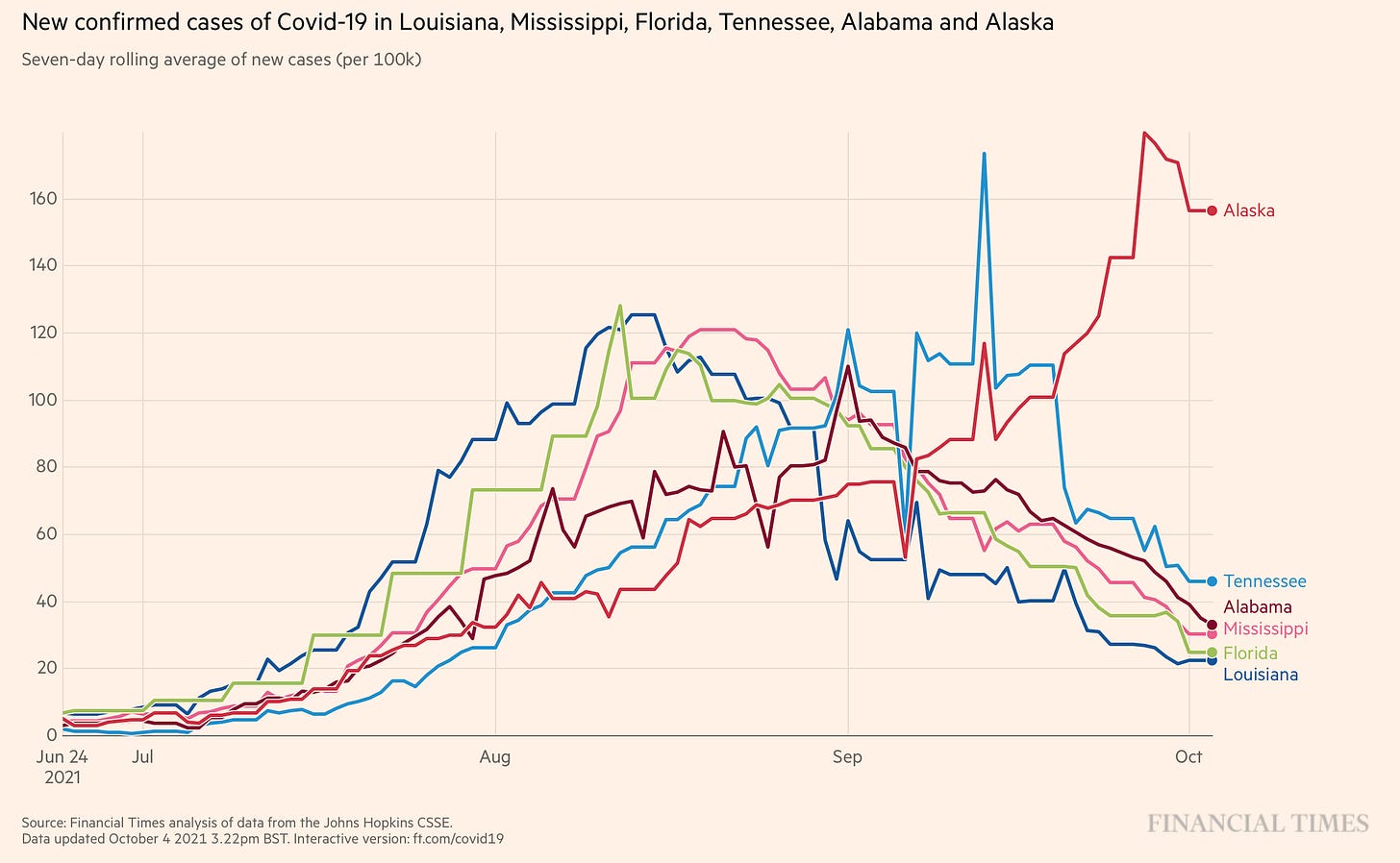
For the first time since mid-summer, all indicators (test positivity rate, cases, hospitalizations, deaths) in the United States are decreasing. A welcome ending to this Delta wave. And while some states are still experiencing upswings (Alaska & North Dakota), the early Delta leaders continue to recover.
Interestingly, this Delta wave had a distinct pattern: 2.5 month flare of virus until retreat. We saw the same pattern across the world, too (with a few exceptions). So, why the 2 months? Why does the pandemic ebb and flow in waves?
Previous Pandemics
Early in the SARS-CoV-2 pandemic, Drs. Tom Jefferson and Carl Heneghan (scientists at the University of Oxford) summarized respiratory pandemics over the past 150 years. They highlighted:
The last five outbreaks, since 1957-58, occurred in the space of two years;
Five outbreaks are described as having a second wave;
2009-10 had two mild phases;
1957-58 had two phases that were equally severe;
1889-92 and 1918-20 had two phases with the latter being described as more severe.
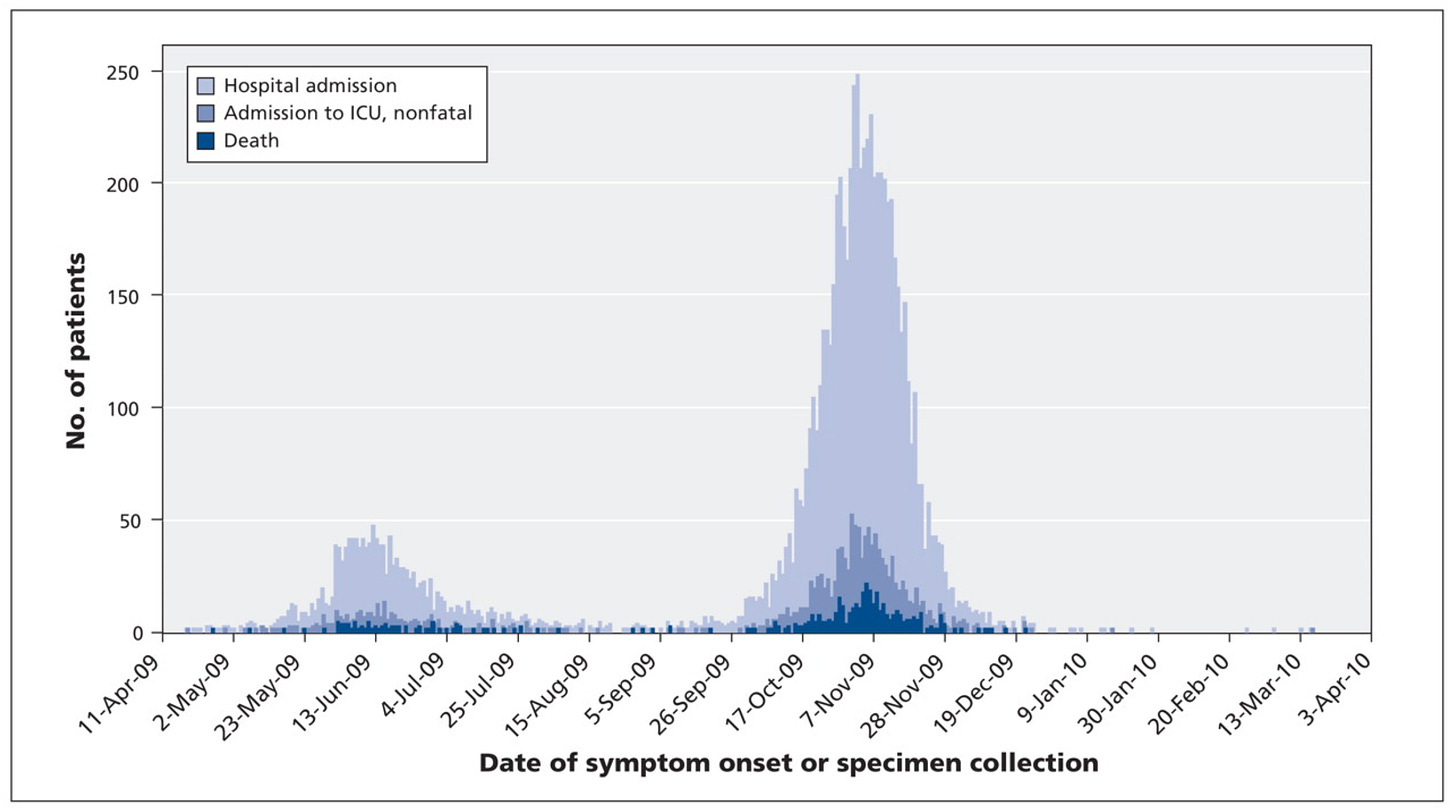
So, epidemic waves are relatively common. During the 1918 pandemic, the world was hit with three waves between Spring 1918 and early 1919. During the 2009 H1N1 influenza pandemic, there were two distinct waves.
But each wave wasn’t the same. For example, during the 1918 pandemic, the second wave was much more severe in younger adults. During H1N1, older people with underlying conditions were more likely to go to the hospital in the second wave compared to the first.
Why do we have waves?
Why doesn’t the virus just spread and spread until it has no more people to infect? It’s a simple, legitimate question with a very complicated answer: We don’t know. There’s no scientific consensus on why this happens. We hypothesize it’s largely driven by the combination of four factors:
Human behavior: Once numbers start increasing, people start changing behavior (whether they know it or not). Even modest restrictions can bring numbers back down, like masking or cancelling plans. People did take the Delta wave seriously. The Kaiser Family Foundation reported an uptick in vaccinations due to Delta, hospitals filling up, and knowing someone who got seriously ill or died due to Delta. Human behavior plays a big role in wave patterns.
Social networks: This plays some sort of role too (and I think the most interesting). As people see their regular contacts and these networks reassert themselves, Delta runs out of places to go. This is highly dependent on how and where people mix. As we all know, schools just started, which would open social networks (not limit them). So this may only play a limited role with Delta.
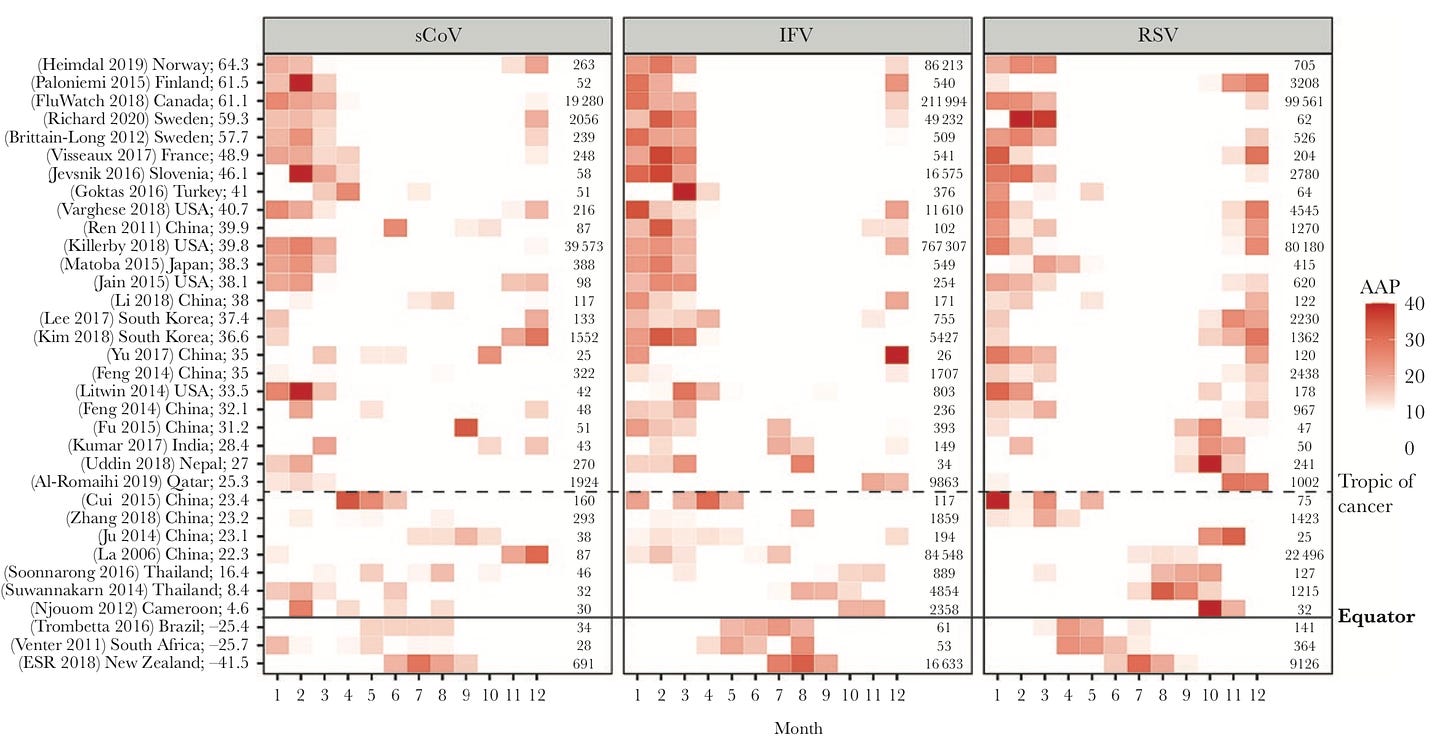
Seasonality. During non-pandemic times, most coronaviruses are seasonal. Other viruses, like the flu, are seasonal because of climate patterns (and human behavior). It’s not a coincidence that our largest COVID19 wave was during the Winter months. But, again, this doesn’t fully explain all waves, as we had some during the summer months too.
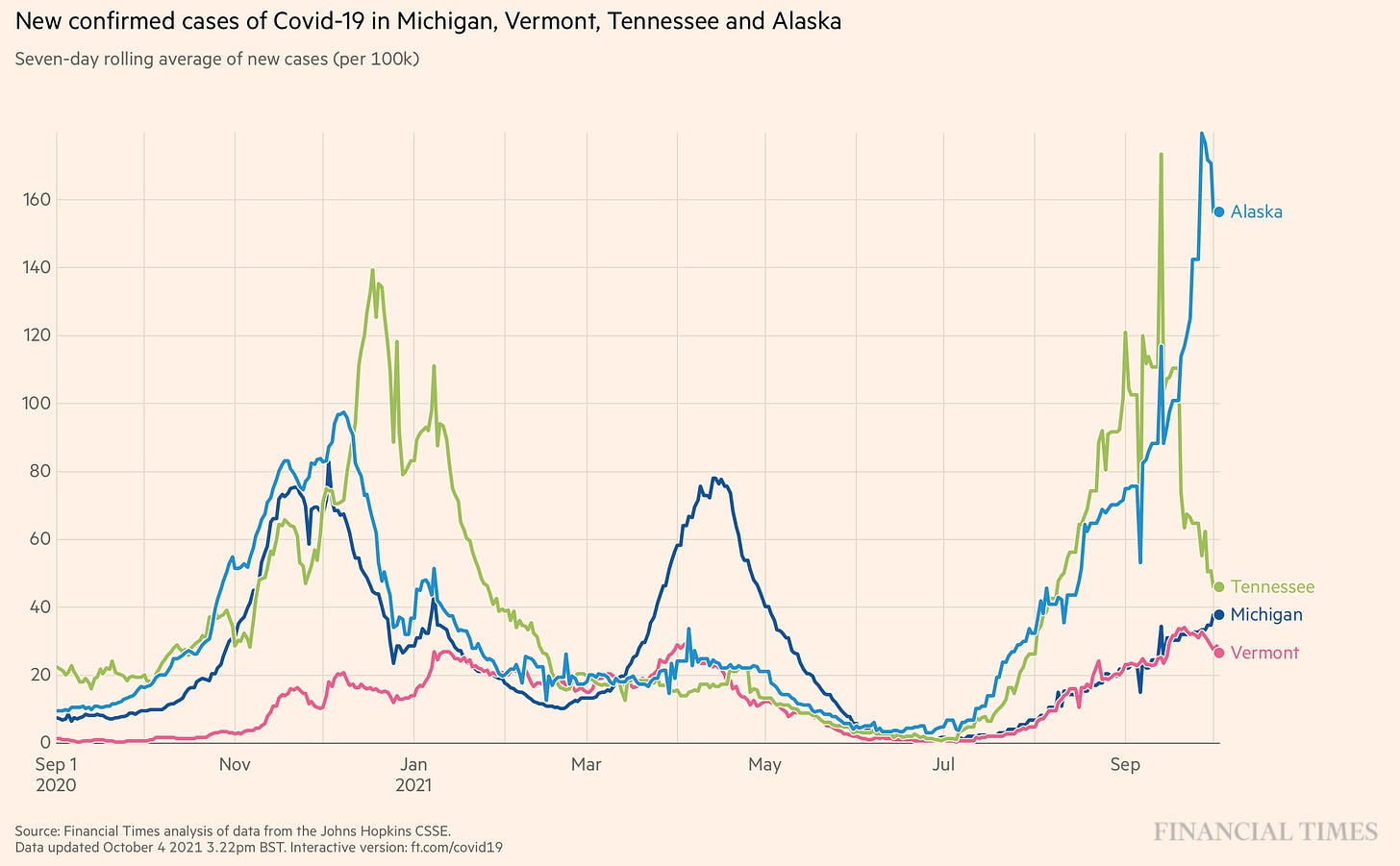
Levels of Vaccine and/or Natural Immunity. As more people become immune, spread slows and the virus eventually stops because it runs out of people to infect. We, no doubt, saw this with vaccine rates and Delta. Highly vaccinated states, like Vermont (70% population fully vaccinated), came out relatively unscathed. As far as natural immunity, we saw this in Michigan. Michigan was hit hard with Alpha in April, which likely provided some protection against Delta. But Michigan numbers are starting to increase now, so we need to keep an eye on this.
Other factors: And there are likely many other reasons that play a less dominant role, like testing patterns (antigen becoming more dominant; less testing due to pandemic fatigue) and humidity.
Is this the last wave?
No one really knows, but it could be. At this point it’s certainly partially (if not fully) dependent on the durability of natural immunity.
This week the Lancet published a study that used data on other coronaviruses evolutionarily close to SARS-CoV-2 to estimate times to reinfection. The study confirmed what we already knew: the durability of natural protection is highly variable. For some people, natural immunity lasts only 3 months and for others it could last up to 5 years. The median protection is 16 months, though.
So if the majority of Americans were naturally infected in the 3rd and 4th waves of this pandemic, we may have enough protection to get us through Winter. Reinfections will eventually get more and more common, though. And we have no idea who’s protected and who’s not.
We started to already see this phenomenon in the UK. Recently, the UK Delta wave started to decrease, but on its way down it changed course and started increasing again. This is due to a myriad of factors, but interestingly as Dr. Paul Hunter (adviser to the WHO) pointed out in a recent NYT article:
“The [UK] rise has been driven by outbreaks in regions that had seen relatively few cases earlier in the pandemic and, therefore, had less naturally acquired immunity, including southwest England and rural parts of Scotland and Northern Ireland.”
So, will this be the final wave in the United States? We’ll just have to wait and see.
Love, YLE
The FDA announced that VRBPAC (external scientific advisory committee to the FDA) will meet to discuss the following topics:
October 15: Moderna booster
October 16: J&J booster; and mixing and matching vaccines
Oct 26: 5-11 year old vaccine
If VRBPAC votes in favor of these, then the ACIP and CDC will review the data a few days later. Then, if that goes well, approval could be given within 24 hours. (However, I’m still not clear how pediatric vaccines will be distributed. I assume they could be mixed for the new formula on site at pharmacies, but this hasn’t been determined yet.) I’ll be at these meetings and, as always, provide cliff notes.







I've not reviewed the Lancet article regarding immunity. Last paper I can recall on the subject, I was willing to accept an 8 month median value; 16 months is a bit of a game changer. IF it is correct. A consideration is that we do not yet have studies that will tell us what Delta did for immune response and cellular activation.
I think we're looking at a minimum of 4-6 months of relative quiet, or, 4-6 months where the public can think we've beaten the virus and drop all precautions, stop getting vaccinated and then wonder what hit them when the next variant arrives. We have to recall that only a fraction of the world's population is fully vaccinated, leaving a significant breeding ground for new variants. Statistically, some of those have to be evolutionarily better adapted to transmission and infection than what we've seen, and some will likely have protein conformational changes that affect how our existing antibodies respond.
We also have the quandary that the public now expects (I don't know why) sterilizing immunity to ALL variants of COVID-19 rather than protection from significant disease and death. I expect the next wave to be accompanied with complaints that we (scientists) missed the mark again.
Thank you for mentioning Michigan. I am in the Mitten State and am wondering why our Delta numbers are lagging behind ... I fear that our wave is just building. Our vaccination rate is close to Alaska's and I am thinking we'll fare no better. It's a tight race to see if my 8 year old grandson can get the vaccine before getting Delta ... very disappointing to see that the pediatric vaccine discussion pushed back.