We are seeing an uptick in RSV and the flu in the Northern Hemisphere and particularly in the United States. Given an anticipated uptick in COVID-19, the media is coining this the “triple threat.” Here is the current state of affairs and what it means for you.
Respiratory Syncytial Virus (RSV)
RSV is a common virus that typically circulates during the fall, winter, and spring. Before the pandemic, everyone could count on being infected at least once before they reached the age of 2. Thereafter, people are typically infected multiple times throughout their lifetime.
Most people recover in a week or two, but it can be serious for two groups:
Young children. Before the pandemic, we saw ~2,300 per 100,000 children under the age of 1 hospitalized. (In comparison, the estimated hospitalizations rate is 30-40 per 100,000 children for flu and 48 per 100,000 children for COVID-19, pre-vaccine.) RSV is the most common cause of bronchiolitis (inflammation of the small airways in the lung) and pneumonia (infection of the lungs).
Older adults. Just like COVID-19, RSV is rough on older adults because their immune systems are weaker and they are more likely to have underlying health conditions, like heart or lung disease. In the U.S. an estimated 177,000 older adults are hospitalized for RSV each year and 14,000 of them die.
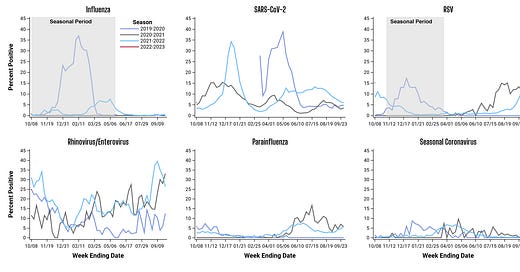
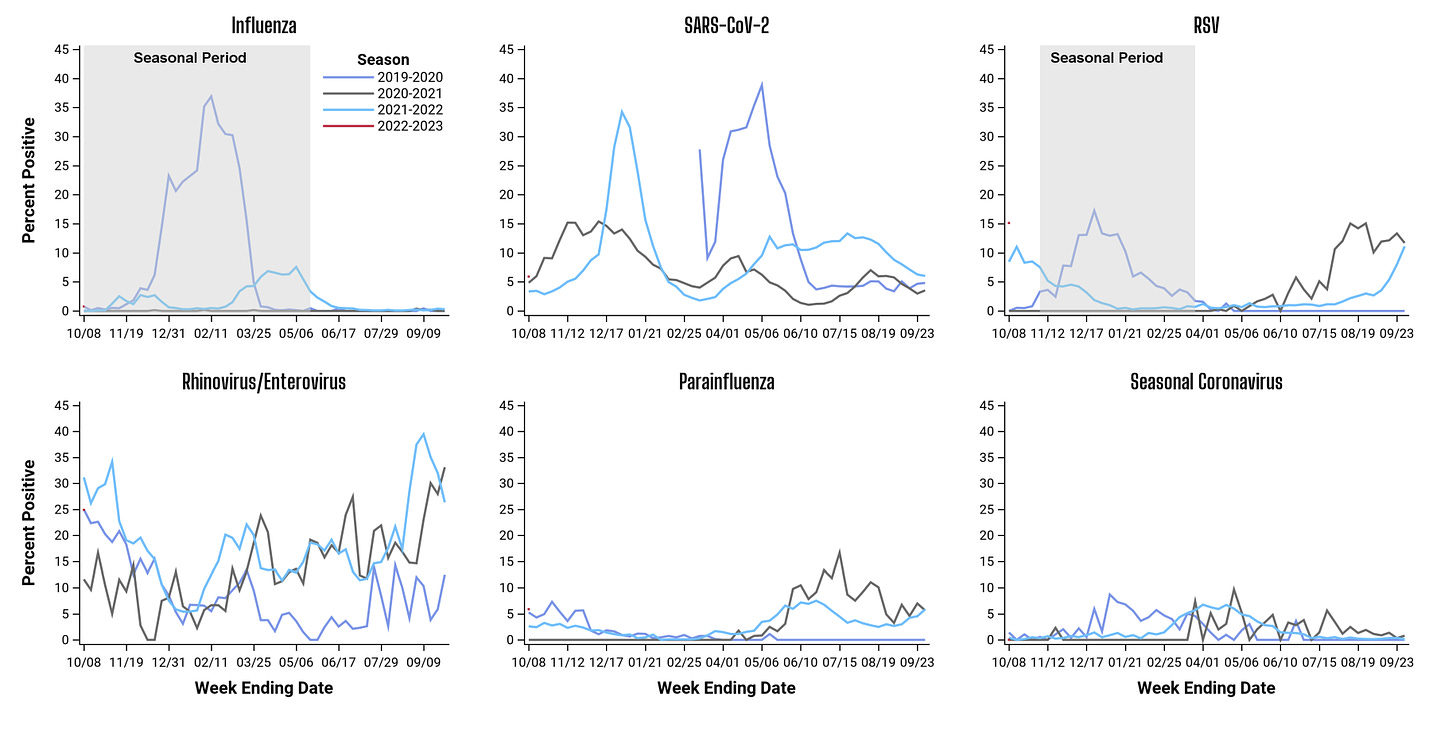
Overall, RSV is on the rise. As shown below, the percent positivity rate is above 10-15% in the U.S.—this means RSV is spreading faster than we can test for it and is causing an exponential growth in cases. However, we aren’t at record numbers yet. In fact, we are still below our very unusual 2021 summer surge. Almost all states are showing the same general trend.

There is quite a bit of discussion regarding how RSV is transmitted. The standard precaution for healthcare workers is hand washing, hospital gowns, and gloves. (Notice masks are not recommended.) These precautions stemmed from older studies showing the main mode of RSV transmission is primarily through large particles in the eye or nose or directly touching contaminated surfaces. RSV does have small particles that travel far, but this doesn’t seem to be a main mode given this older research.
There is currently no vaccine for RSV. However, last week we received very good news from two manufacturers (GSK and Pfizer) that vaccines in development for adults were highly effective: 82% efficacy rate for GSK and 86% for Pfizer. We can’t expect a vaccine for this season, but maybe next year.
Influenza (Flu)
The official “flu season” started two weeks ago and case numbers are higher and earlier compared to the past two pandemic years and compared to before the pandemic. (See red triangles in the graph below.)
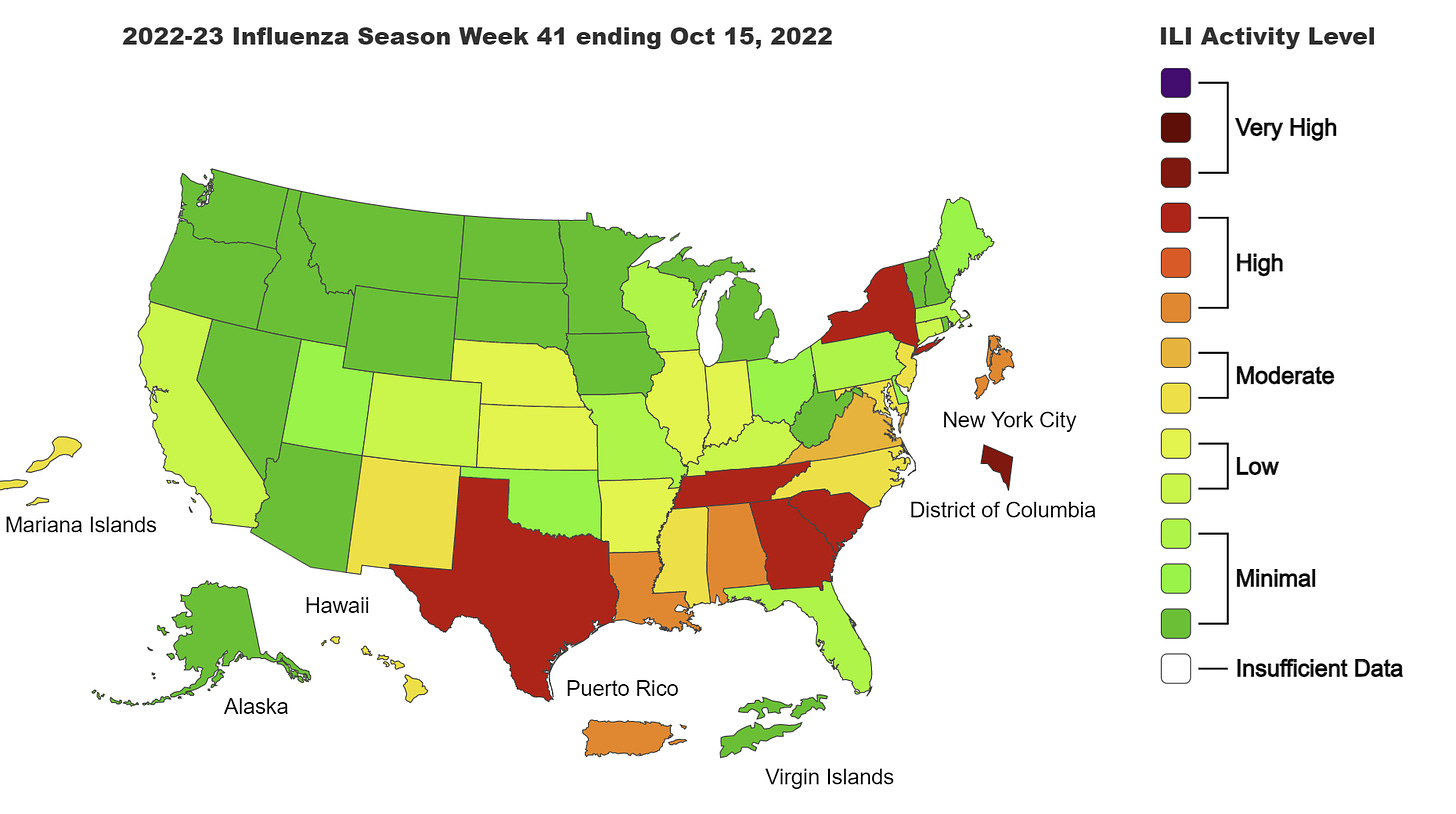
Flu rates are highest among 0-4 year olds, but cases in every age group are increasing. We are seeing regional trends with the flu, as the South has the most activity but East Coast states are starting to increase, too, particularly New York.
Flu viruses can be detected up to 5-7 days after becoming sick, but people are most contagious in the first 3-4 days after symptoms begin. Symptoms typically begin about 2 days (but can range from 1-4 days) after flu viruses infect a person’s respiratory tract. Some people can be infected with flu viruses and have no symptoms but still spread the virus.
There is a flu vaccine. We won’t know how well the flu vaccine works until next year (we collect real world data in real time), but lab data is indicating the vaccine is a good match this year. Unfortunately, flu vaccine uptake dropped during the pandemic.
COVID-19
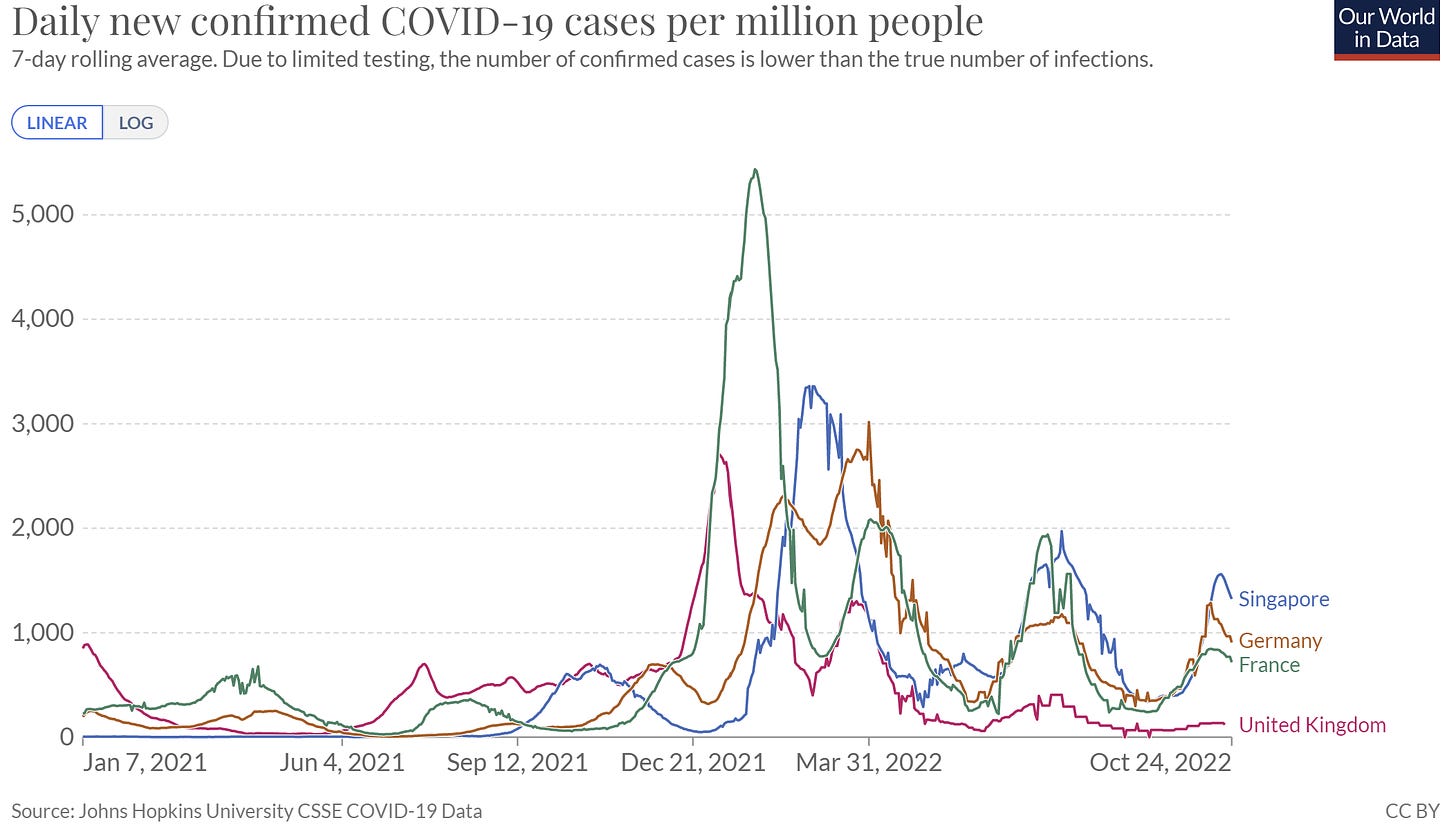
Then there is COVID-19, which is calming down in Europe, even in Germany. We are also getting good news from Singapore, where the Omicron subvariant XBB took hold and caused an infection wave. Thankfully their XBB infection wave was smaller than the BA.5 wave. (We expected the opposite.)
In the U.S., wastewater is stalling, while the Omicron subvariants, and particularly BQ.1.1, take hold. BQ.1.1 has now grown to 16% of reported cases. We typically see a variant’s impact at around 50%, so we still have some time.

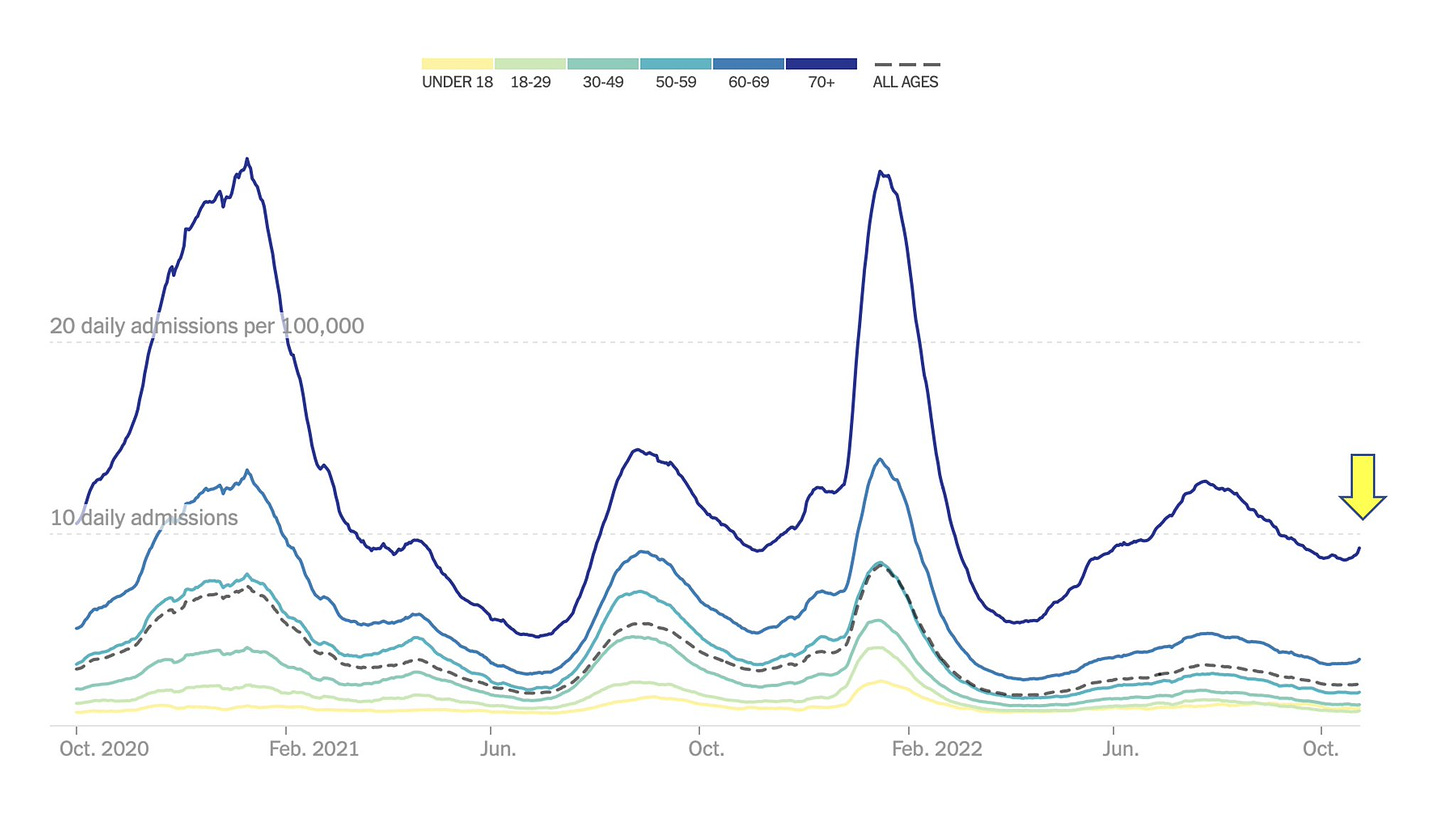
However, hospitalizations have started to rise for those over the age of 65, which is not a welcoming trend given that subvariants have yet to take over.
What does this all mean?
It’s becoming a petri dish out there. The triple threat specifically, though, isn’t in full throttle yet. This is clearly displayed in Chicago’s weekly surveillance report below where some viruses are rising but not all.
Will a triple threat come? This is one of the biggest debates among epidemiologists— the concept of whether we are witnessing virus-virus interaction. We know very little about how well viruses co-circulate with each other. For example, is flu spiking early because COVID-19 isn’t spiking yet? Maybe. Could RSV spike, then decline, then COVID-19 take over, then decline, then flu spike, and then decline? Maybe. Or, could they all spike at the same time? Maybe. We just don’t know what will happen, but a resurgence is expected.
This winter also depends on the strength of our healthcare system. The combination of our usual viruses co-circulating with COVID-19, burnt out healthcare workers, understaffed hospitals (in 2021, over 330,000 workers left healthcare), and staff being out for illnesses themselves, does not paint a pretty picture.
Bottom line
Lots of viruses are spreading right now and it’s a bit earlier than normal. We don’t have a triple threat yet, but I don’t think we want to see one, as I’m concerned for our healthcare systems. Do your part by getting vaccinated, staying at home while you’re sick, and other measures like washing hands, wearing a mask, and getting that airflow moving.
Love, YLE
“Your Local Epidemiologist (YLE)” is written by Dr. Katelyn Jetelina, MPH PhD—an epidemiologist, data scientist, wife, and mom of two little girls. During the day she works at a nonpartisan health policy think tank, and at night she writes this newsletter. Her main goal is to “translate” the ever-evolving public health science so that people will be well equipped to make evidence-based decisions. This newsletter is free thanks to the generous support of fellow YLE community members. To support this effort, subscribe below:





I'm curious to hear more about what you make of the COVID 'calming down' we're seeing in Europe and the unexpected smaller wave in Singapore. I know Germany had implemented some enhanced NPIs, but it seems those were too recent to have a material effect on the infection curve? What can we make of these seemingly better than expected trends and is it possible to extrapolate anything to what might happen in the US in the coming months?
Thanks so much Katelyn, I am a school district medical director and have shamelessly re-worded and quoted from your post for a school website announcement. I gave you the credit today and I give you SO much credit every day for the great work you are doing.
Ann Engelland, MD. aengelland@gmail.com