year. In other words, hospitalizations weren’t as bad as before but still had a sizeable impact.
Of course, BA.2.86 on the scene complicates fall/winter predictions. The COVID-19 Modeling Hub—8 academic teams across the U.S.—made projections before BA.2.86 was identified but took this kind of scenario into account:
If BA.2.86 explodes, we likely see closer to scenario F
If BA.2.86 fizzles, we likely see scenario E
This means we should expect to lose 55,000 (optimistic model) to 450,000 Americans (pessimistic model) over the next two years.
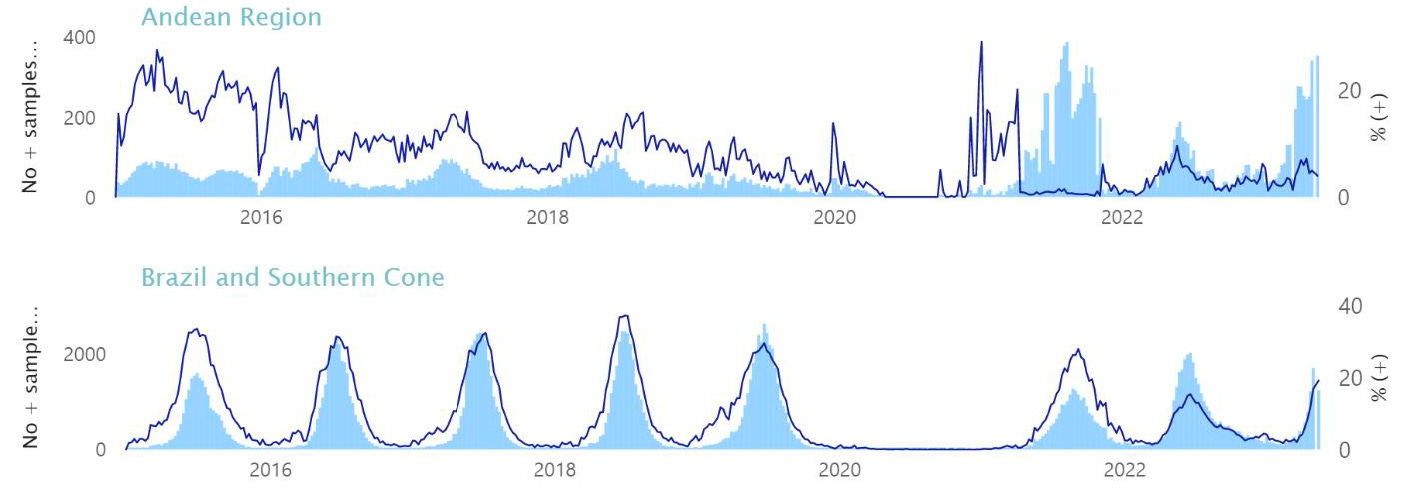
What happened in the Southern Hemisphere?
The Northern Hemisphere has an advantage in predicting upcoming seasons—Southern Hemisphere data. Their respiratory season occurs before ours, so we can look to their winter season to predict ours.
This year’s Southern Hemisphere respiratory season looked a whole lot like last year's:
In South America, RSV made huge waves, just as high as last year.
Flu hospitalizations in Australia were as early and about as high as 2022.
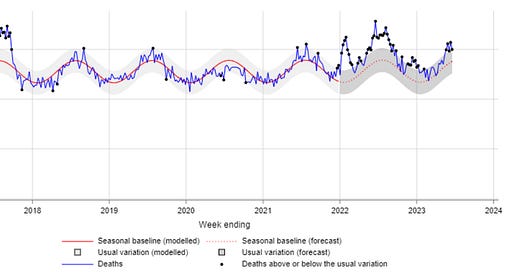
Excess deaths in Australia continue to tick up from pre-pandemic levels.

Bottom line
I wouldn’t be surprised if the Northern Hemisphere saw a repeat of last year: an early RSV wave, followed by an early flu wave, and COVID-19 finishing us off. But of course, predicting patterns only 4 years into a novel virus is a fool’s game.
Regardless, we know viruses are coming. Their wave height depends heavily on how we utilize our tools, like vaccines, ventilation, medications, and masks. Let’s consider using them.
Love, YLE
“Your Local Epidemiologist (YLE)” is written by Dr. Katelyn Jetelina, MPH Ph.D.—an epidemiologist, wife, and mom of two little girls. During the day, she is a senior scientific consultant to several organizations. At night she writes this newsletter. Her main goal is to “translate” the ever-evolving public health world so that people will be well-equipped to make evidence-based decisions. This newsletter is free, thanks to the generous support of fellow YLE community members. To support this effort, subscribe below:








I saw a school in Kentucky has already shut down due to high levels of staff and student illness:
https://www.today.com/health/news/kentucky-school-district-cancels-classes-covid-flu-strep-rcna101536
https://www.wkyt.com/2023/08/24/multiple-ky-schools-close-due-illness-start-new-year/
Oh, I guess it’s multiple Kentucky schools now.
As someone immunocompromised for fall for the first time and *still* recovering from my very first COVID case (caught from 2 family members coming into my house, one with symptoms not disclosed til the end of the visit.), I’m dreading the Fall and hoping I survive it. Very thankful for Paxlovid. I have no doubt I would be hospitalized otherwise.
Masking absolutely works. I masked through all other exposures (including as a hospital nurse with COVID patients) and came out negative. So since there are no accommodations for working from home at my company, I’m just going to be wearing the best masks I can find starting now.
As a communicable disease nurse, it’s going to be a very busy and probably ugly winter. The politicization hasn’t toned down at all. I suspect the uptake of vaccines to be fairly abysmal other than the older folks. I hope I’m wrong. With other opportunistic infections like invasive strep stepping on the coattails of our damaged immune systems, this could be a lot of heartache. I wish we could all just take common sense precautions instead of running headlong into a hurricane to prove a point.
Good forecast, and for what it’s worth I agree. I’m guessing Covid “wave” first this fall with BA.2.86 since it’s by far the most contagious (of these 3 viruses), and booster uptake will be low and less effective than if we had a more closely matched vaccine. Not vaccine makers’ fault.
And I enjoy not being sick, so I’ll be wearing that N95 I never stopped wearing in higher risk situations.
When I get Covid I want it to be “worth it.” Family gathering instead of public bathroom kind of thing.
And I’ll be taking paxlovid, or oral remdesivir once it arrives.