We’re starting to see a drastic shift on the national level (and international level) for pandemic preparedness. In the United States, the White House released a new budget/plan for “Transforming our Capabilities”. Also, the Office of Science and Technology Policy was elevated to the Cabinet level for the first time ever last week— a big deal for science.
This is greatly needed. We have to get out of this reactive response mode and mount a proactive, coordinated, national strategy. This has been a difficult lesson for the United States to learn.
Some countries were forced to learn this lesson from previous epidemics, making their response to COVID19 tolerable. For example, South Korea’s COVID19 success is due to their flawed 2015 MERS response. After MERS, they made several changes to their health system, insurance system, and strengthened relationships between public and private agencies. This foundation allowed them to respond quickly to COVID19. We also saw success in Vietnam due to a heavy investment in public health years before the pandemic. New Zealand also had success focusing on four cores: "Rapid", "Science-based", "Empathetic leadership", and "Public confidence and adherence". This resulted in manageable country-level pandemics, even in the wake of Delta.
More diseases are coming
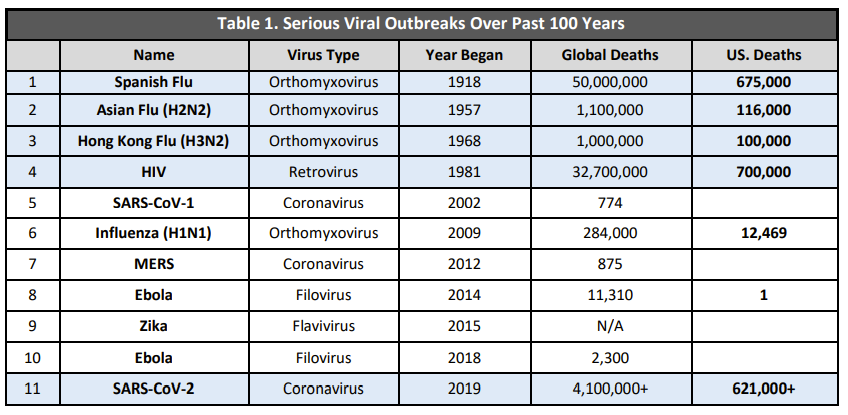
Since the Spanish Flu, we’ve seen the emergence of diseases come faster and faster. This is due to a myriad of things, but mainly because:
Diseases are jumping from animals-to-humans. With climate change, people are moving into areas that have never been inhabited before; animals, like mosquitos, are also shifting. An example is unfolding in real time. An outbreak of Nipah virus has caused hundreds to quarantine after a 12-year old died of the disease on Sept 5, 2021 in India. Nipah virus jumps from animals-to-humans, such as bats or pigs, and then is easily transmitted human-to-human. Nipah virus has a 45-75% mortality rate.
Humans easily spread the virus. Due to globalization, humans are able to travel more than ever, so viruses will be introduced in places that they’ve never been. We just saw this on July 15, 2021 when a case of Monkeypox from Nigeria landed in Dallas. But thanks to mask mandates on the plane and airports, a potentially severe outbreak was 100% prevented.
There’s no question that we will have another pandemic in coming years.
A critique…
And while the national plans are a fantastic step in the right direction, there is a blaring issue: The need for accessible, timely scientific communication.
When the Office of Science and Technology Policy was elevated to the Cabinet level, a memo highlighted, repeatedly, the need for science to be available to every American:
“Science is a tool that should be available to every American. More inclusive engagement in science benefits the American people, the environment, and the economy. The American public must be both knowledgeable about and involved in science research and its products, thereby fostering trust.”
And while this is nice, this is very different than making science accessible. We can’t just make journals free and expand STEM and expect the public to all of a sudden understand, trust, and engage in science. The vast majority of the U.S. will never engage if they can access nothing other than big brains talking about methods sections.
You've got to meet people where they are. We have to communicate to the public— the stakeholders — in real time, in “English”, in an inclusive, nonpartisan manner. Building capacity for effective scientific communication needs to be a key part of our national strategy. We have to bring the community along for the ride. This can look like a few things:
Communicate the threat clearly, communicate how the science is unfolding in real time, communicate how our understanding is shifting. And communicate this where the conversations are happening. The majority of Americans get their news and health information from social media; not an ivory tower.
Address the circulating misinformation and explain why it’s incorrect. We can do this by developing real-time, misinformation surveillance system;
Engage with community stakeholders to amplify evidence-based information through grassroots networks;
Improve health communication by addressing social determinants of health and acknowledging health equity; and
Listen, which is different than hearing. We have to actively engage with the public; go where they are asking questions. In the comments section of news articles, on YouTube videos, in community FB pages. We can even set up a database, like I did for YLE, to field thousands of amazing questions and messages to help guide content.
If we can do this, then the public may trust the science and may start making evidence-based decisions rather than decisions based in fear or misinformation. If we don’t, much of this billion dollar pandemic preparedness budget won’t matter. So, if you’re at the White House, Office of Science and Technology, or World Health Organization, I have a few ideas. Let’s please consider this as a core component of pandemic preparedness.
Love, YLE



As a professional communicator, I completely agree with the need for accurate, understandable communication about science.
Two things:
1. Effective communication is a learned skillset that takes years to master. Communicators who can communicate effectively about science are particularly rare. Most good communicators gravitate toward mainstream journalism, public relations and politics, because that is where the money (at least in the last two) and the "juice" is. You have to build (and pay) a cadre of science communicators. Far too many people think that they can talk and write effectively because they can talk.
2. Countering misinformation and disinformation isn't just a matter of correcting misinformed commentators. There is a well-funded, well-organized disinformation machine out there, highly skilled in the use of social media as well as unscrupulous false news media outlets. Combatting this machine and its products requires constant aggressive, professional communication. I believe it also includes some sort of legal reform so people and organizations that propagate false information that causes harm or death are held civilly and criminally liable for their speech.
Fantastic post—thank you. As an opera performance major at Indiana University who switched to major in chemistry (after an accidental explosion in an entry chemistry-for-majors lecture) and then went on to get an MS in Biochemistry, I FEEL THIS.
It is not difficult to understand the overall *stories* told by scientific discovery when science is treated as a fun and normal part of our world. Science is not the study of inaccessible ideas—it is the study of everything we care about and rely upon and the excitement and discoveries of this process can be shared with literally everyone *if* the jargon and ego can be dropped.
I got terrible undergraduate chemistry grades because I had to teach myself how to study science and how to make the the material make sense to me. I had literally no context for the words or ideas being thrown at me and had to create a framework to help me hold it all together. My core GPA was, like, The Worst.
I was discouraged from applying to graduate school…until the woman I had gone to for guidance changed her mind and said I absolutely SHOULD apply because the outcome (rejection) was guaranteed so there would neither be disappointment in the outcome nor regret for failing to try.
I got in to the program I applied to and ended up being an award-winning, independently funded graduate student who passed prelims while planning a wedding (and writing the real grant for real funding *and* teaching as an adjunct at the local community college). I ended up with an MS only because my advisor fired me following my request for medical leave and a reduction in training responsibilities so I could do my degree-earning research—he asserted someone interested in science education, as I was, had no need for a PhD.
I disagree.
And I disagree *vehemently* that there should be any allowance for any person with a PhD to be indifferent toward—let alone disdainful of—the importance of science communication and education. On one hand, my ability to communicate about science in such a way with new lab employees and graduate students was extremely useful to my advisor; on the other, that ability disqualified me from my position. That contradiction in attitude made my life very hard then and changed the entire trajectory of my life, but the pain I felt then is inconsequential to the pain being felt by all of us *right now* as we experience the real-world consequence of the failure of science to appreciate and *honor* the value of effective scientific communication and engagement with the public.