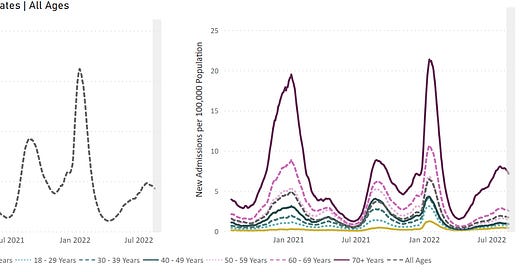
Age is the strongest predictor of COVID-19 severe disease and death. Even though those aged 65+ are the leaders in vaccination rates, they continue to lead hospitalizations in the U.S. and across the globe.
But… why?
An onslaught of scientific information can tell us why this may be the case. I worked with Edward Nirenberg to translate the science to show why boosters among this population, especially, should be of utmost priority.
First wall of defense: Degrading
We have a complex immune system, but for simplicity, we can reduce it to a few major walls of defense.
The first wall is neutralizing antibodies. These antibodies are powerful because they act fast—you inhale the virus and neutralizing antibodies stop the virus before there’s a chance for it to get into your cells (and start replicating). This prevents infection from happening in the first place. The issue is that it’s essentially impossible to retain a high level of neutralizing antibodies without regular, repeated exposures—and it gets even harder as you get older.
A recent preprint study found that the number of neutralizing antibodies you make in response to infection differs by age: the older you are, the fewer neutralizing antibodies you have (see figure below). In fact, when faced with Omicron, 43% of people had no detectable neutralizing activity and, among those, the mean age was 63.5 years.

Another important aspect of antibodies is not just the sheer number we have, but also the ability for the same antibody to recognize different variants of the same part of spike. Scientists found that antibodies among people 65+ years old were less likely to recognize multiple variants’ spikes compared to antibodies among those less than 65 years old.
Second wall of defense: Solid
Another line of defense are memory B cells. When we come in contact with a virus after having been vaccinated or previously infected, B cells remember what they need to create and start pumping out antibodies to help fight the virus. B cells can be quickly called in the event that more antibodies are needed.
An article published this week showed that B cell levels largely did not differ by age, which is great news. This wall of defense is solid. The challenge, however, is that for B cells to live up to their potential, they need the help of another wall: T cells.
Third wall of defense: Degraded
The third wall of defense is T cells. T cells are a key factor in determining the outcome of infections (severe or mild disease). There are two major groups of T cells.
Killer T cells recognize and kill infected cells
Helper T cells help B cells make antibodies and instruct B cells to make better antibodies
This means that while T cells can’t stop infections from happening altogether, they can rapidly control them once they start, potentially even to the point that people don’t have symptoms.
But there’s a challenge with T cells. Once we reach puberty, the thymus (the organ that gives rise to T cells) gradually degrades into a useless blob of fat and we stop making new T cells. There’s an especially big decline once we hit about age 40. This is usually okay because we typically accumulate all of the T cells we need throughout our lifespan. Unless a totally new microbe comes along that we have no exposure to (and fortunately, though SARS-CoV-2 is new, it’s still a coronavirus, so there is T cell memory from old coronavirus infections to work with). But as we get older, just like the rest of the body, our T cells age too.
Unfortunately, we see T cell dysfunction in COVID-19. An article published this week showed that the diversity of T cells for those aged 50+ years is much more limited than those under 50 at infection. Once symptoms resolved, there was restoration but people over 50 can’t really make full use of this unless they are infected again.
Implications
Two of the three defense walls among people over 50 years old have more holes than those of younger people. Comorbidities also increase with age, which means the immune response in general is a lot more taxed. This means the rate of breakthrough cases, and specifically severe breakthrough cases, is substantially higher for older people.
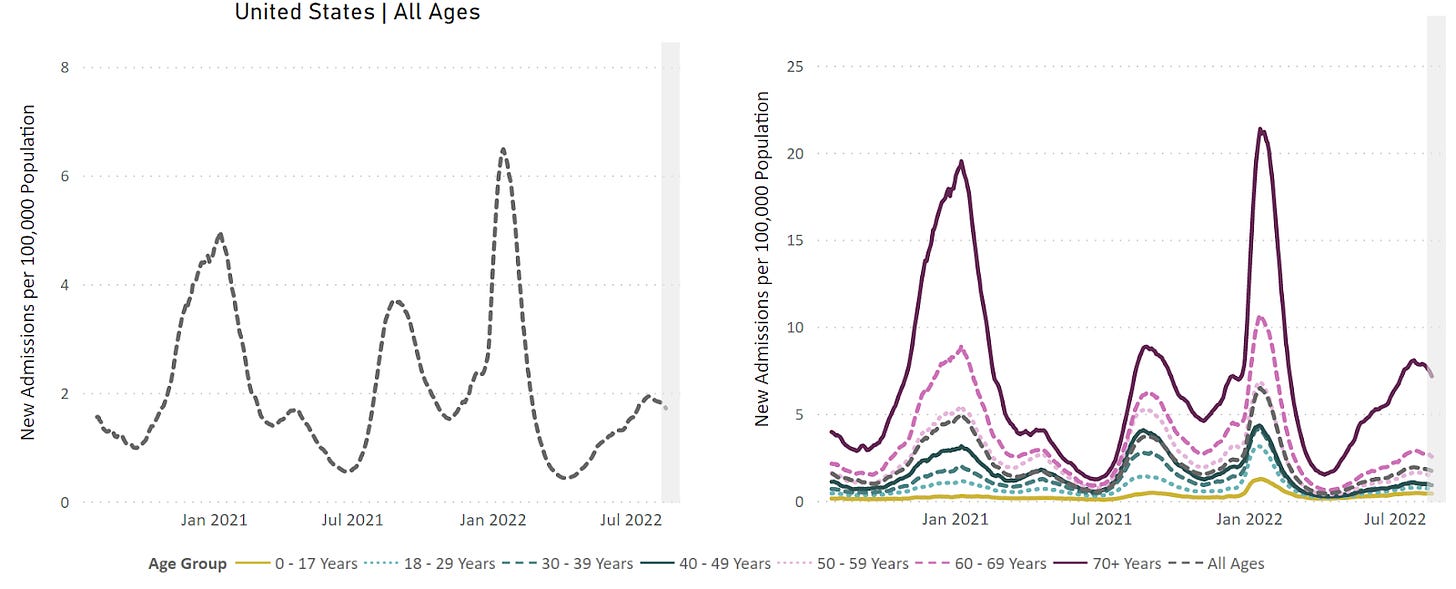
The good news is that the immune system is still working for a majority of people. We clearly see that the risk of severe disease even in the very elderly dramatically declines with even just the primary vaccine series.
However, it may take more doses to coax immune systems into doing the things we want. This may mean more frequent boosting in older age groups. We already see benefits with older people vaccinated with one booster dose having 4 times the risk of dying compared to people with two booster doses. (Unvaccinated people had 42 times the risk of dying from COVID-19 compared to those with 2 boosters.)
How much each incremental booster helps (or does not help) is something that we really don’t have a good grip on prospectively. For example, we didn’t really know a second booster was needed among 50+ year olds. We kind of guessed and relied on data from Israel (and the recent articles suggests why 50 might be a key age). Retrospectively, we can see that this was certainly the right policy call. But, the FDA needs to require pharmaceutical companies to test B cell and T cell functions—not just neutralizing antibodies—to assess the added benefit, instead of retrospectively determining good or bad policy.
Bottom line
Only 39.8% of 65+ year olds are up-to-date on COVID-19 vaccines. The best thing that this group can do is to fill the holes in their immunity walls by staying up-to-date. This also highlights that we cannot rely on immune systems alone, especially people aged 50+. Everyone else also needs to do their part (still) to keep the more vulnerable safe.
Love, YLE and Edward Nirenberg
“Your Local Epidemiologist (YLE)” is written by Dr. Katelyn Jetelina, MPH PhD—an epidemiologist, biostatistician, wife, and mom of two little girls. During the day she works at a nonpartisan health policy think tank, and at night she writes this newsletter. Her main goal is to “translate” the ever-evolving public health science so that people will be well equipped to make evidence-based decisions. This newsletter is free thanks to the generous support of fellow YLE community members.




Professor Jetelina — Thank you for this and for your other posts. You're a stellar, an absolutely stellar, public health communicator. This from a former senior consultant to CDC and national foundations and a former state senior public health official.
I have been looking for this well laid out data for a long time and a simple explanation of how the immunization system works and possibly why older people are so much at risk- including on the CDC website. I've found it so difficult to put together that I'd pretty much given up. Thank you very, very much, Katelynn.