Okay, mamas. I did some digging tonight and found all the data on we have, thus far, on COVID19 vaccines and pregnancy/lactating. There are currently three sources of rich information.
Bottom line: It’s looking good.
Note: This is important because pregnant and lactating people were excluded from vaccine trials (this is normal but this decision is consistently debated among scientists). So, we are at the mercy of time to see “real world” data. This post is based on mRNA vaccines; we do not have J&J data yet.
ACIP
On March 1, the ACIP (Advisory Committee on Immunization Practices) at the CDC met to discuss updates on COVID-19 vaccines. The meeting minutes are here. Buried in those presentations, were slides regarding of safety data for vaccinated pregnant women:
30,494 pregnant women have gotten the vaccine and registered in CDC’s V-safe
These people are then called and invited to participate in a study (they are asked to be followed throughout pregnancy, at birth, and 3 months after birth). As of mid-Feb, 1,815 women were enrolled.
In this study, they have found a few things so far…
Pregnant people with the vaccine had the same side effects as not pregnant
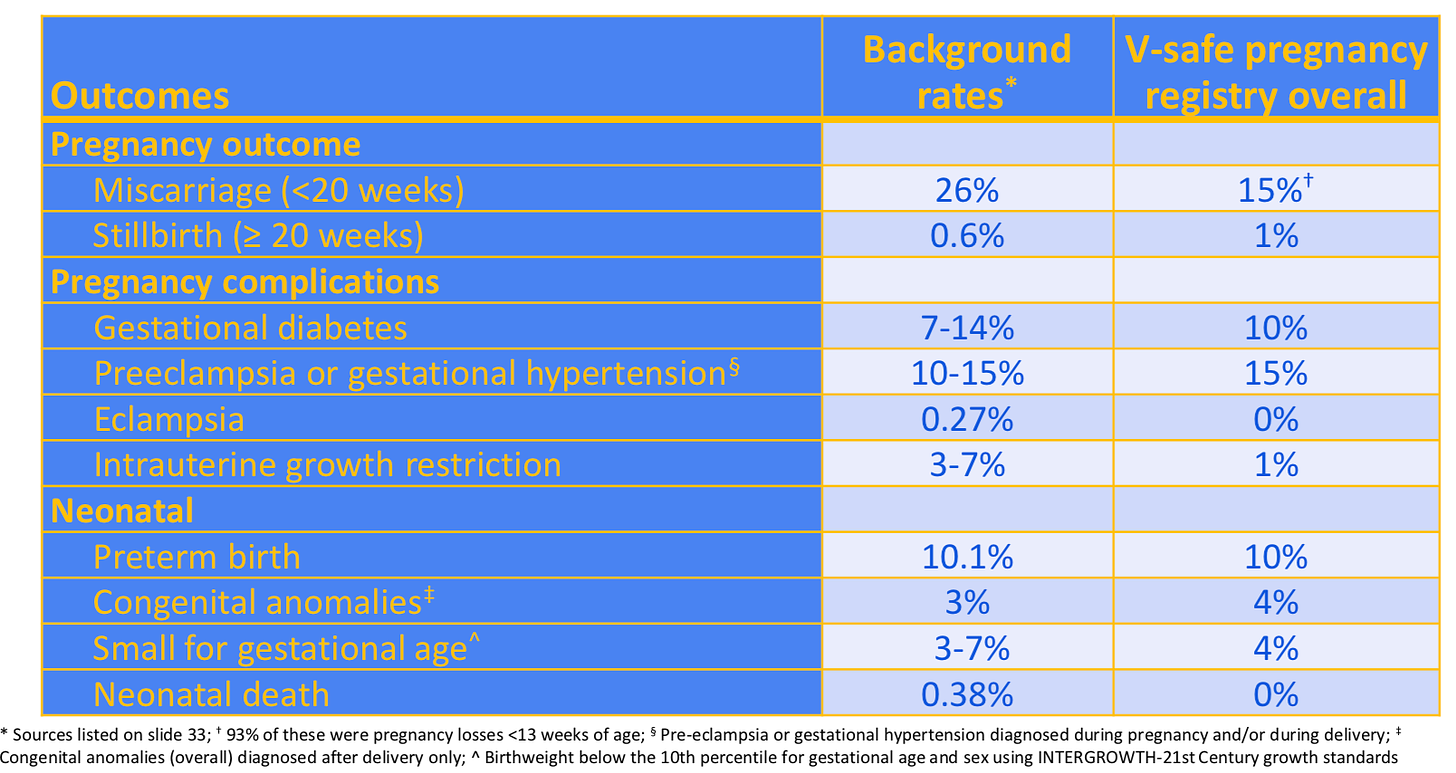
No unexpected pregnancy or infant outcomes have been observed related to COVID-19 vaccination during pregnancy. The rates in the general public are included in the table for easy comparison (labeled “Background rates”).
American Journal of Obstetrics and Gynecology (AJOG)
On March 25, a study was published in a highly regarded scientific, OBGYN journal. The scientists enrolled 131 vaccinated women (84 pregnant, 31 lactating, and 16 non-pregnant) between December 17, 2020 and Feb 23, 2021. The scientists compared vaccinated pregnant women to two groups: 1) unvaccinated pregnant women and 2) “naturally” infected pregnant women.
This is what they found:
Among the pregnant and vaccinated, 13% received their first vaccine dose in the first trimester, 46% in the second trimester, and 40% in the third trimester.
Antibody levels were the same in pregnant and lactating compared to non-pregnant women
Antibody levels were higher among vaccinated compared to “naturally” infected pregnant women
Antibodies were present in all breastmilk samples
The second vaccine dose increased a specific type of antibody (IgG but not IgA) in maternal blood and breastmilk (which was expected)
Vaccine-related fevers/chills were reported by 32% of pregnant women after the second dose and 50% of non-pregnant
13 people delivered babies during this study period
All 13 were vaccinated in the 3rd trimester (which makes sense, because they delivered during the study period, which was only 2 months)
Antibodies were present in all umbilical cord blood samples
One participant delivered 17 days after vaccine 1, with spontaneous preterm labor at 35 weeks’ gestation
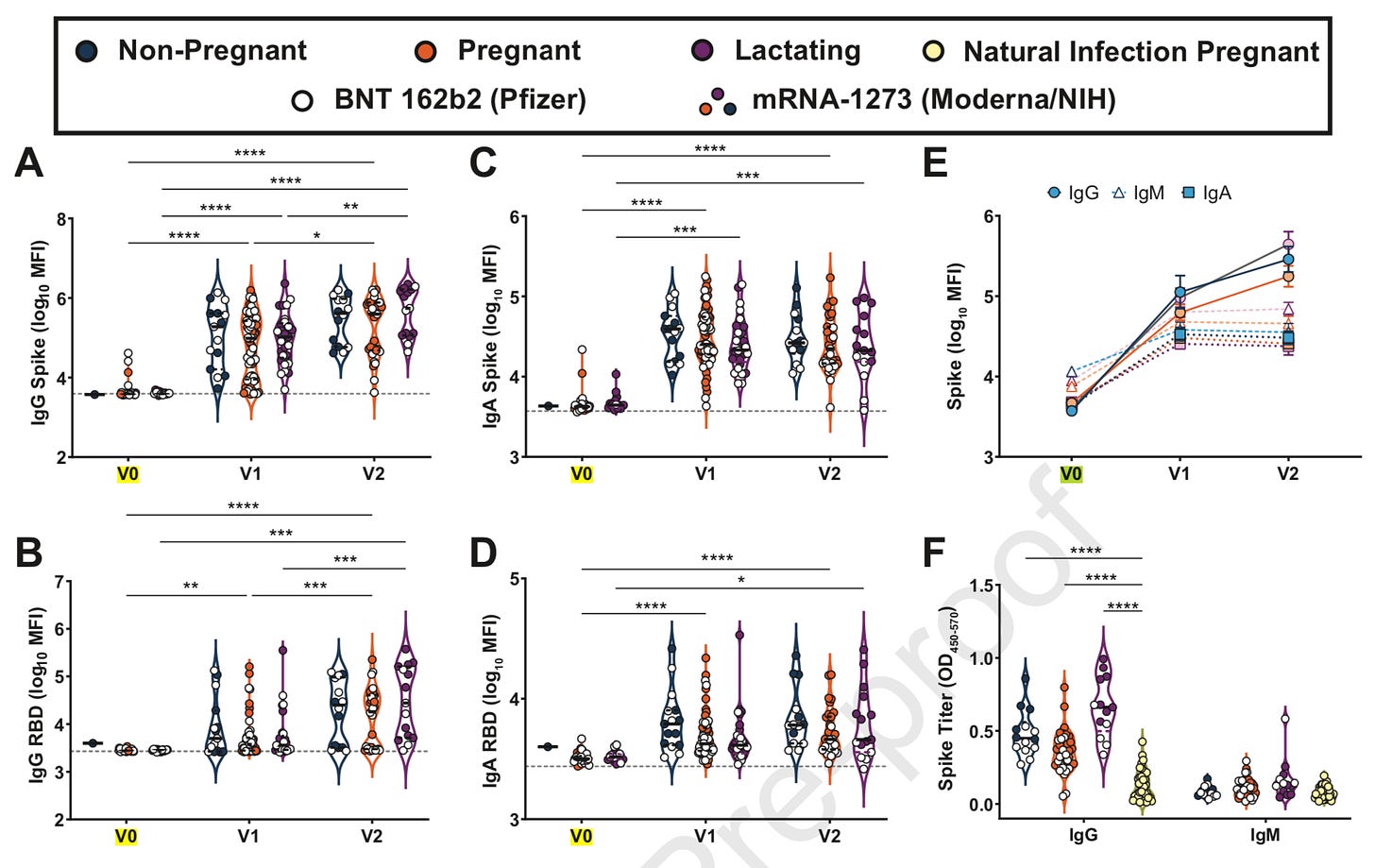
Here is a figure from the paper. Don’t let it scare you off (it scared me off at first). I’ll walk you through two panels.
Panel A: At baseline (i.e. V0=no vaccine protection), antibodies were low across non-pregnant people, pregnant people, and lactating. When participants got the second dose (V1), antibodies were high across all three groups. Then, 2 weeks after the second dose (V2=fully protected), all three groups had even more antibodies. This is fantastic news.
Panel F shows that antibodies were higher among vaccinated (blue, purple, orange dots) compared to “naturally” infected people (yellow dots). Also, great news.
Developmental and Reproductive Toxicology Study (DART) studies
We do have data from Pfizer, Moderna, and J&J DART studies. These are small animal studies that are required before studying vaccines among pregnant humans. Scientists basically give pregnant rats the vaccine and see how they do. What did they find?
Rats did not have any adverse effects on female reproduction, fetal/embryonal development, or postnatal developmental. We are not surprised, but still good to know.
Other Helpful Links
Fertility and vaccine previous post here
Pregnancy and mRNA vaccine previous post here
Mom to baby transfer of antibodies previous post here
HERE is a great decision tool to help you (if you’re pregnant) decide whether or not you should get the vaccine. A group of experts in the fields of OB/GYN, Maternal-Fetal Medicine, Shared Decision-Making and risk communication, Emergency Medicine, and current COVID-19 research at the University of Massachusetts Medical School – Baystate made a decision aid to help individuals who are pregnant, lactating, or planning on becoming pregnant decide whether or not to receive a COVID-19 vaccine (in conjunction with their healthcare providers). At this site you can get the decision aid in 10 languages.
Hope this is helpful!
Love, YLE (and a fellow mama)






Did they study anything else about the lactating people? Besides just the presence of antibodies in their milk? I wish we had some more information for lactating people like me to help us decide if/when to get vaccinated.
Thank you. My niece is in her second trimester. I will be sharing this with her and our family 🙏🏻