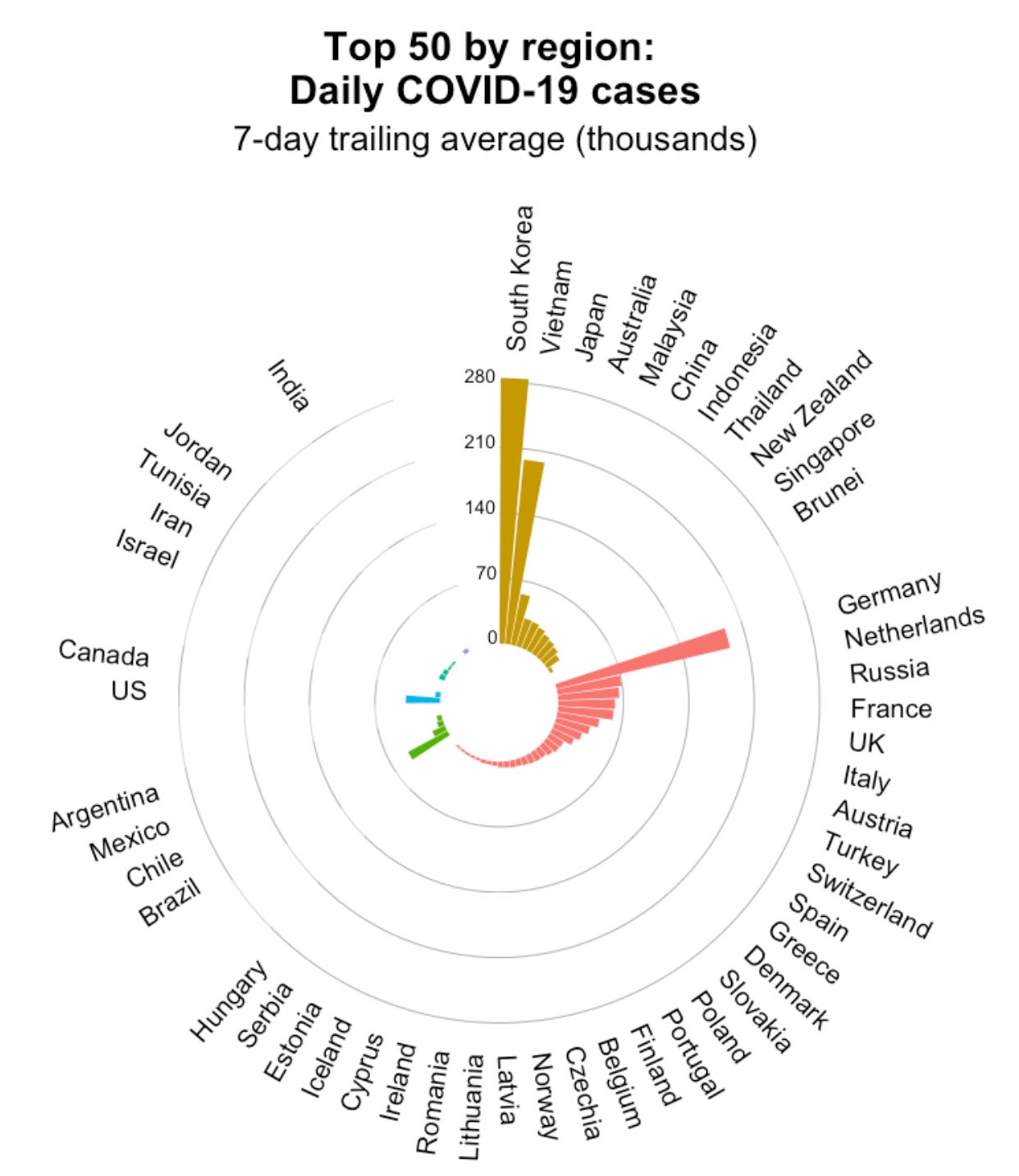
Case trends around the globe have made a u-turn and started increasing, specifically in Asian and European countries. The virus will continue to transmit and mutate, so a change in case trends shouldn’t be a surprise. We are also at a point in the pandemic where a rise in cases means something very different from country to country.
Asia
Asia is quickly catching up to the reality of Omicron. This combined with very low infection-induced immunity and the gradual move away from zero-covid approaches is proving to have some dire consequences for some countries.
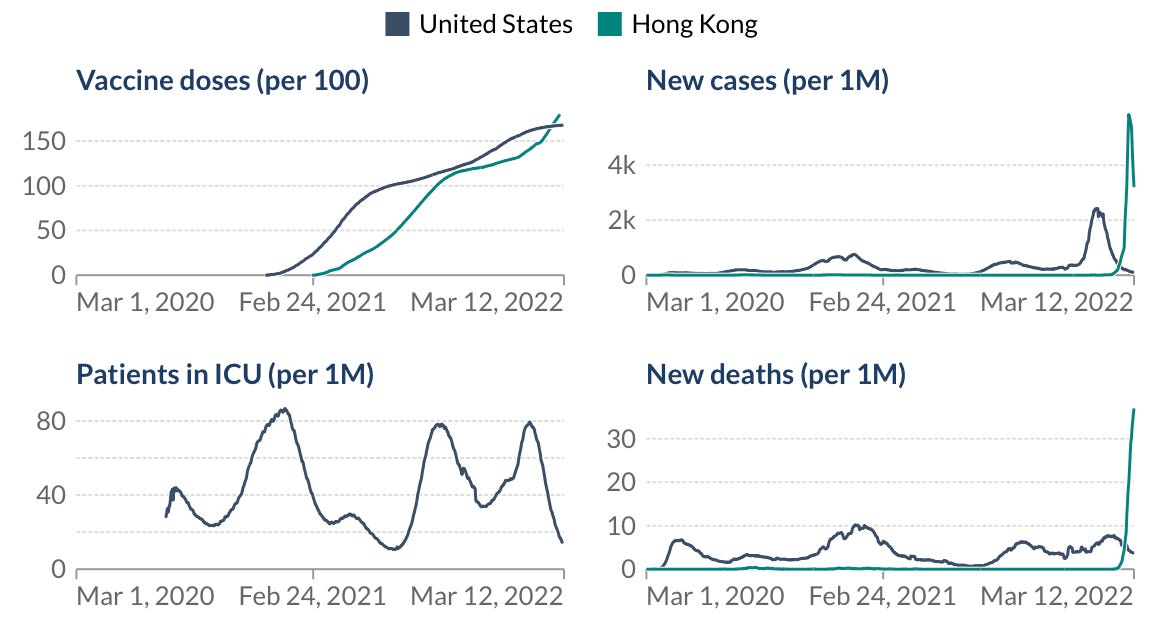
Hong Kong, for example, is an absolute tragedy right now with cases reaching heights that we’ve never seen before. They don’t just have a rise in cases, they also are breaking records for deaths, losing 35 per 1 million people to COVID19. As a comparison, the U.S. was losing 18 per 1 million people at the height of our COVID19 deaths. The amount of death Hong Kong is experiencing is unfathomable.
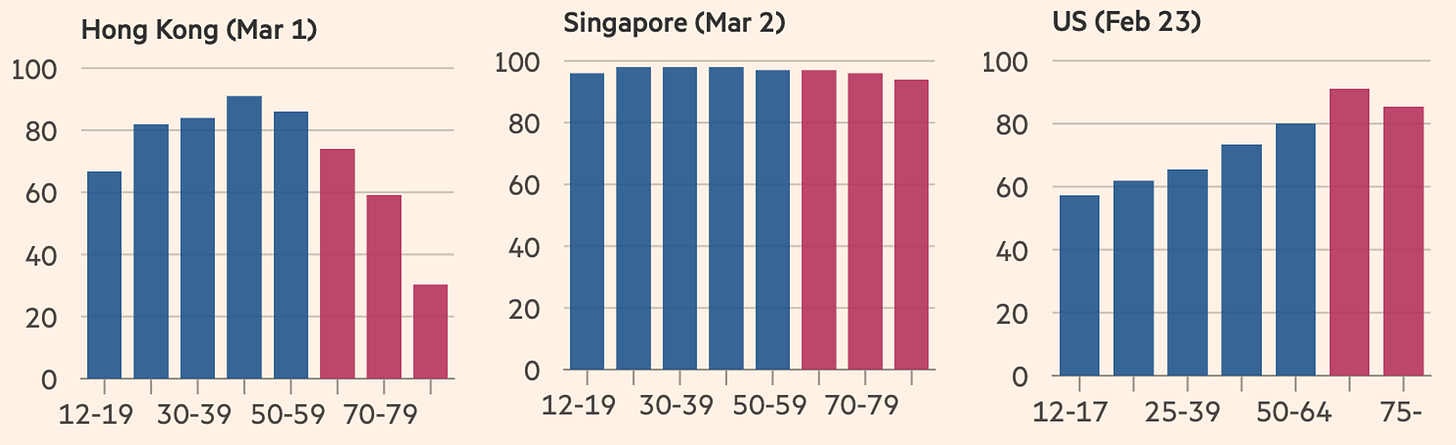
Hong Kong has roughly the same vaccine doses administered as the U.S., so what’s happening? Vaccine coverage among older adults. In Hong Kong, only 30% of 80+ year olds vaccinated with the primary series. This is compared to Singapore’s coverage of 95% and the U.S.’s coverage of >80%. Age is one of the strongest predictors of severe disease, so not protecting the older groups through vaccinations has dire effects. Also, this could be dependent on the type of vaccine. About half of people are vaccinated with CoronaVac, a vaccine produced by Beijing-based company Sinovac. Research has shown that among those over 80 years old, CoronaVac was only 45% effective against death.
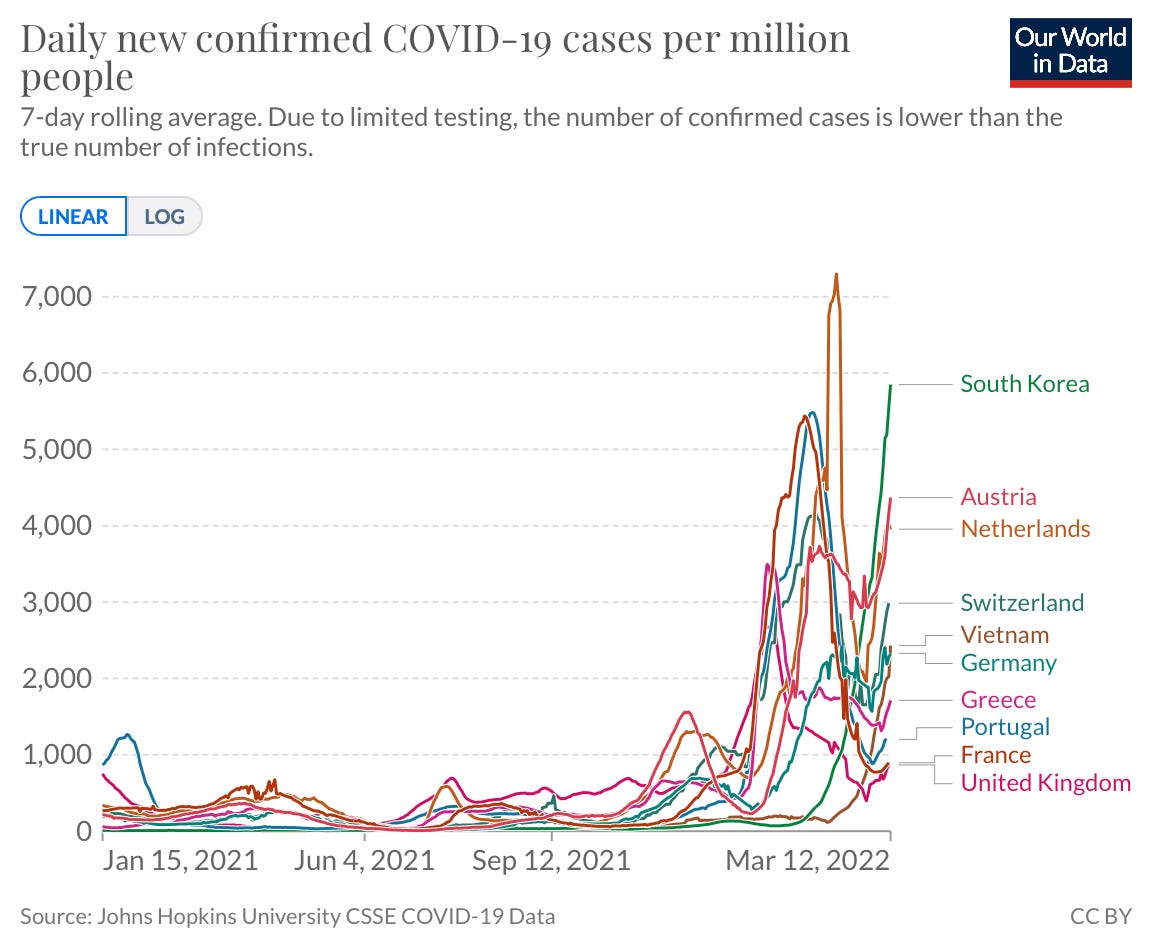
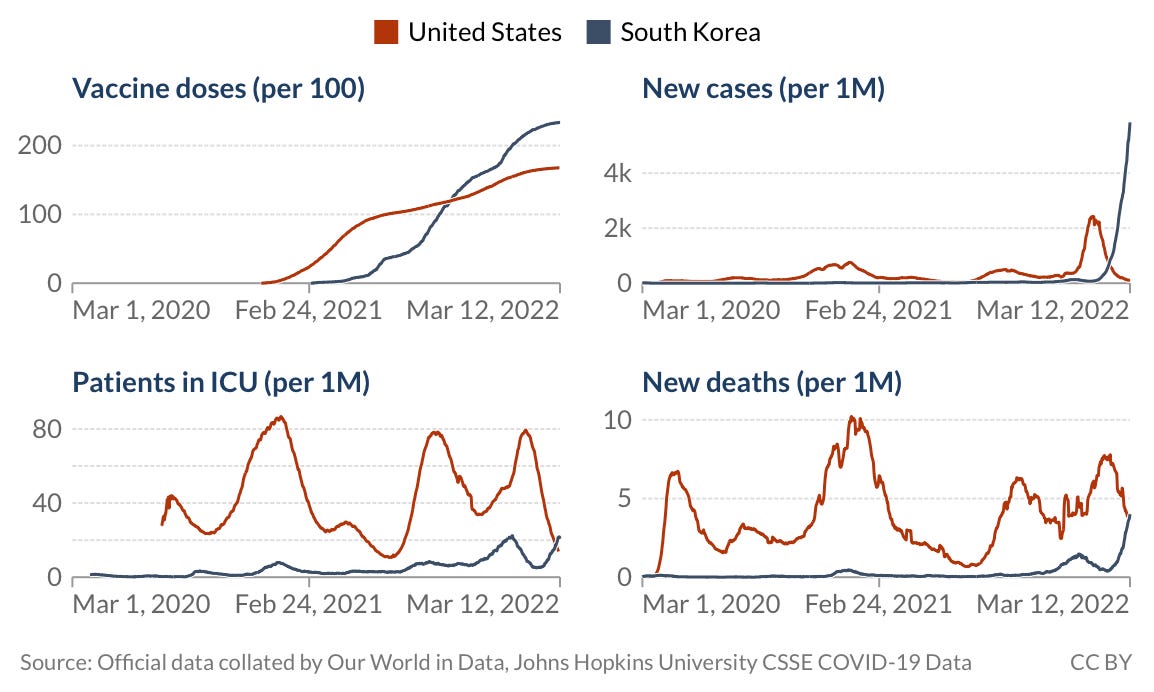
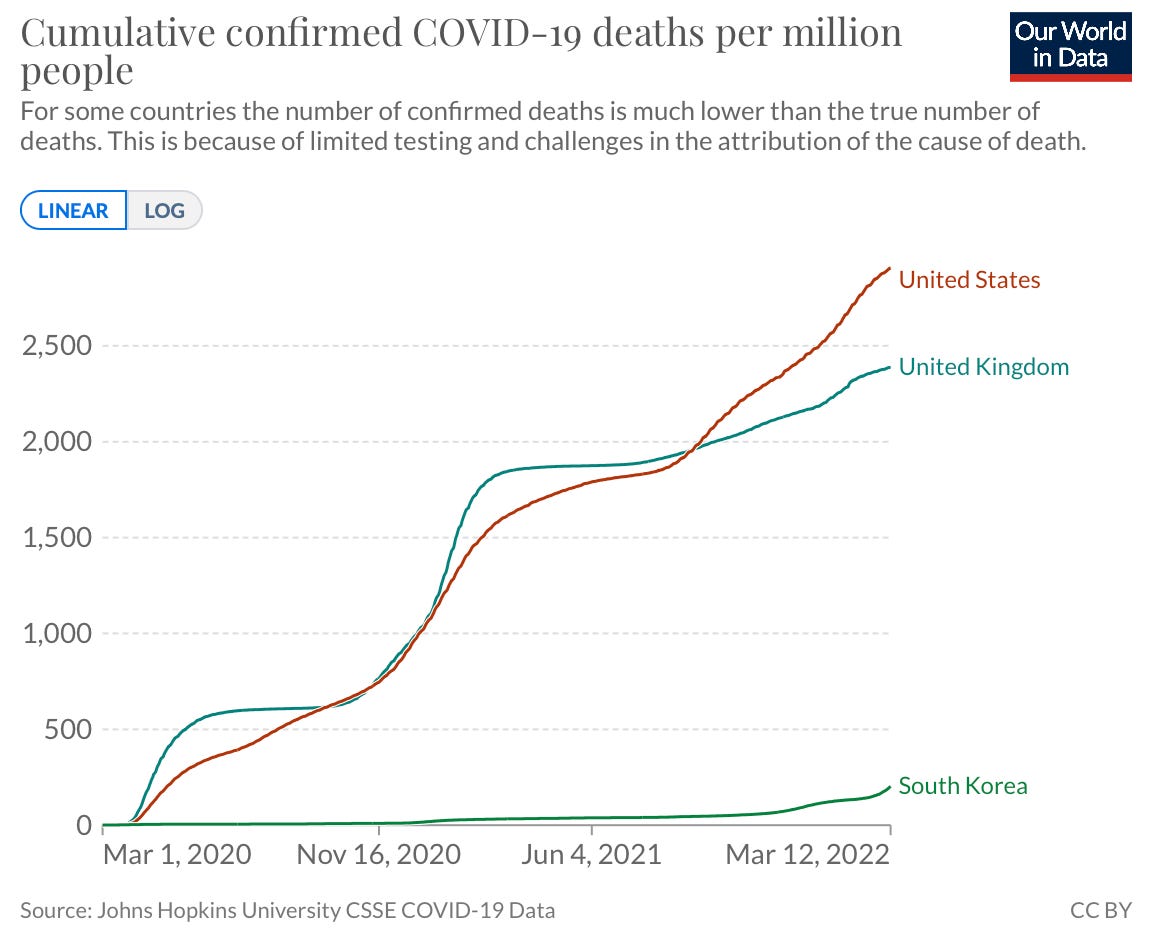
South Korea has been an exemplary model of COVID response throughout the pandemic, but even they are taking a big hit from Omicron. In one month, they’ve had a 450% increase in cases. Deaths are increasing too, but thanks to their fantastic vaccine coverage, deaths are not nearly as high. In fact, deaths in South Korea are still lower than deaths in the U.S. today.
It’s important to keep this in context. Cumulative deaths in South Korea are still merely a blip on the radar compared to the U.S. They’ve saved hundreds of thousands of lives because of their effective response throughout the pandemic and I’m confident they will continue to do so.
Europe
Cases in Europe are increasing, too. Germany is the case leader followed by the Netherlands, Russia, and France. In the U.K, cases have increased 30% in the past week. Austria, Portugal, Greece, and Switzerland are also seeing increasing trends.
There are many hypotheses for this uptick:
Collectively, the uptick could be driven by behavior. Countries are opening and people are really wanting to put COVID behind them (regardless of whether the virus is ready for that). For example, in the U.K., all mitigation measures have been removed, including self-isolation.
There has been chatter that the war in Ukraine may impact COVID transmission in Europe. In the past, war has increased the prevalence of infectious diseases, so this is possible. But I do not think mass displacement has directly caused an increase in European cases. Poland, who has received the most refugees, hasn’t had an uptick in cases. Countries that are accepting Ukrainian refugees are offering “health screenings, vaccinations, mental health support, and other health care at points of entry.”There may be an indirect effect, as headlines have taken the focus off COVID, so the pandemic may not be on the forefront of people’s minds.
Some have hypothesized waning of vaccination protection. However, cases in the U.K., for example, are increasing across each age group. Given that vaccines were rolled out by age, if vaccines were waning, we would only see this uptick among those who were vaccinated first.
Mainly, though, I think the uptick in European cases is driven by BA.2— the sister sublineage of Omicron. We typically see the impact of variants once they account for ~50% cases. Germany and the U.K. just recently reached this threshold (see light purple in figure below). Switzerland and Netherlands are close. Denmark, which has been slammed with cases over the past month, has been well past 50% for while.

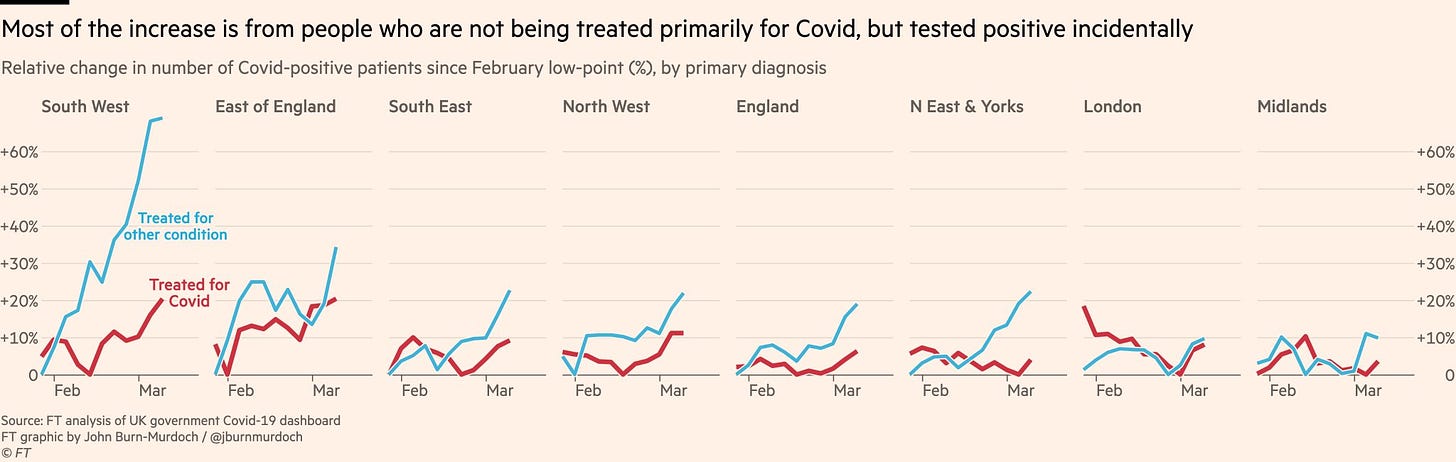
Typically hospitalizations lag cases by 3-4 weeks, but they too are already increasing in some parts of Europe, like the U.K. The fact that hospitalizations are not lagged in the U.K. may be explained by their high test positivity rate (>10%)—people are just not testing anymore and, thus, hospitalizations are sneaking up.
Thankfully, the U.K. has great vaccine coverage, with 92% of people having at least one dose and 67% boosted. So, as we see in the figure below, hospitalizations are mainly driven from “with COVID” (blue lines) compared to “for COVID” (red lines). While this does not signal an emergency yet, it does signal high transmission in the community and COVID is still a threat to the vulnerable.
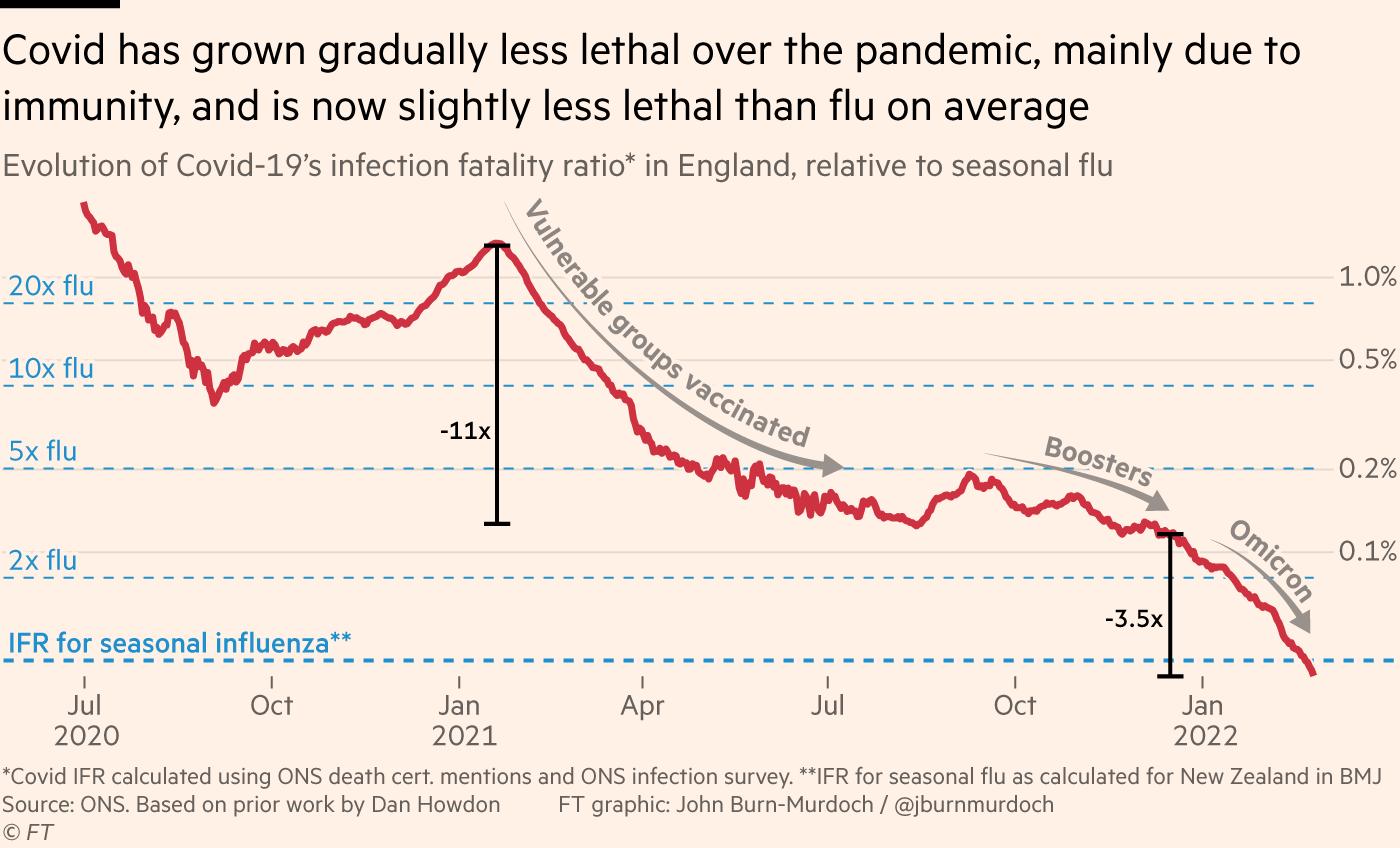
The U.K. also recently reached a huge milestone. For the first time ever, COVID is only as severe as the flu across all age groups. This represents phenomenal progress thanks to vaccine coverage in the U.K., infection-induced immunity, and a little luck from a less severe Omicron variant.
It’s really important to recognize, though, that risk of mortality is on an individual-level. COVID19 is far more transmissible than the flu and is not seasonal (yet), so population-level mortality is still higher than the flu, as seen in the figure below.
So, what does this all mean for the U.S.?
Throughout the pandemic, the U.S. has lagged Europe trends by a few weeks. Right now only ~10% of our cases are due to BA.2. But once this starts reaching the 50% threshold, we can expect cases to start increasing. This combined with removed mitigation measures should land us with an uptick in April/May.

The height of the uptick and the implications of such is dependent on a few things:
BA.1’s (the original Omicron) reach. Scientists estimated that Omicron reached about ~45% of Americans. Scientific studies have found reinfection of BA.2 after BA.1 is very rare. So, this leaves ~55% of Americans still susceptible to Omicron infection. Especially if these 55% of people are not boosted.
The height of the uptick will also be dependent on how well CDC’s new framework works and if people are willing to change behaviors, like wearing a mask again.
BA.2’s impact on hospital systems will depend on who Omicron reached in the first wave. If the unvaccinated and older non-boosted were reached during this past Omicron wave, our hospitals may be okay. But if they weren’t, then the hospital picture will be different. Our booster rate in the U.S. is suboptimal, especially when we compare to other European countries (see figure below). Does this mean that we will look like Hong Kong? Definitely not. But, hospitalizations may be higher than what we’re seeing in the U.K., for example.

Nonetheless, all eyes are on wastewater surveillance. In the past 15 days, 34% of wastewater sites on the CDC dashboard have reported an increase in viral detection. If these sites continue to increase and/or more sites report upticks, then it’s a great early signal of where cases may be going in the U.S.
Deltacron
The other thing peppering the news is a new variant that some have called “Deltacron.” The scientific name is AY.4/BA.1 recombinant. This variant was first discovered by Dr. Scott Nguyen, a scientist in D.C., who discovered that some French samples had a combination of Delta and Omicron properties. This was further verified in a number of other samples, including samples taken from the U.S.
While the combination of Delta and Omicron sounds terrifying, it isn’t of much concern right now. This is mainly because it looks like the virus is copying Omicron’s entire spike protein and pasting it onto the Delta skeleton (see Figure below). Because the spike protein determines immune invasion, the defenses that people have acquired against Omicron and/or our vaccinations should still work against this new recombinant. The other great news is that Deltacron hasn’t taken off yet. This means it’s probably not as transmissible as BA.2 and so it cannot outcompete. If this is the case, it will eventually fade away.
How does this happen? It is possible for people to be infected by two variants at the same time. This means that it is possible that two variants can enter a person’s cell at one time. When the virus tries to replicate inside the cell (to further spread to other cells), the genetic material can be mixed up. This would result in something like Deltacron.
Bottom line
As expected, the virus will continue to mutate. And, because it does, transmission across the globe will ebb and flow. But it’s getting harder and harder to know what one country’s pattern means for another country. The nation-wide implications will be very different dependent on vaccine coverage and mitigation measures.
Love, YLE
“Your Local Epidemiologist (YLE)” is written by Dr. Katelyn Jetelina, MPH PhD—an epidemiologist, biostatistician, professor, researcher, wife, and mom of two little girls. During the day she has a research lab and teaches graduate-level courses, but at night she writes this newsletter. Her main goal is to “translate” the ever-evolving public health science so that people will be well equipped to make evidence-based decisions. This newsletter is free thanks to the generous support of fellow YLE community members. To support the effort, please subscribe here:







You are absolutely phenomenal! I love your graphs and your explanations. And I realize that my next statement is not scientific but I believe that your daughters are absolutely blessed with the best💙
As for the potential April/May uptick, I’d love to hear your take on whether the rollout of Evusheld will affect that. My husband is now on the list to get it, and a friend who is a medical professional already got her first dose. They are both on ocrelizumab, so not the first “tier” of recipients, so I assume others who are more severely immuno-compromised are being treated now.