I’m back! Thank you for your patience and the thousands of messages of support and encouragement. (Someone even sent me an amazing banana muffin recipe to try). I read them all. And was, quite frankly, blown away. So, thank you.
I was about to press send on my newsletter this morning but woke up to the devastating news of war. Posting on a global pandemic felt insensitive without addressing a different kind of pain and suffering and tragedy that millions will soon face. Just like the pandemic, many will also fall victim to mis and disinformation—a new tool that enemies have found to work swimmingly well in a time of anxiety and confusion. Please be sure to find (and share) only solid sources; preferably ones with a reporter on the ground in Ukraine. There are such things as disaster epidemiologists, so I hope they come to the forefront too (email me!) to share the public health perspective of war or, more accurately, the devastating interaction between war and pandemic. This morning I’m hoping for peace, thinking about all of those in harms way, praying that leaders have the wisdom to guide us through, and hugging my girls extra tight.
Si quiere leer la versión en español, pulse aquí.
For those of you that want a break from war news coverage, here’s what has happened in the past two weeks of the pandemic. It can all be organized into three large buckets: Denmark, BA.2, and boosters.
Denmark
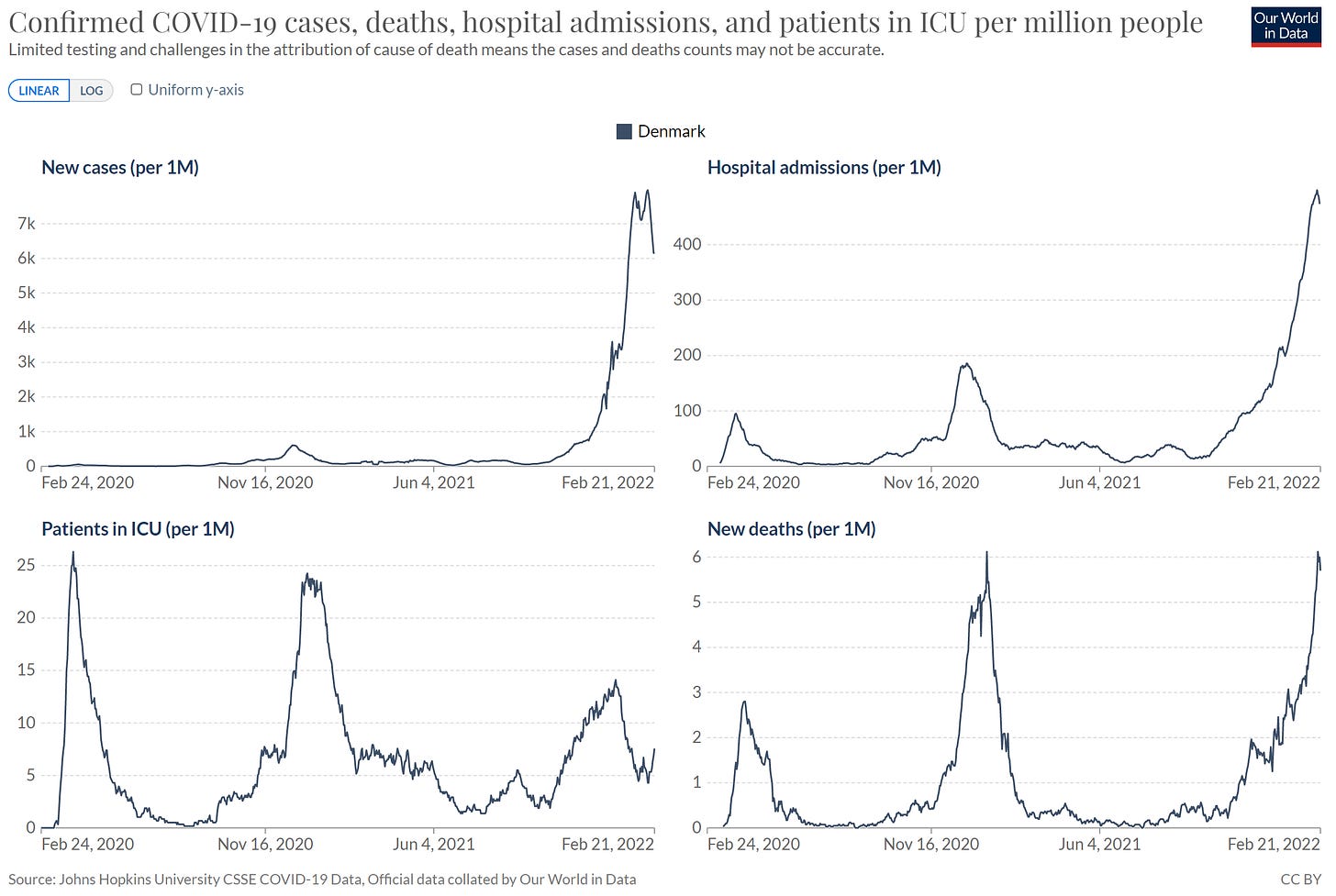
After initially escaping the Omicron wave without overwhelming hospitals and very little mortality, Denmark decided to remove all public health mitigation measures in the beginning of February. This decision was made regardless of their exponential, out-of-this-world COVID-19 transmission rate at the time.
While controversial (and risky), the policy decision provided the world a front row seat to a natural experiment: Are Denmark’s vaccination rates (10th most vaccinated and 4th most boosted population in the world, which equates to a 83% vaccination rate overall and 62% booster rate) high enough to go back to “normal” despite a massive case surge? What would this look like?
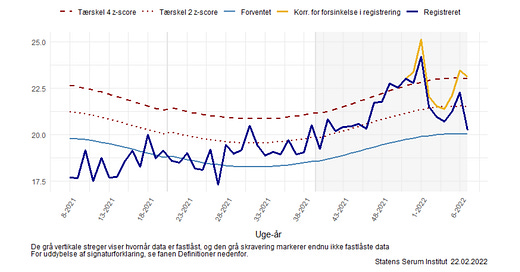
Well, to no one’s surprise, cases continued to skyrocket. Interestingly, ICUs decreased but then plateaued and just recently began increasing. Denmark’s deaths continued to exponentially increase. In fact, just recently they reached a record-breaking high.
Many people specifically focused on exponential deaths: did Denmark make a mistake? There are two camps of thought:
Some continue to support Denmark’s decision. This was specifically the case after the Danish Health Authority clarified an important caveat: official Danish death counts combine those that died “from COVID” and died “with COVID.” After stratifying deaths by cause (see figure below from a Danish report), it’s clear that mortality composition has shifted in this wave compared to previous waves. Some think the mortality rate “from COVID19” is now low enough to warrant dropping public health measures altogether.
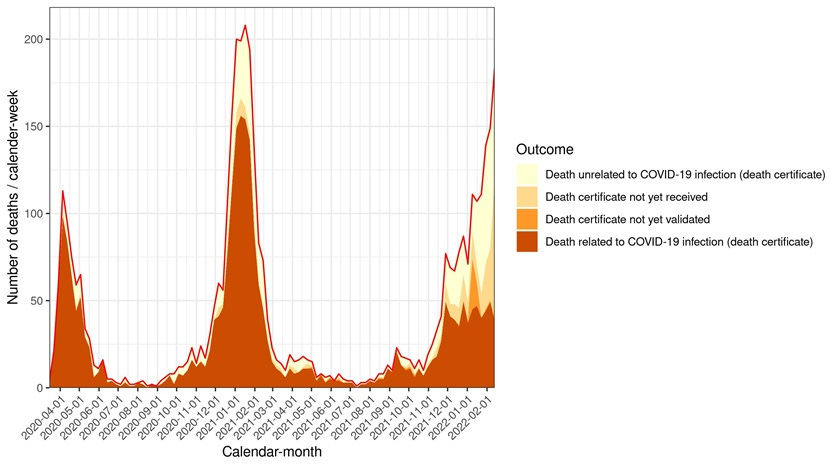
On the other hand, many believe the Danish policy was a mistake. One reliable signal of the severity of the pandemic is excess mortality, as it removes all the noise from case definitions. Denmark’s report this week found a substantially high number of excess deaths, particularly among those aged 85+ years old. Unfortunately, this data is delayed, so excess deaths may continue to increase, too. This confirms that even though there is a high vaccination rate, the vulnerable are not guaranteed protection in a high transmission environment. Vaccines work great, but are not perfect.
Vaccination rates play a big role, but as Denmark has shown, it’s not the only factor at play. Other country-level factors like general health, age distribution, strength of a healthcare system, and the availability social safety nets also need to be taken into account. The country also needs to decide how much excess death and excess morbidity (long COVID19) they’re willing to culturally accept.
This public health policy debate is an important one, as the public is constantly looking for a goalpost: When can we go back to “normal”? We first need to recognize that we have a new virus in our repertoire, and we aren’t going back to 2019 normal. How we move forward, though, is a legitimate question and a decision that needs to be made country by country. As Dr. Mike Ryan said yesterday at the WHO press conference, “If countries start parroting each other and just doing what the other guy or girl did, then they’re going to find themselves in real trouble.”
The U.S. is not Denmark. The U.S. currently ranks a measly 64th for “fully vaccinated” and 54th for boosters in the world. Right now, 1,960 Americans are dying each day, which continues to add to excess death (see Figure below from the Guardian). We also have a fragmented healthcare and public health system, and little-to-no safety nets. The conversation on how to control the virus and prepare in the U.S. is still important and very much needed. Dropping all public health mitigation measures now and forever is just not a choice we have.
BA.2
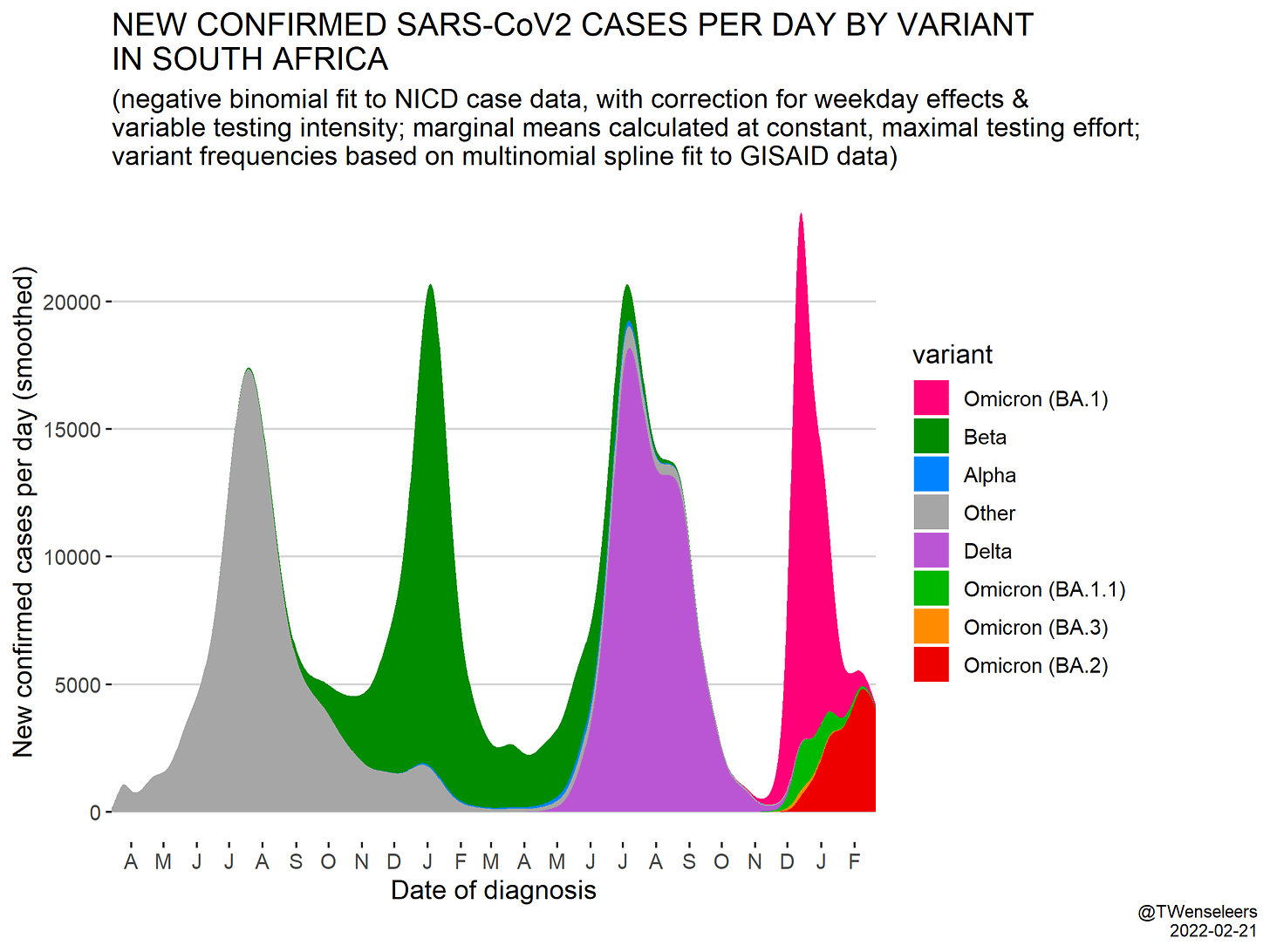
In the past two weeks we’ve also gotten more scientific clarity on BA.2. As a reminder, Omicron (called BA.1) continues to mutate as expected, but one of the sublineages (called BA.2) caught the attention of many scientists due to a number of concerning mutations. Since my last update, we’ve learned more about this sister lineage:
Transmissibility. We now have consistent data showing that BA.2 outcompetes BA.1. A recent study found the global reproductive rate of BA.2 was R(t)= 1.4 compared to BA.1, which had a R(t)=1.1. In England, secondary attack rates in U.K. households are also higher: 13.4% of BA.2 cases transmitted within their households vs 10.3% of BA.1. Together, this means that BA.2 will become the dominant variant worldwide very soon.
Immunity escape. In a recent lab study, immune escape was similar for BA.2 compared to BA.1. In the real world, we have evidence that boosters continue to work against BA.2, but just like BA.1, protection against infection wanes over time (see Table below). A study of Denmark households found that vaccination helped protect against transmission more for BA.2 than BA.1. So, vaccines continue to work against BA.2. This is not surprising but sure is great news.
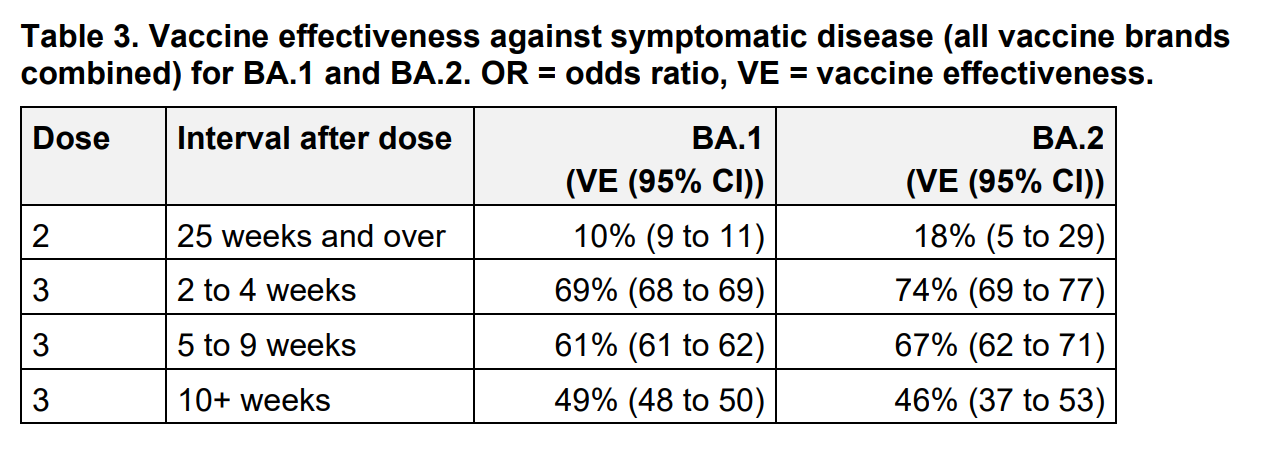
UK Health Security Report Source Here What about infection-induced immunity? A recent preprint from Denmark found that BA.2 reinfections after BA.1 infection were rare, but much more common among unvaccinated compared to vaccinated: of the 47 reinfections, 89% were not vaccinated and 6% had only the two-dose series.
Severity. We’ve gotten mixed signals as to whether BA.2 induces more severe disease than BA.1. A recent lab study in Japan found that BA.2 is more severe in hamsters. Hamster models have helped us out a lot in the past, but they certainly have limitations. A “real world” study in South Africa found something different: BA.2 had similar risk of hospitalization as BA.1. Because hamsters are not people, and because the lab is not the real world, I tend to have more confidence in South Africa’s conclusion that BA.2 is not more severe than BA.1. But we definitely need confirmatory analyses from other countries.
Taken together, we thought BA.2 would extend the tails of the Omicron wave. Many countries, like South Africa, did see the tail of the epidemic extended a little, but BA.2 did not cause a huge case upswing. Which is great news.
Another booster?
Over the past two weeks, conversations have bubbled up about the need for another booster. As far as I can tell, the triggering event for these discussion was a recent U.S. study published in MMWR. This study analyzed data from a network of hospitals across 10 states during August 26, 2021–January 22, 2022. The scientists wanted to evaluate mRNA vaccine effectiveness (VE) against hospitalizations over time. What did they find?
Two doses: VE for hospitalizations was 93% <2 months of a booster → VE was 80% >4 months after a booster
Three doses: VE for hospitalizations was 95% <2 months of a booster → VE was 81% >4 months after a booster
So this study showed that vaccine effectiveness against severe disease waned over time, regardless of a 2- or 3-dose series. Is this a sign that the booster did not solidify long-term effectiveness like we hoped? Maybe. But there are some significant limitations to this study. For example, the data was not stratified by age or health status. Those over 65+ years or immunocompromised may disproportionally contribute to waning. If that’s the case, this study doesn’t necessarily support a broad fourth dose policy. There was also a very small sample with very limited follow-up data: only 39 people in the study had a booster for more than 4 months. This means there is a lot of uncertainty in the statistics. We really need a more robust study to see whether there is a “true” waning signal.
Cue Kaiser Permanente. They published a study this week in Nature. (Note that the study was funded by Moderna). Kaiser has an incredibly extensive database because of their closed health system, making this sort of study among a huge population feasible. The scientists leveraged a sample of over 26,000 patients to assess VE against infections and severe disease. What did they find?
Protection against infection waned, regardless of booster status. This is no surprise and another indicator that we really need to shift our focus away from infection to severe disease.
During Delta, VE of 2 and 3 doses against hospitalization was ≥99%.
During Omicron, VE of 2 and 3 doses against hospitalization was 84.5% and 99.2%, respectfully.
The 4 people hospitalized with Omicron despite three mRNA doses were more than 60 years of age with chronic diseases, and one was also immunocompromised. (Immunocompromised people really need to get their fourth dose!)
The number of boosted hospitalizations in this study was so low researchers were not able to measure any possible waning.
This study shows that vaccines and boosters continue to work incredibly well against severe disease. But limitations also exist with this study. There was limited follow-up time to properly evaluate waning against severe disease. This was also an insured population, meaning it’s not a great representation of the general U.S. population.
In addition to the Kaiser study, data from the U.K. continues to show a three-dose mRNA series continues to protect swimmingly well against hospitalization. However, they also only have 14 weeks of follow-up data after a booster, so we are at the mercy of time to see if boosters do in fact start waning like the primary series. So far, in the U.K., it doesn’t look like they do.

So, do we need another booster right now? No. Do we need another one soon? Before next winter? Ever? No one knows. That decision will be highly dependent on the duration of protection, how protection changes due to occupation, age, health, and, probably the most important factor, how this virus continues to mutate.
Bottom Line: Denmark is providing an interesting natural experiment, but the U.S. is not Denmark. BA.2 is something to keep an eye on, but I’m not too concerned. I’m more concerned about another variant popping out of nowhere like Omicron did. The booster story will continue to evolve as long as this pandemic continues to evolve.
Love, YLE
“Your Local Epidemiologist (YLE)” is written by Dr. Katelyn Jetelina, MPH PhD—an epidemiologist, biostatistician, professor, researcher, wife, and mom of two little girls. During the day she has a research lab and teaches graduate-level courses, but at night she writes this newsletter. Her main goal is to “translate” the ever-evolving public health science so that people will be well equipped to make evidence-based decisions. This newsletter is free thanks to the generous support of fellow YLE community members. To support the effort, please subscribe here:






It's great to have you back!!