We are losing ~400 Americans a day. In the last 7 days, we have lost 2,299 people. During August 2022 alone, we lost 15,284 Americans to COVID-19.
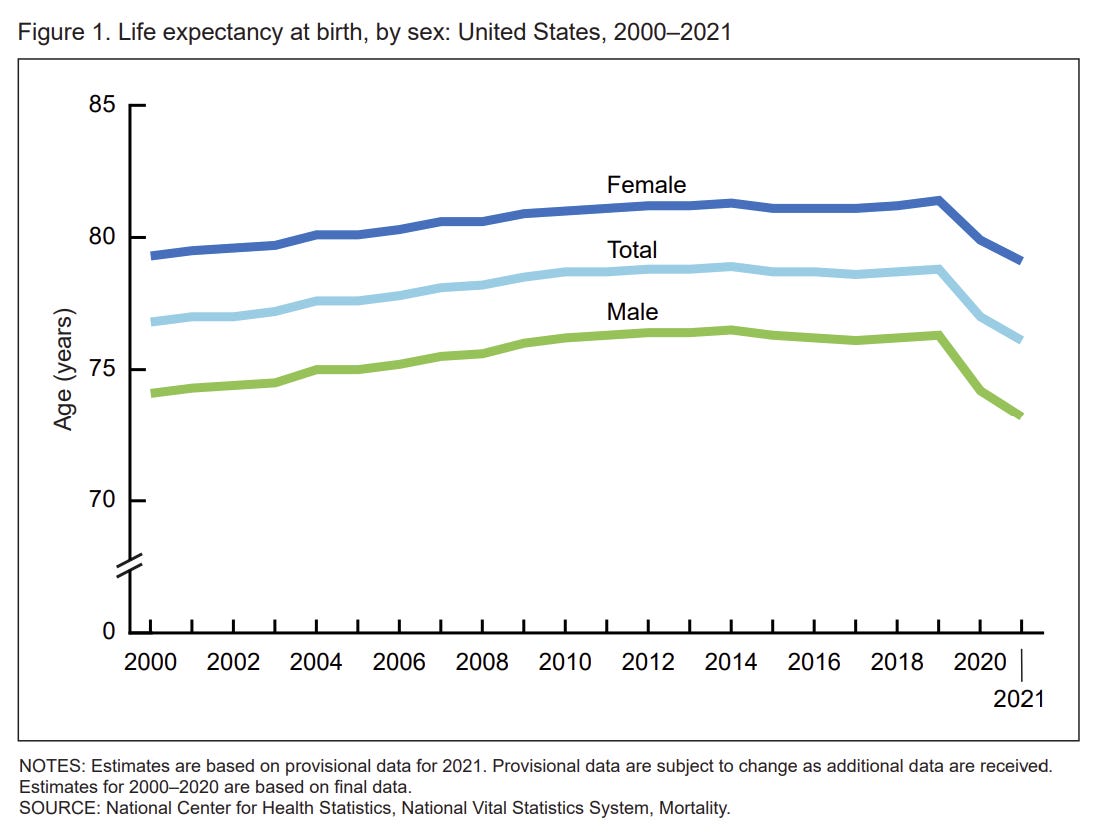
This means COVID-19 remains the third leading cause of death in our repertoire of threats. And it’s largely preventable. In the U.S., death rates are not back to pre-pandemic times; excess deaths are still 10% above “expected.” This is changing our average life expectancy. In fact, the U.S. experienced the sharpest two-year decline in life expectancy in nearly 100 years.
We cannot accept this reality. So it’s important to recognize who is dying so public health officials, families, and communities can work together to decrease this toll. This isn’t a reflection of blame, but rather a measure of where we can do better.
Who is dying from COVID-19 today?
An incredibly simple question that is challenging to answer. Death records are delayed, and we have a very fragmented data infrastructure in the U.S. making it almost impossible to capture a national picture. Regardless, I tried to scrape together what we have.
Vaccination
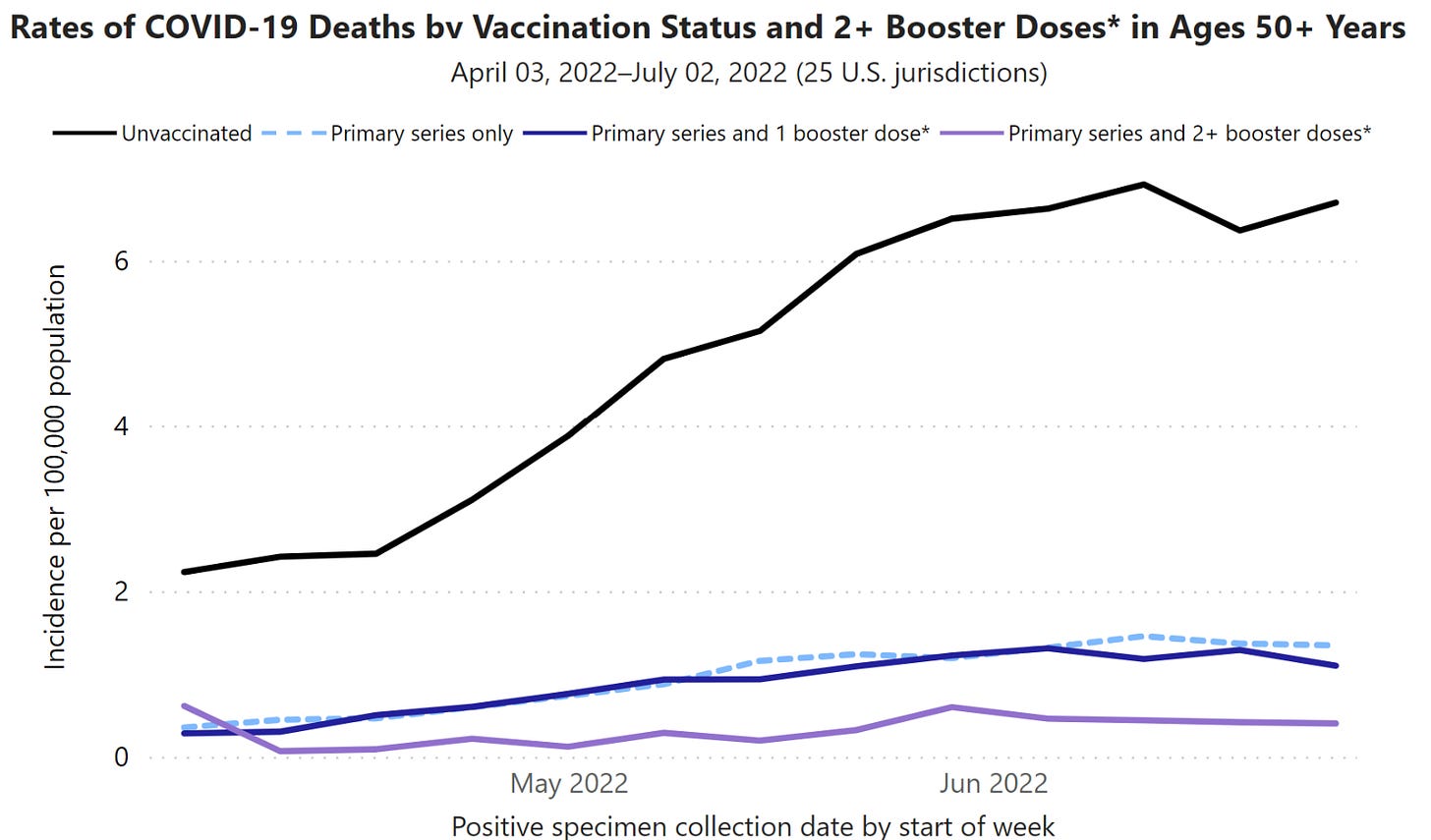
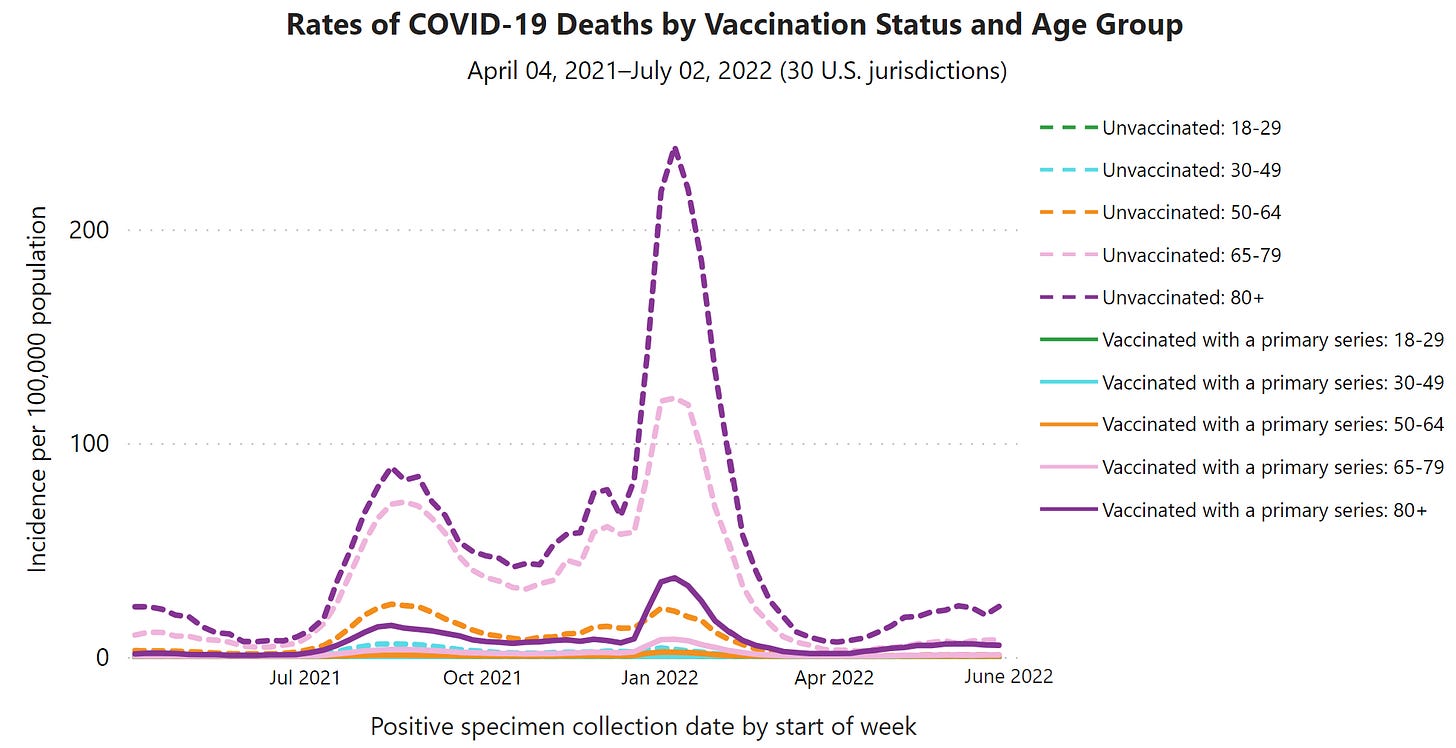
It’s abundantly clear the majority of deaths continue to be among the unvaccinated (20% of Americans are still without even one dose).
In addition, there is a clear dose response with vaccines: the more vaccine doses one has, the more that person is protected from death. According to the CDC, vaccinated people with one booster had 3 times the risk of dying compared to people vaccinated with two boosters. Unvaccinated people had 14 times the risk of dying compared to those with two boosters. Interestingly, the under- or un-vaccinated are more and more likely to have been infected. So, models are no longer comparing vaccinated people to immune naïve; rather, they are comparing vaccinated (or hybrid immunity) to those with more and more infection-induced immunity. This indirectly highlights a positive effect of vaccines against death compared to infection.
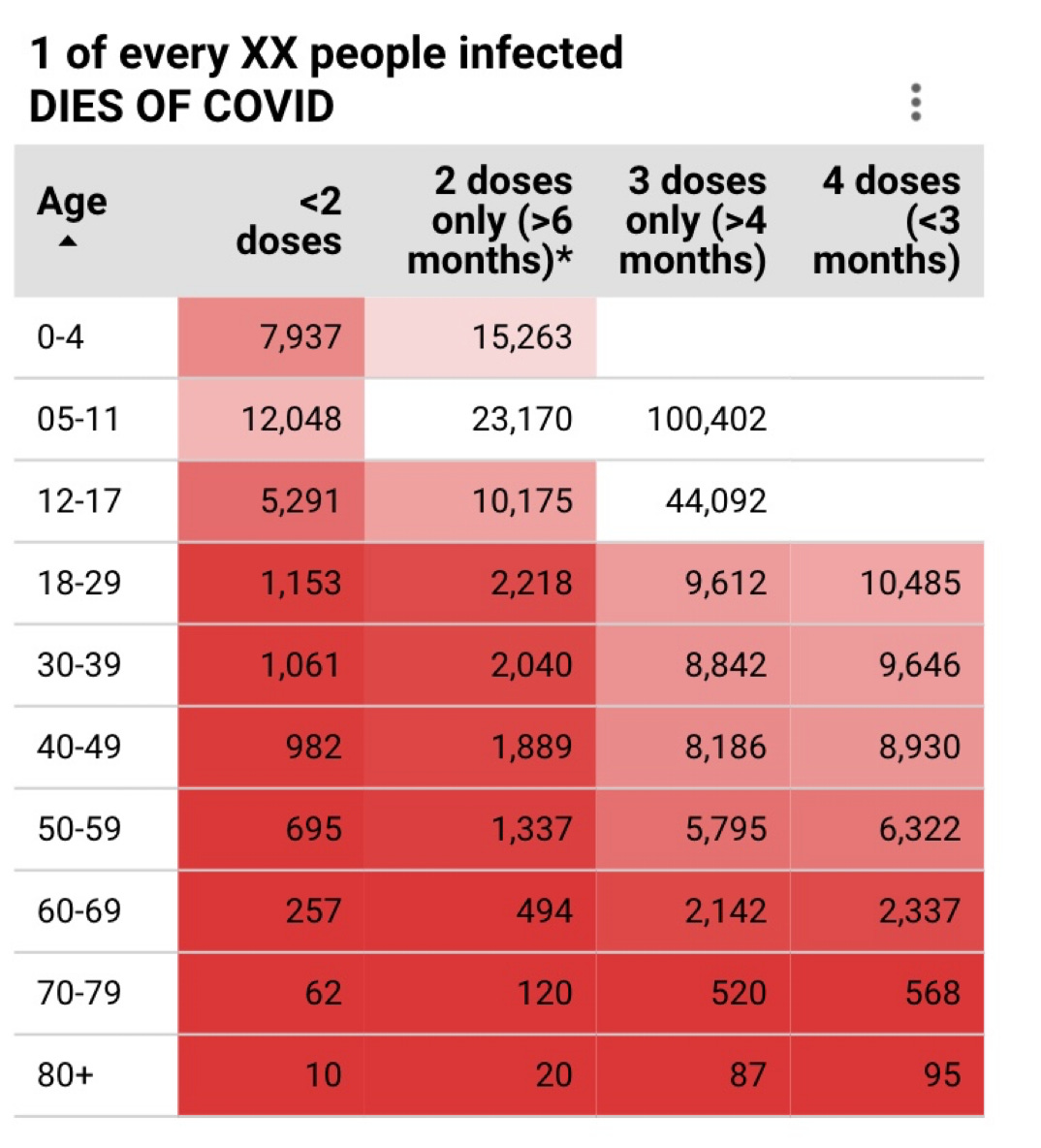
We also see this phenomenon from data in Canada from the COVID-19 Hazard Index. For every 10 people over the age of 80 who are infected, 1 dies. The odds decrease with more doses. The population-level benefit is true across every age group.
Age
Age continues to the be the strongest predictor of death. Specifically, unvaccinated 65+ year olds have, by far, the highest rates of death.
This also happens to be the most vaccinated sub-population in the U.S. (As I’ve written before, there are several physiological reasons for this phenomenon). But 5% still have not been vaccinated with the primary series. While 5% seems small, as we’ve seen throughout the pandemic, a small percentage of a lot of people (57 million) can be a lot of people. Even more concerning is that 60% of this population who have the primary series have not had a booster shot. This needs to change.
Beyond vaccination and age, we don’t have much information
Understanding the health status of those who die from COVID-19 is incredibly difficult without health records. In fact, this is impossible on the national level. The University of Michigan shared fantastic data on local hospitalizations (which we could roughly attribute to deaths). Among patients in the ICU and/or ventilators for COVID-19, about half are immunocompromised, have a significant underlying lung disease, or are over the age of 65 years. Also, 5 out of 6 people in the ICU are under- or un-vaccinated. This highlights that it’s essential to stay up to date on vaccines. One of six patients in the ICU is up-to-date on vaccines. This highlights that vaccines are not perfect; therefore, it is still important to try and reduce community transmission so vulnerable populations don’t get swept up in waves.
Other patterns
Because of death’s strong relationship with vaccination rates (and age and comorbidities), we continue to see other interesting relationships emerge across the States.
Regional patterns continue to shift. For example, Florida just passed New York in cumulative deaths. This is a big milestone given NYC’s huge death toll in early 2020.
Racial disparities. Interestingly, age-adjusted racial disparities continue to attenuate. I would attribute this to two things: 1) massive community engagement on the ground to reduce disparities; and 2) Black and Hispanic adults were more likely to be in the “wait and see” category for vaccines compared to non-Hispanic Whites adults, who were more likely to be in the “never get vaccinated” group. The Kaiser Family Foundation continues to update their data on deaths over time, and this closing gap is apparent.
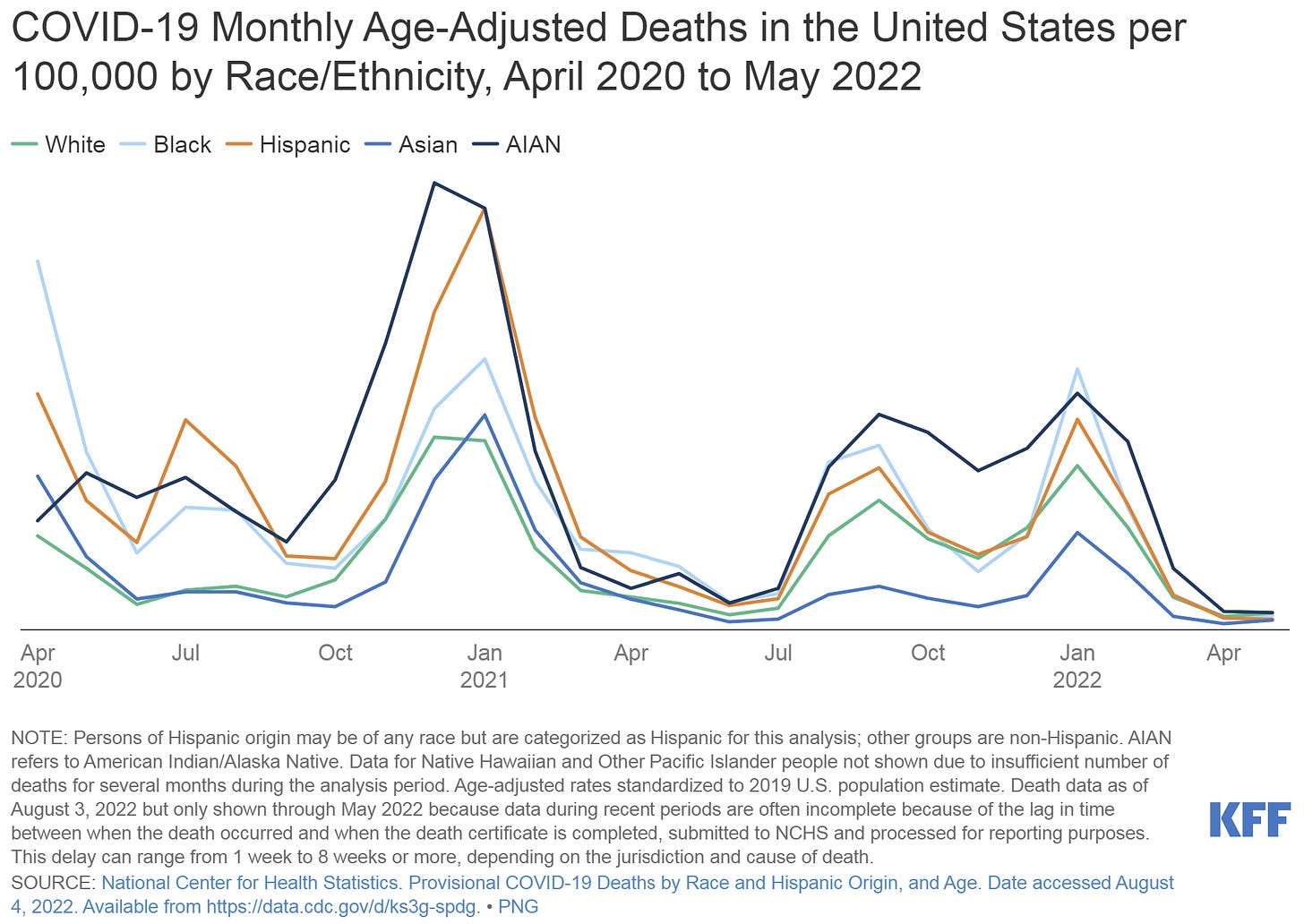
(Kaiser Family Foundation Source Here) Political patterns also continue to emerge. The Washington Post posted an article a few days ago highlighting this continued trend. While there is no difference with cases per capita, deaths per capita strikingly separate along partisan lines.
Bottom line
We are still losing an unacceptable number of Americans to SARS-CoV-2. I know it doesn’t feel like it in the news, or the grocery store, or even emergency departments, but it is happening. This is happening for myriad reasons, including misinformation, lack of trust, and lack of access to basic healthcare needs. Understanding who is dying and why is essential for public health outreach. We cannot accept this death toll in our society. We can do better.
Love, YLE
“Your Local Epidemiologist (YLE)” is written by Dr. Katelyn Jetelina, MPH PhD—an epidemiologist, biostatistician, wife, and mom of two little girls. During the day she works at a nonpartisan health policy think tank, and at night she writes this newsletter. Her main goal is to “translate” the ever-evolving public health science so that people will be well equipped to make evidence-based decisions. This newsletter is free thanks to the generous support of fellow YLE community members.








Now that we have experienced Covid in our home, it is even more apparent how insane the government's current response is. It basically begs us to get infected, and to spread the disease. And the thing is, prevention isn'y hard - masks work. I spent a week in a covid hospital room with my dad and did not get covid - i masked, i washed my hands, i was careful. We have had a covid positive person in our house and, so far and knocking on all the wood, it hasn't spread (although I am waiting for the shoe to drop) - but we masked, we isolated, we tested - and test everyday, we have been careful. It's not hard - it feels like common sense. I just don't understand the 'offiical' guidelines, which seem to be encouraging disease spread. Teachers don't get days off for quarantine but use their already not enough sick days, masks are not required and barely encouraged, testing after the initial test is not encouraged (because you may test positive again... and then you would know you are contagious and stop spreading??? it makes no sense)
And when you do follow common sense protocols - you almost feel crazy, like you're being extreme.
sigh.
As a person with Long Covid, I find this even more reprehensible. Even my closest friends who love and support me run about unmasked in crowded public stores and are adamant about their children having the 'freedom' to roam free of masking. Our world has grown increasingly smaller as we mitigate the very serious long term effects of this virus and the commitment to not becoming reinfected. I was vaxxed and boosted when I caught Omicron in June. Yes, vaccines and therapeutics must catch up but social distancing and masking are SO easy as a collective response to caring about our community. Befuddled.