Disclaimer: I am now engaged as a consultant for the CDC to strengthen scientific communication in the United States. I’m beyond happy CDC has recognized this gap, and I’m honored to play a small role in the solution. I helped with the report discussed below.
Until now, the CDC has relied on Morbidity and Mortality Weekly Report—an internal scientific publication journal—to communicate COVID-19 science throughout the pandemic. But this pipeline is too slow for crisis communication. We need rapid analyses to guide evidence-based decision-making.
The WHO and countries like the U.K. have used technical reports throughout the pandemic to publicly share data they were seeing in real time, even if imperfect. This achieves many goals (transparency, proactive communication) but also allows for laser focused, data-driven strategies for innovative problem solving. The CDC leveraged technical reports (eventually) with monkeypox. It’s about time we use this strategy with COVID-19, too.
This week, CDC released their first COVID-19 Technical Report. This report provided a key puzzle piece we’ve been missing throughout the pandemic: Who is dying? Answering this question is the first step in moving the increasingly stubborn needle of COVID-19 mortality in the U.S. (We still have excess death and COVID-19 is still poised to be the 3rd leading cause of death in 2022.)
Below are a few key findings that I pulled from the report.
Signs of improvement
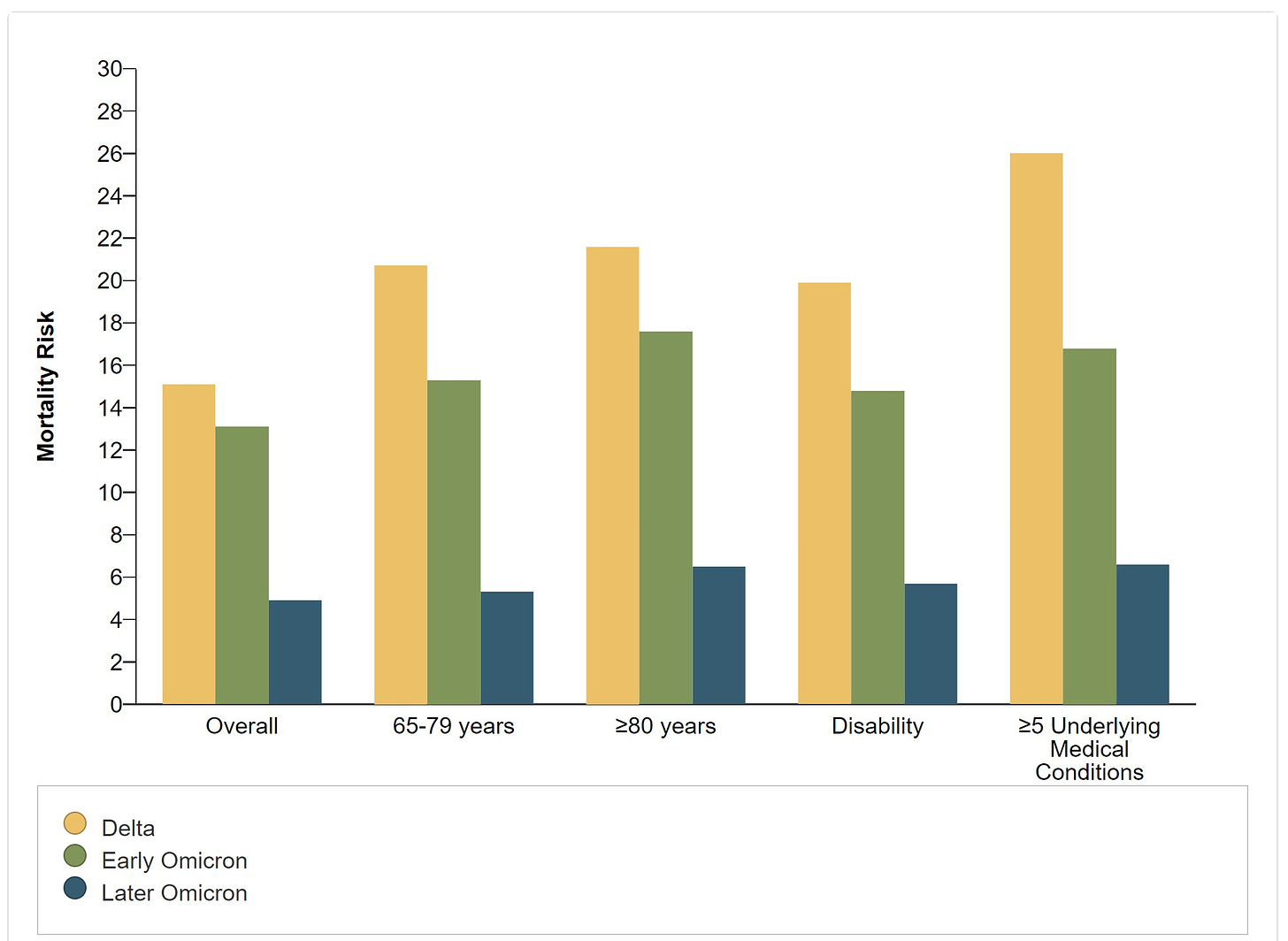
Fewer people are getting severe disease from infection. People who are hospitalized are now less likely to go to the ICU or be put on a ventilator—both metrics have more than halved since Delta. This means the risk of death has significantly declined. This is great news and unsurprising (although I was surprised how much this changed from early Omicron to later Omicron).
A shift in who is dying
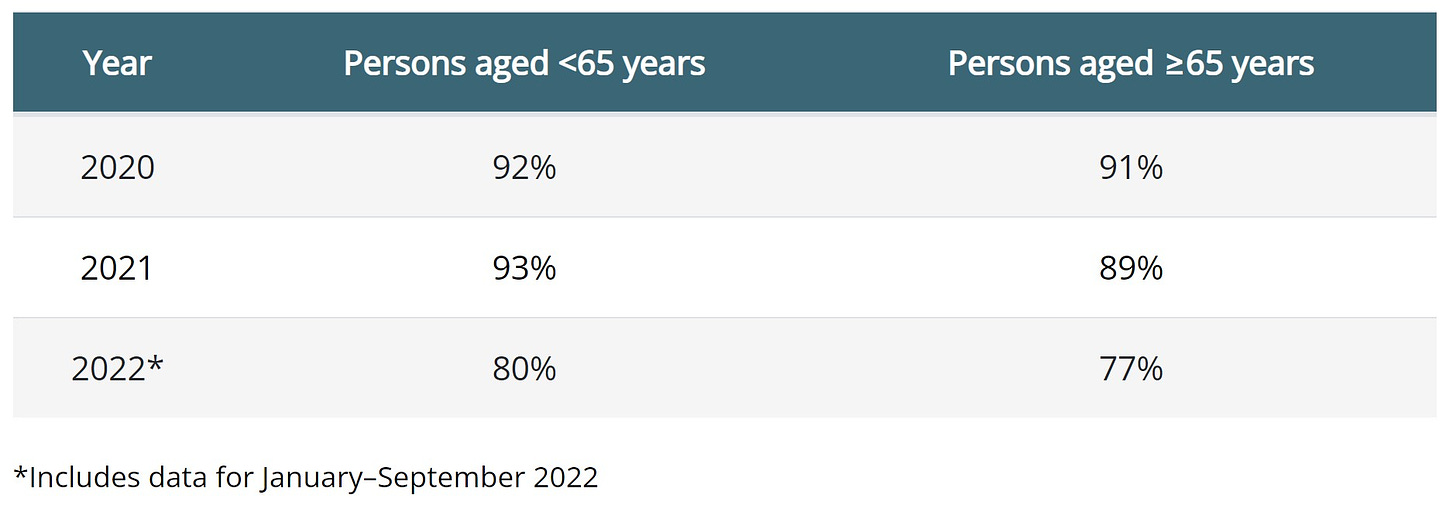
Age. Those 65 years and older are contributing more and more to the proportion of deaths over time. This is likely due to a few things: younger people are now vaccinated; older people have weaker immune systems; and older people are more likely to have comorbidities. Targeting communication and resources to older adults will be key to further reducing mortality.

Sex. Men are still dying more often than women. There may be some hormone and genetic factors at play here. (Also, men, go to a doctor if you feel sick.)
Race/ethnicity. Disparities have narrowed. Among those under 65, mortality is highest among American Indian/Alaska Natives. Among aged 65 and older, it’s highest among Non-Hispanic White. These demographics shift frequently, though, as differences are small.
Vaccines are effective if you’re up-to-date
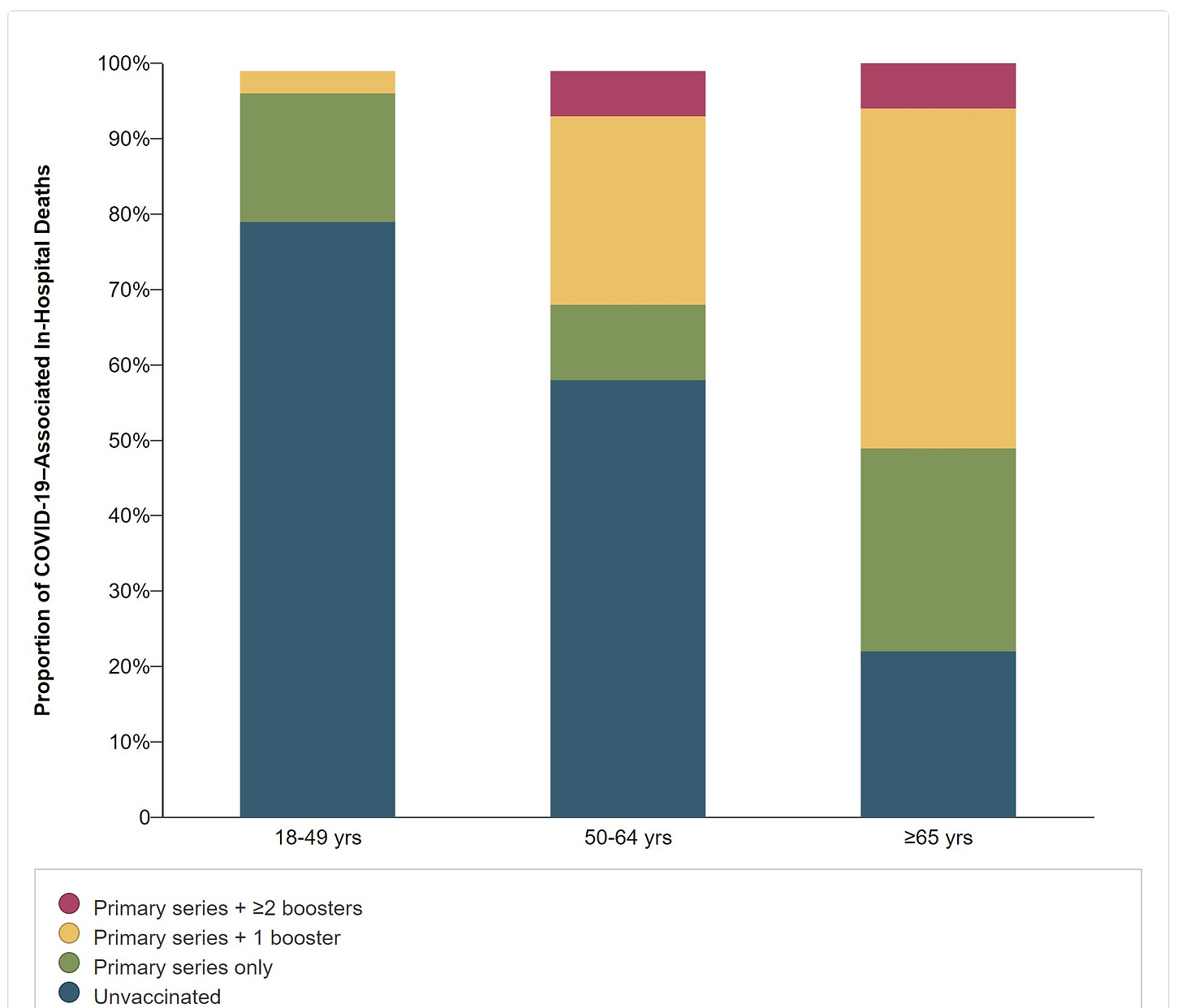
Vaccines have saved countless lives. However, it’s increasingly clear that those over 50 must be up to date. Today, 1 in 2 deaths among those over 65 had one booster. (While ~5% of adults 65 and older remained unvaccinated, they comprised 22% of deaths—a disproportional amount.) Given that only 29% of older adults have their Fall booster means we have a lot of work to do.
Shifts in where and how deaths occur
Yes, people are still dying from COVID-19. In fact, the vast majority of deaths have COVID-19 listed as the underlying cause of death. This is opposed to a contributing cause of death (COVID-19 infection putting stress on an already failing heart) or incidental death (e.g., from trauma and they happen to have COVID-19).
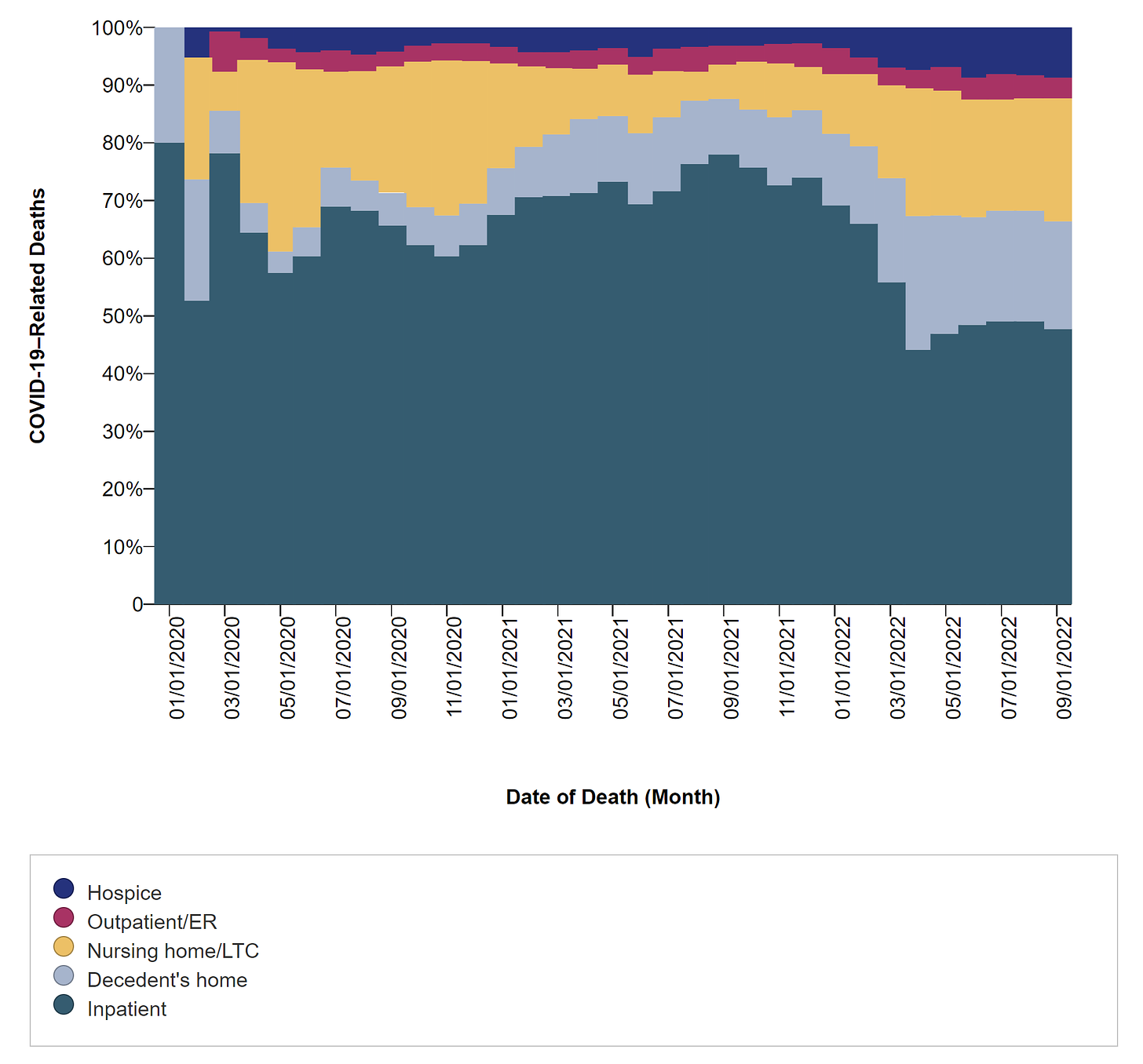
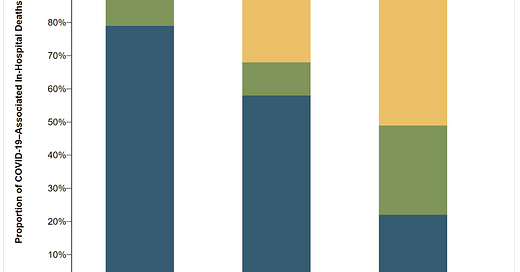
There has been a substantial shift in where people are dying. People are dying less in hospital settings, and more in hospice, at home, or in nursing homes. There are a lot of complicated reasons for this, including people who survived initial infection but continued to suffer COVID-19–related long-term health effects.
Treatment distribution is suboptimal
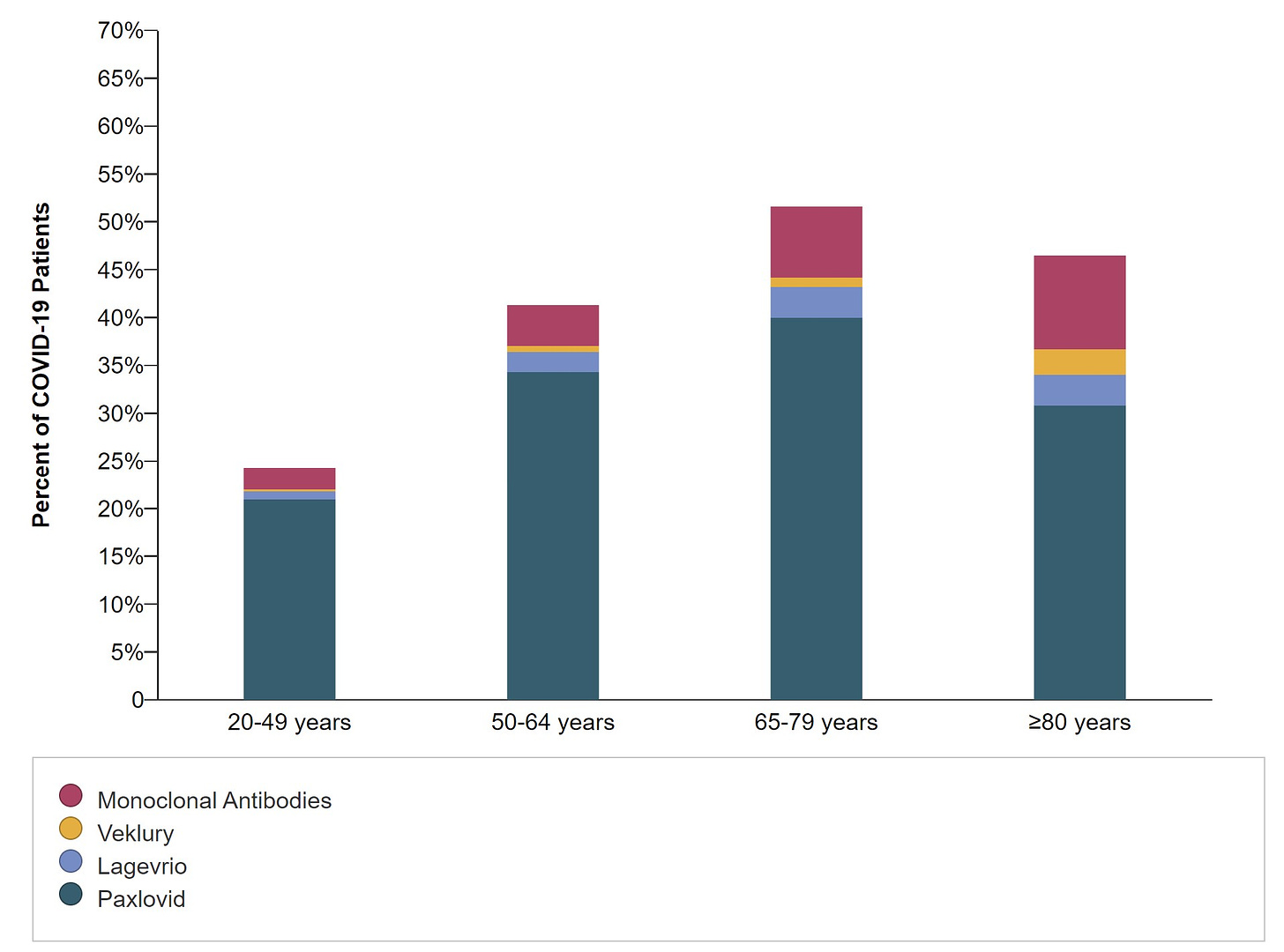
People over the age of 80 are less likely to receive Paxlovid than those under 65. This is a huge problem and may be for several reasons—medication contraindications (whether they are true contraindications or not), ageism, lack of clinician knowledge, and lack of access to treatment. We need to fix this and it should be a priority.
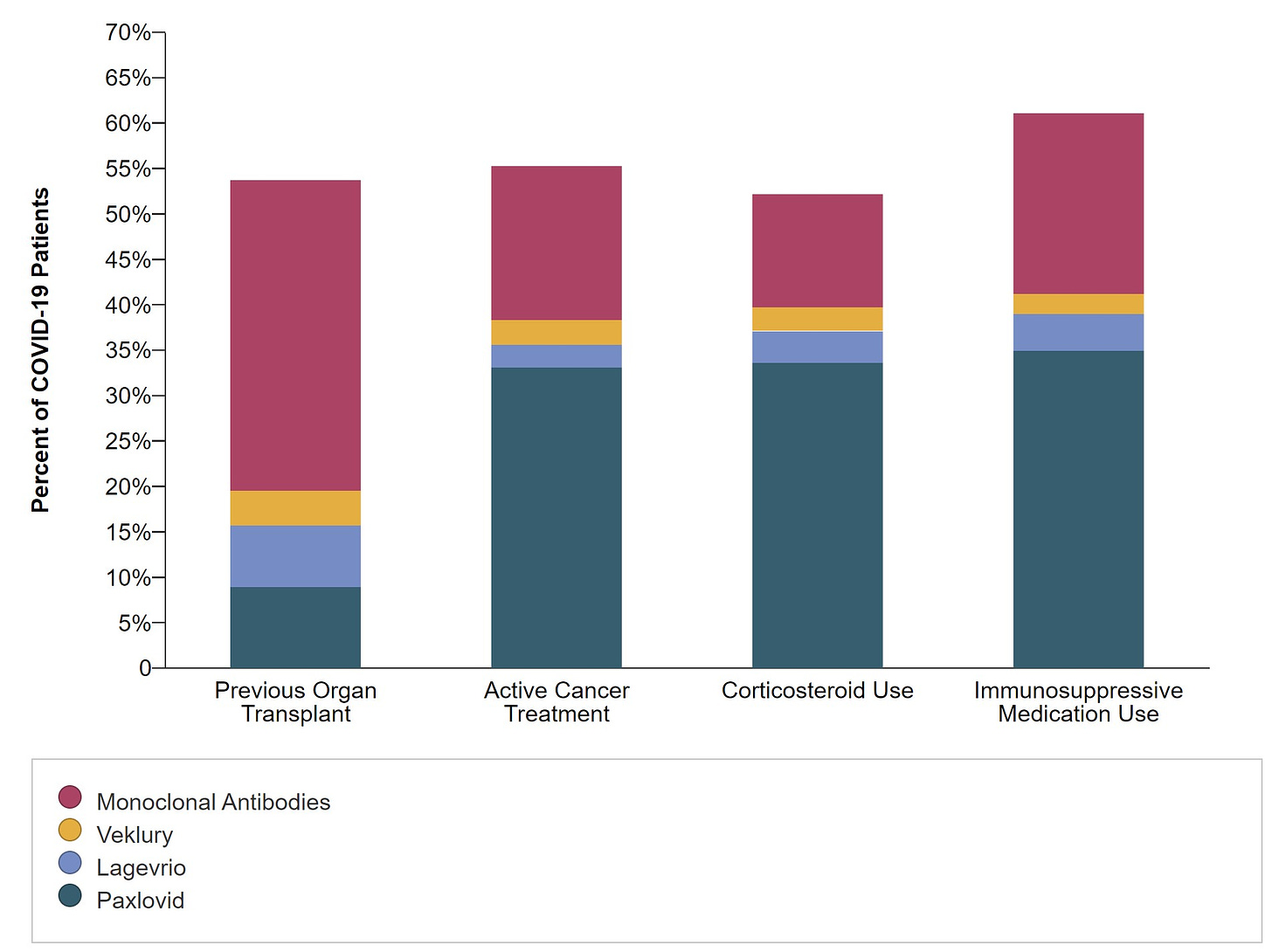
Among immunocompromised patients, 1 in 2 do not get medical treatment. This is even more concerning given that monoclonal antibodies are not effective against the newest of Omicron variants. In other words, that maroon color below will be removed for patients very soon.
Bottom line
To remove COVID-19 as a leading cause of death we need to focus on who is dying and why. To me, it’s clear that we need targeted communication, resources, and efforts to reach this goal, even given a landscape peppered (drowning?) with pandemic fatigue.
Love, YLE
“Your Local Epidemiologist (YLE)” is written by Dr. Katelyn Jetelina, MPH PhD—an epidemiologist, data scientist, wife, and mom of two little girls. During the day she works at a nonpartisan health policy think tank, and at night she writes this newsletter. Her main goal is to “translate” the ever-evolving public health science so that people will be well equipped to make evidence-based decisions. This newsletter is free thanks to the generous support of fellow YLE community members. To support this effort, subscribe below:




Congrats 👏 on the CDC appointment! Well deserved and definitely needed! Loved your appearance earlier in the year on WNYC with Brian Lehrer and I hope this new gig leads to more opportunities for you to do that kind of communication.
One suggestion for you - I spent close to 40 years in the biopharmaceutical industry. I had to prepare, present and interpret data for myself, my colleagues and management on a daily basis. I personally find many of the graphics used in the CDC summary you just reviewed baffling, especially the stacked line chart graphs. Please convince the powers that be that simpler, more straightforward presentations of critical data will go a long way to better communication and engagement by a wider public audience.
I can think of no one more qualified to share important information from the CDC.
You have been an invaluable resource for those of us who have been following you.