Happy March! Public health news isn’t slowing down, so here’s what you need to know to start your week.
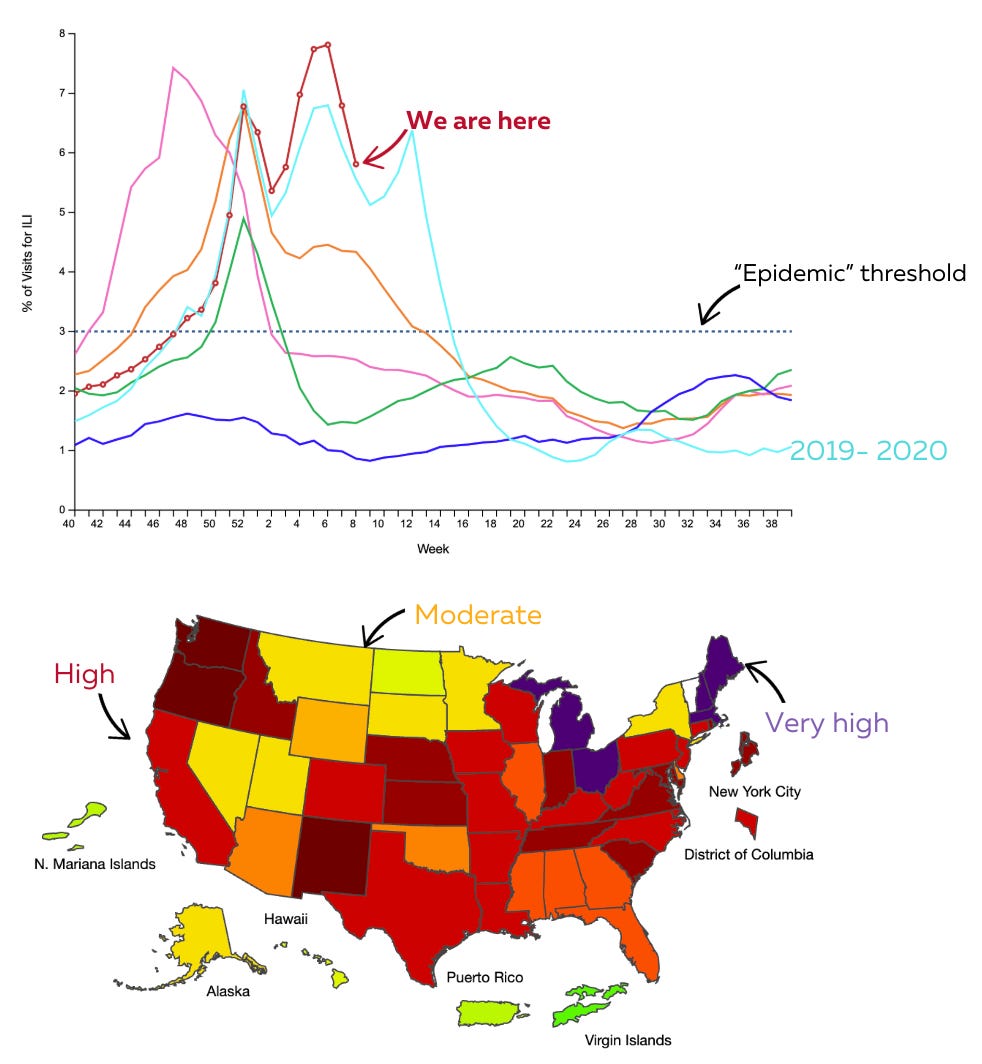
Your national disease report: Flu is decreasing
Good news: We’re getting a break from “influenza-like illnesses” (fever, cough, sore throat), which continue to decline—typical as the weather warms up. The Northeast still has very high levels.
A rare flu complication that impacts the brain—influenza-associated encephalopathy (IAE)—has increased this year, accounting for 13% of flu-related deaths (9 out of 68). We don’t yet know why it’s increasing, but it highlights the importance of flu vaccination in kids and the use of antivirals.
Meanwhile, Covid-19 metrics have been declining for a few weeks but are now stalling. With a mild winter and flu on the downturn, I’m watching closely to see if Covid-19 makes a spring comeback.
Last week, CDC published flu vaccine effectiveness data, and it’s looking good: 36-54%. The range is due to a combination of different data systems and one strain circulating that is notoriously hard to target with vaccines.
Other viral outbreaks in the past week
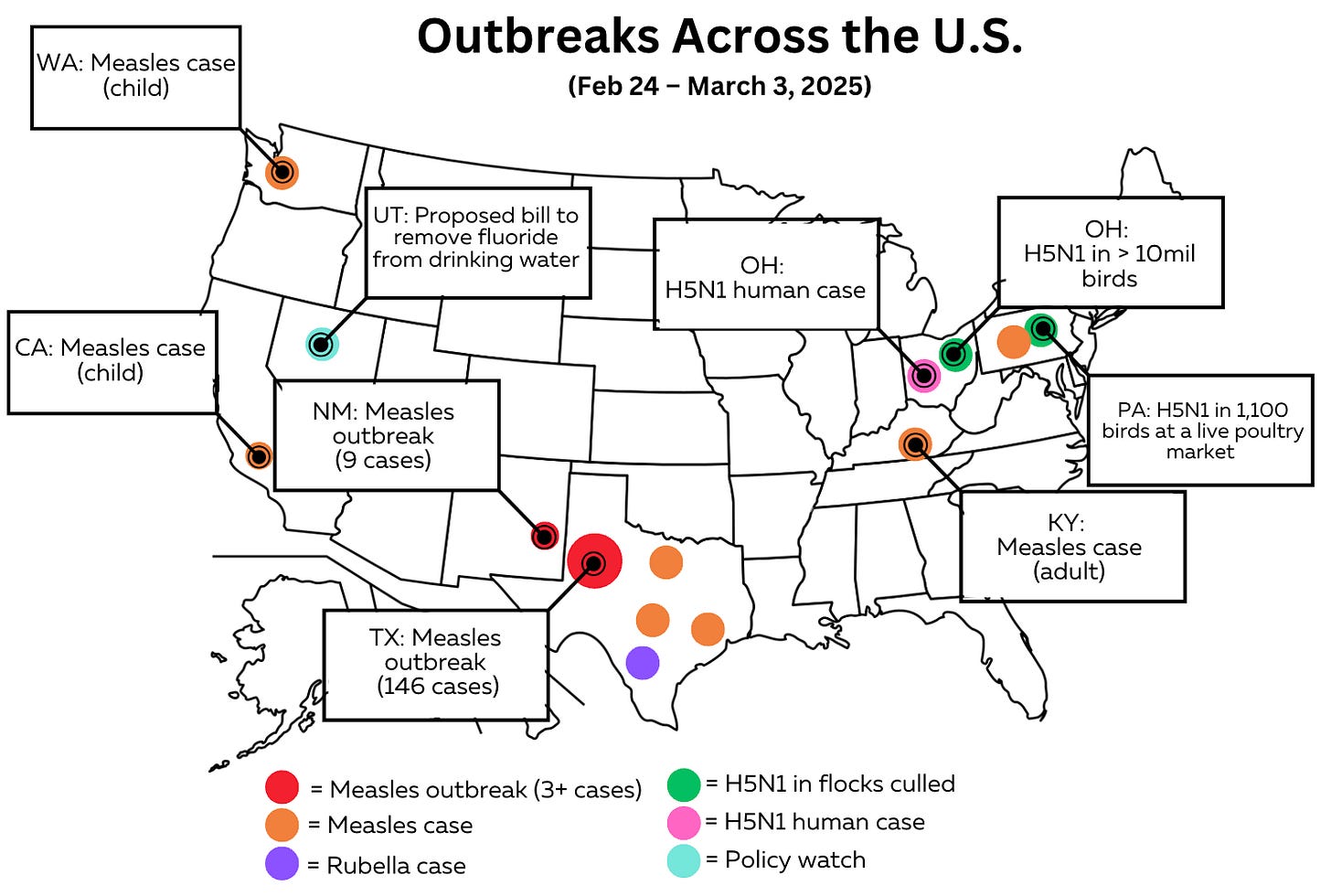
Other events, beyond flu, are popping up nationwide.
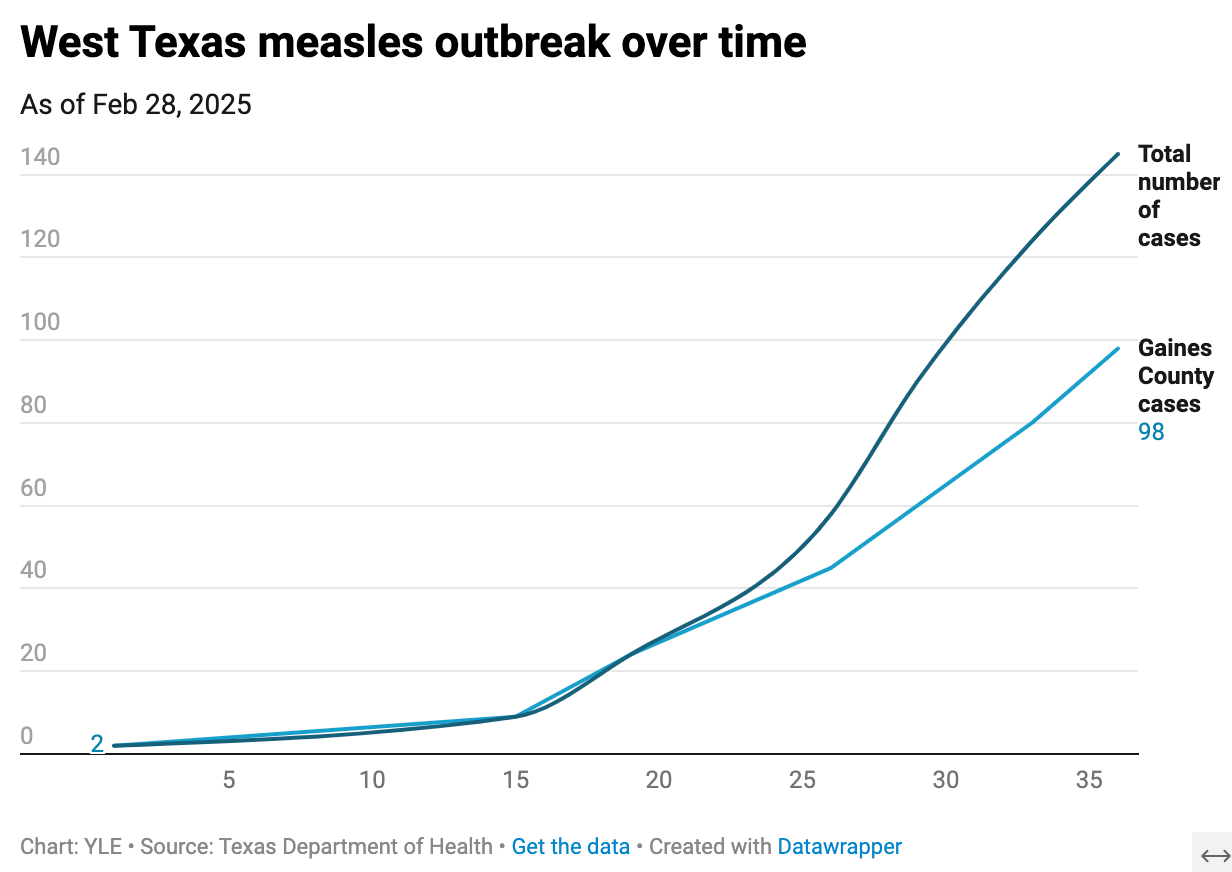
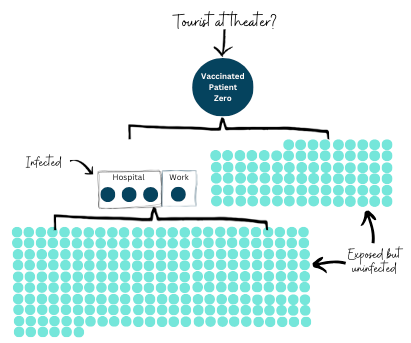
The latest count in West Texas measles outbreak is 146 cases. Twenty children have been hospitalized, some in intensive care. None were vaccinated. Texas’s case curve looks like it’s slowing, but it’s unclear if that’s due to control efforts or data/reporting challenges.
Other measles cases are popping up in Kentucky, Austin, Houston, Los Angeles, Seattle, and Pennsylvania. All are from international travel and have not resulted in outbreaks (3+ cases) yet.
A rubella case was reported in Texas (San Antonio). This vaccine-preventable disease can be devastating to pregnant women. Since we eliminated it in the U.S., it’s very rare—there were only 38 cases total from 2016 to 2022. Rubella, the “R” in the MMR vaccine, is caused by a virus that spreads from coughing or sneezing in airborne droplets.
In Ohio, a farm worker became infected with H5N1 after coming into contact with dead poultry. The virus jumping from a bird to a human shouldn’t be too surprising, given that Ohio had to cull 10 million birds due to mass infections. The risk to the general public is still low.
On our policy watch radar: Utah could soon ban fluoride in drinking water. The legislature is waiting on the governor’s signature. Fluoride in drinking water has beneficial effects, particularly in underserved areas. (Check out the YLE deep dive on this topic.) Utah would join Hawaii, which has already banned fluoride in drinking water.
Spring Covid-19 vaccine reminder
If you’re 65+ or moderately/severely immunocompromised, a spring Covid-19 vaccine is available. Last October, CDC recommended a second dose of the 2024-2025 Covid-19 vaccine for this spring. It’s a 6-month recommended interval, so the first people will be eligible this week.
Are they still working? Yes. Data published last week showed Covid-19 vaccines provided 45% additional protection against hospitalizations this winter.
Wait. Wasn’t the Advisory Committee on Immunization Practices (ACIP) stalled? It was. But this recommendation was approved in the fall, before Secretary Kennedy arrived.
Do you really need one? It’s hard to tell, given that the ACIP meeting was stalled, but I’ll tell my 93-year-old grandparents to get one based on last year’s data. They don’t need to run, but it’s worth the extra protection as we expect a summer wave.
VRBPAC meeting canceled—here’s why that matters
Speaking of vaccine policy, FDA’s VRBPAC meeting originally scheduled for March 13 has been canceled under the direction of HHS Secretary Kennedy.
While ACIP is CDC’s external vaccine advisory committee, VRBPAC is the FDA’s. This meeting is important because it would have determined the fall 2025 flu vaccine formula—a decision that must be made now since manufacturers require about 6 months to develop the vaccines.
What does this mean to you? Not much. This doesn’t mean there won’t be a flu vaccine this fall. The FDA and vaccine manufacturers will likely follow WHO’s formula recommendation (set last week). The U.S. rarely deviates from WHO.
That said, it’s ironic that the administration is pulling the U.S. out of WHO and has little communication with the agency, yet it is still deciding to depend on WHO’s guidance. Delaying VRBPAC’s meeting raises two other concerns:
Reduces transparency on options and decision points. These organizations have consistently been the voice of wisdom, providing clear, unbiased decision-making around vaccine policy.
Destabilizes insurance coverage. There is uncertainty about where to go next with vaccines, and without insurance coverage, there is less motivation to produce vaccines.
The strategy for flu vaccine development is now unclear. The ripple effects of these decisions could be significant in the long run.
Food safety alert: Listeria outbreak in nursing homes
A slow-burn Listeria outbreak (since 2018) was finally linked to frozen supplement shakes from Prairie Farms, which were distributed to long-term care (LTC) facilities.
The details:
38 people were infected across 21 states, resulting in 12 deaths
Cases were all in long-term care facilities. This is bad because older adults are at the highest risk of Listeria infections.
When CDC officials first investigated the outbreak in 2018, then in 2021 and 2023, they found that people were consistently sick only in LTC and nursing homes but couldn’t link the outbreak to its food source.
What does this mean to you? Spread the word to anyone in LTC facilities. Here is more info from FDA.
Science output is being slowed
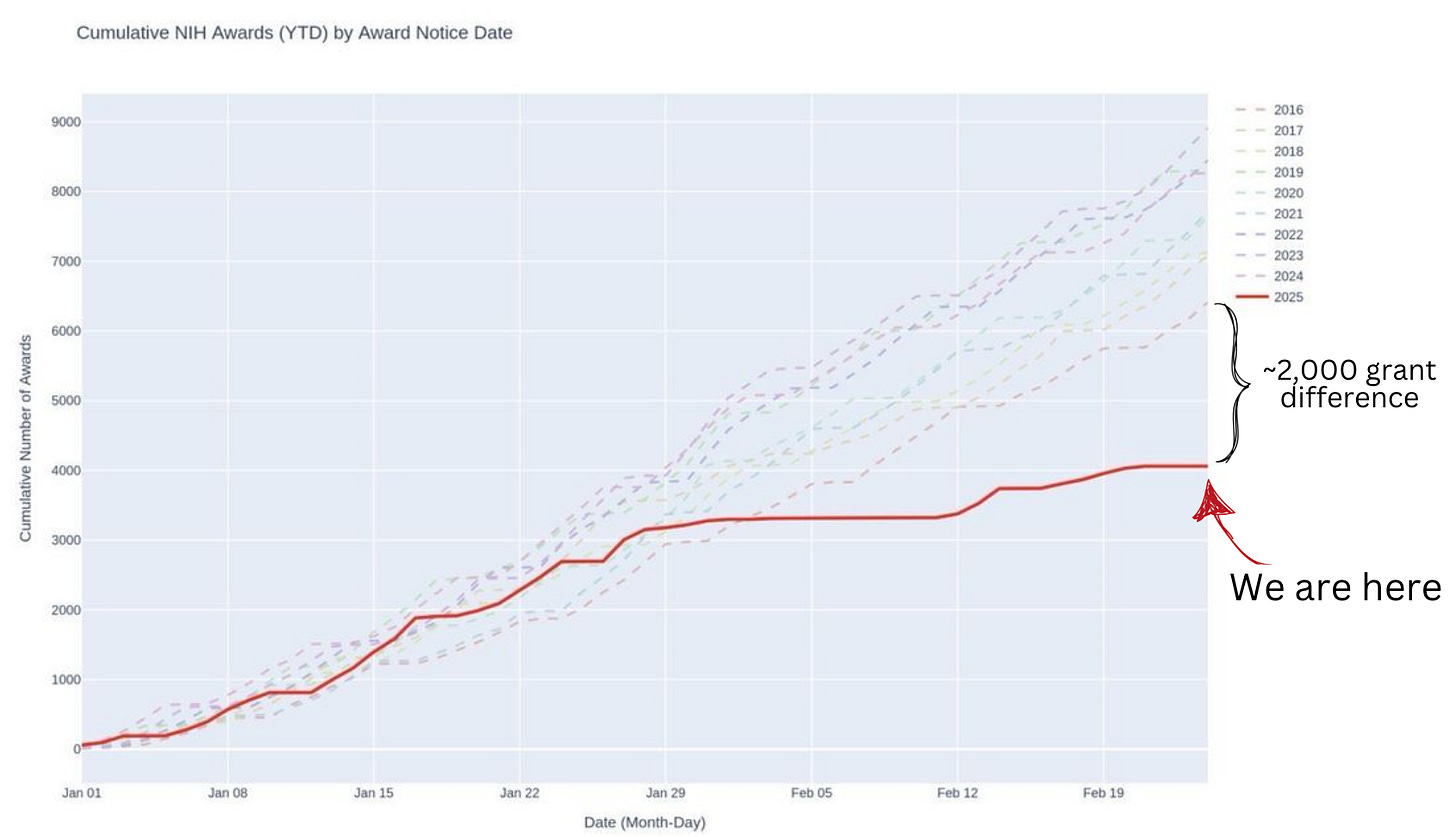
The National Institutes of Health awards grants annually, with funding distributed throughout the year. However, due to the funding freeze, stalled communication, and federal changes, significantly fewer scientific research grants are being awarded compared to previous years (as shown below).
As of February 18, this means the U.S. is answering approximately 2,000 fewer research questions—questions that could improve Americans’ health, quality of life, and longevity. While the immediate impact may not be obvious, a continued slowdown will create a ripple effect, jeopardizing future health outcomes and undermining the U.S.’s leadership in biomedical innovation and advancement.
Question grab bag
“Would H5N1 be transmissible through undercooked eggs? E.g., should people who prefer sunny-side-up or over easy eggs be advised to thoroughly cook eggs for the time being rather than having runny yolks?”
Technically, yes, but poultry don’t lay eggs if they are sick (or dead). So it’s not a big concern. The poultry industry has been dealing with H5N1 for a long time, so their biosecurity is top notch.
I’m also getting a lot of questions about measles boosters (very few people need one). Here is a post I put together last year that covers a lot of it:
Poll
There will be no poll for a deep dive on topics because… I’m off this week, stuffing my face with tapas and wine! That is, of course, unless something big happens; if so, I will jump back in.
Bottom line
You’re all caught up for the week! Stay healthy and sane out there.
Love, the YLE team
Your Local Epidemiologist (YLE) is a public health newsletter with one goal: to “translate” the ever-evolving public health science so that people feel well-equipped to make evidence-based decisions. This newsletter is free to everyone, thanks to the generous support of fellow YLE community members. To support the effort, subscribe or upgrade below:






Much appreciation for your work, always, but especially now. Thank you.
No one deserves a vacation more than you do, Dr. Jetelina!
Enjoy your time off. We'll all still be here when you're back. As always, your work is appreciated.