In two short months, more than 18,000 cases of monkeypox (MPV) and five deaths have been reported across the globe. This is a rapidly evolving situation, but clearly a public health crisis.
While one takes hold (MPV) we concurrently fight another pandemic (COVID-19), so it’s tempting to compare the diseases and our responses. There are certainly similarities, but there are key differences, too.
Differences
MPV can be contained, but the window is closing. SARS-CoV-2 was (almost) impossible to contain because it was novel, mainly spread through the air, was very contagious, and spread asymptomatically. MPV doesn’t have these features, which means it can be contained*. It’s not clear whether this window has already closed, though. We need to act fast.
Response efforts seem to be effective in some countries, like the U.K. and Germany, as acceleration of reported cases has slowed, as shown in the log graph below. Acceleration in the U.S. continues. It’s hard to know whether this is because of increased testing capacity (which would be good) or because this is getting out of hand. It’s likely a combination of both, but we desperately need real time test positivity rate numbers to know.
This is not a novel virus. SARS-CoV-2 popped up out of nowhere, so we had to build everything from scratch: our knowledge base, tests, vaccines, and treatments. MPV has been around since the 1970s, and we already have all these tools. The frustrating part is that we need access to them, and this is moving slowly.
Not everyone is at risk for infection. For now. A virus that primarily spreads through the air (COVID-19) means everyone is at risk for infection. A virus primarily spread through close contact (MPV) means there is a social network phenomenon; some people are at higher risk for infection than others.
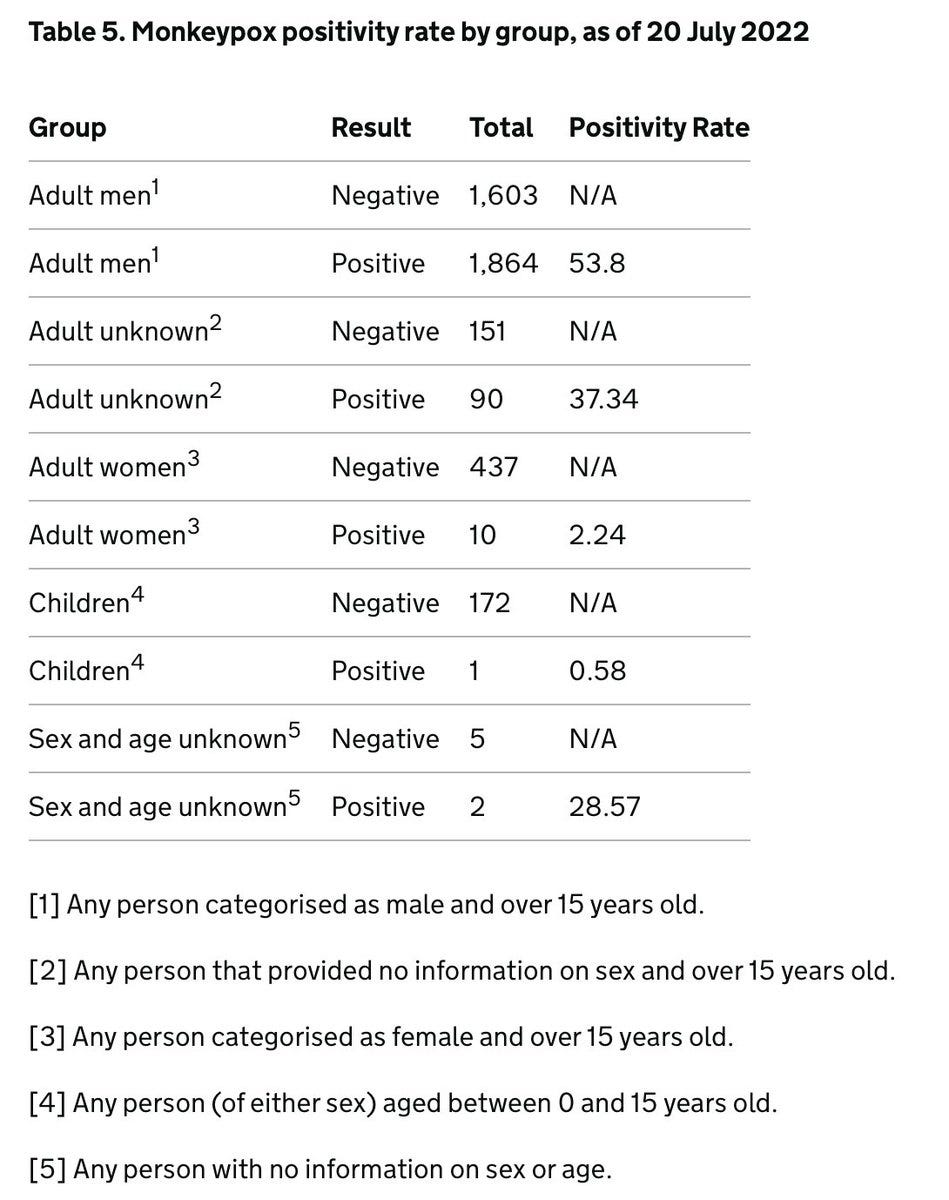
Using WHO demographic data, 98% of cases are men who have sex with men (MSM). Sexual contact is the main mode of transmission (91%). Weekly European reports continue to confirm this: Cases are almost exclusively male, aged 18-50 years old, and 43% MSM (56% of sexual orientation data is unknown or missing). U.K. data shows that this is not due to biased testing either—men have a high test positivity rate while women and children have a very low rate.
But this could change. There is already a clear (but rare) spillover into other populations. For example, two children in the U.S. got MPV. (Note both cases were from in-home transmission, so maybe contact with infected sheets or clothes but not door handles.) A pregnant woman and her baby were also just infected (the story of how she got it is not public yet). We need to stop MPV from taking hold in high-risk groups or new animal hosts.
Similarities
Public health infrastructure. The U.S. is somewhere in the middle between being prepared and unprepared. Just like with COVID-19, the MPV outbreak is highlighting our neglected, under-funded, fragmented public health system in the U.S. that desperately needs fixing:
Data infrastructure
Contact tracing capacity
Community engagement
Communication
Bureaucratic coordination
Trust
Fixing this is complicated, expensive, and takes time. It is certainly not fixed overnight, and it’s not fair to assume that we already had the time to fix it. Regardless, it’s hard to watch.
But it’s important to acknowledge that we are also not starting from scratch. We’ve spent the last 30 months creating systems, building capacity, activating leaders, building scientific and communication teams, engaging stakeholders, and understanding faulty data. Unfortunately, much of this work started to unravel because funding was chipped away. We need to reactivate and/or adapt these efforts. We need to allow for local cross-funding too—we can use COVID-19 dollars for MPV.
We also need a more aggressive, or at least faster, federal response: No more “wait and see”, declare an emergency (so we can get funding), and appoint a leader, a point person, someone to coordinate and communicate.
Communication. In the beginning of COVID-19, I would argue we had close to zero communication. It’s still not great. With MPV, we have another added layer of complexity. Different groups need different messages. Everyone should be aware of how it’s transmitted and what to do if there’s an unexplained rash. But resources, vaccine messaging, and education need to be laser focused on the MSM network. However, we cannot pigeonhole ourselves to this group, because we need to prevent stigma and because the situation may change. That’s challenging to communicate.
Misinformation gaining speed. Just as it did with COVID-19, MPV misinformation is starting to spread.
No, you cannot spread the virus with the new vaccine. (You could with the old vaccine, but that’s not being distributed right now.)
Yes, the vaccine is safe. No, we don’t have effectiveness data among humans for MPV. We have 22 clinical trials showing that it works great with smallpox and primate studies for MPV.
There’s a lot we don’t know. Despite their warnings about MPV, scientists were not heard and MPV remained a neglected tropical disease. Because of this, there are still a lot of things we don’t know:
What are the right doses and dosing intervals for vaccines?
How effective is smallpox vaccination from the 1970s?
What is the safety and effectiveness of the smallpox treatment TPOXX for MPV?
Is the virus viable in wastewater?
Is this a sexually transmitted infection? (We have preliminary evidence of live virus in semen, but need more data.)
The NIH is starting clinical trials to answer these questions. We also need to get data systems in place yesterday to track real-world data. (Are we using V-safe for MPV vaccines?) But, like with COVID-19, we have to make decisions now with limited information. For example, NY moved to delay second MPV doses to get more coverage while we wait for more vaccines (the right call). We are, once again, building the ship as we drive.
Bottom line
MPV is very different from COVID-19, but it certainly continues to highlight our vulnerabilities. We cannot give up; we have to do all we can to contain this before it establishes itself as another health risk in our repertoire.
Are we tired of this revolving door of panic and neglect yet?
Love, YLE
*A previous version of this said that MPV can be eradicated, which was removed. Given this is in multiple animal hosts, eradication is impossible.
In case you missed it:
“Your Local Epidemiologist (YLE)” is written by Dr. Katelyn Jetelina, MPH PhD—an epidemiologist, biostatistician, wife, and mom of two little girls. During the day she works at a nonpartisan health policy think tank, and at night she writes this newsletter. Her main goal is to “translate” the ever-evolving public health science so that people will be well equipped to make evidence-based decisions. This newsletter is free thanks to the generous support of fellow YLE community members. To support the effort, please subscribe here:





YLE - thanks for the update-
Monkeypox is another health concern that the health officials are destroying public trust in our institutions.
We have learned from Dr Brix that the CDC COVID response was politics over science. Data was manipulated.
Now public health officials are worried about stigmatizing a group over avoiding spreading a disease.
The real epidemic is how the Global Health and US Health officials are eroding all public trust.
Katelyn,
Thanks for the update. And, I look forward to your take on the vaccine round-table. But without funding, where does this go?
I'm concerned that we're looking at a longer-standing outbreak (recall this is a 2018-2019 trigger event) that went unnoticed in Europe and the US (or... worldwide). The latest manifestation is in the MSM population, but that could well be artifact. I had a discussion with our clinicians, most in primary care, and until the news started frequent discussions, they were unaware of the potential in the US and would not have had it on the differential diagnosis. When we add in the atypical presentation now being seen, that of a single lesion (often a genital lesion at this time), identifying it, and swabbing and sending the swab for viral culture would have been unlikely until the last 60 days or so in this country. Africa is different as it's endemic, highlighting the failure of the world to maintain adequate smallpox and monkeypox vaccinations.
There is ample evidence there is a respiratory component to transmission, during the prodromal phase when viral symptoms are the key feature, with a direct contact issue when lesions form.
This isn't as readily transmissible and the CFR is much lower than SARS-CoV-2, but identification of the problem has come very late and we're playing catch-up. I suspect we're 15x underreported, due to clinician unawareness and lack of test facilities.
While this has been seen and documented by CDC and WHO as a MSM issue, the potential for cross-over into the mainstream population remains present. I'm seeing the media hype, and for that matter CDC's focus on the MSM population as very similar to what I saw with AIDS decades ago.