For the past two days, ACIP—the CDC advisory board—met to discuss COVID-19 vaccines among children. Actually, this was one of their three regularly scheduled annual meetings, so they discussed many vaccines. Here are the cliff notes re: the COVID-19 ones as there seems to be a ridiculous amount of misinformation circulating.
Adding COVID-19 to the vaccine schedule
The biggest piece of news was that ACIP voted unanimously to add COVID-19 to the pediatric vaccine schedule. What does this mean? CDC adds the COVID-19 vaccine to the Vaccines for Children program. This means that when the federal government stops purchasing vaccines (funds are all but exhausted), kids without health insurance can still get them for free. This is incredibly important for health equity.
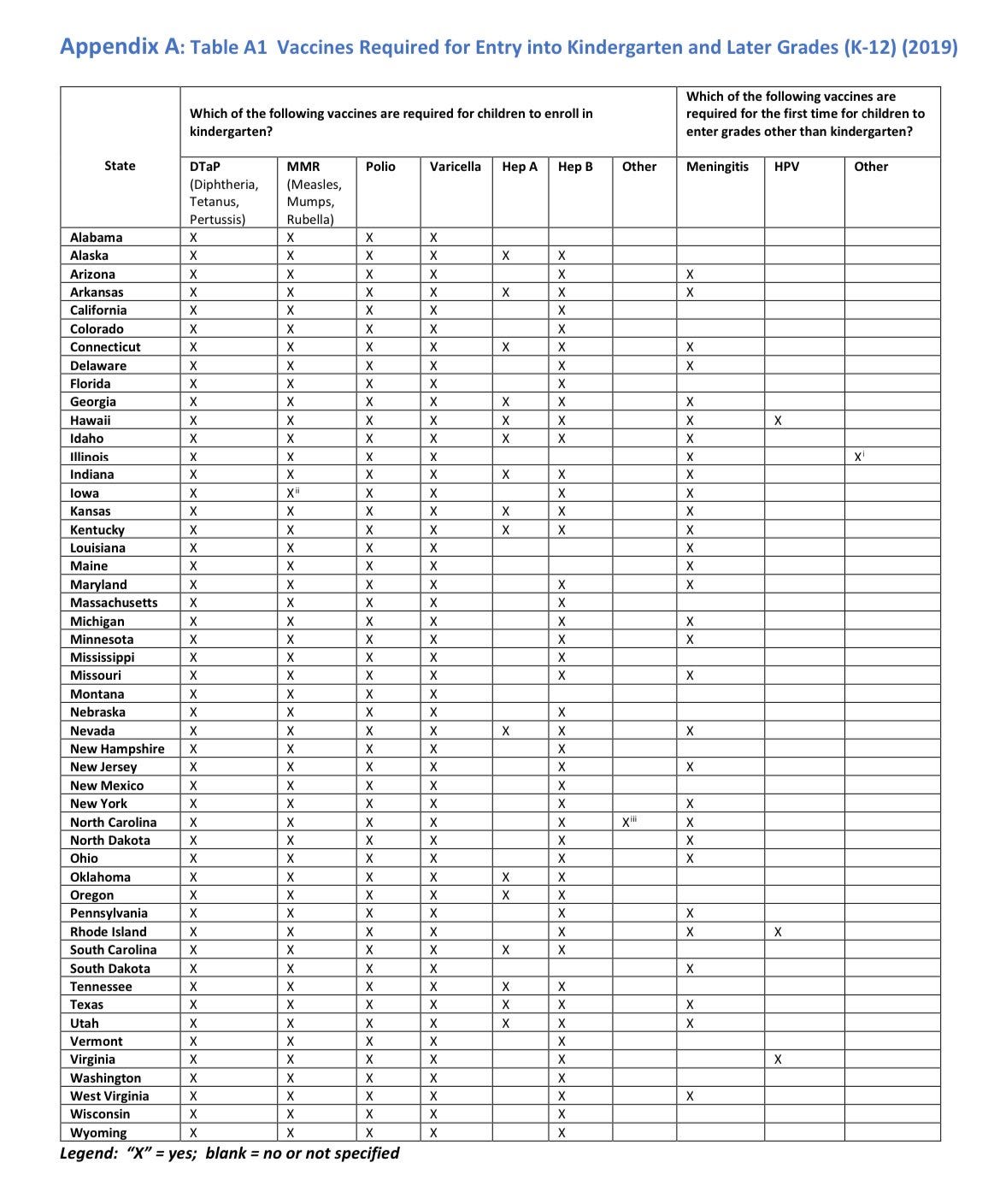
This does not mean the CDC is mandating vaccines for schools (looking at you Tucker Carlson). In fact, the CDC has no say in this. This is done on the state and local level. Some states may decide to mandate the vaccines, but some states will not. (This is why vaccine mandates, overall, are not uniform across the country, as shown in the table below.)
COVID19 hospitalization and myocarditis
The hospitalization rate among children aged 6 months-4 years remains the highest compared to other pediatric age groups. This is likely due to suboptimal vaccination.

Because so much was packed into the meeting, there was no formal myocarditis benefit/risk analysis (as I had hoped). But ACIP clearly stated that they regularly conduct this analysis (6 times in total, with the last one on September 1, 2022) and “each time ACIP has determined that the benefits outweigh the risks”. They presented some quick statistics:
No evidence of an increased risk for myocarditis following mRNA vaccination in children ages 6 months–5 years
Risk of myocarditis is rare in adolescent and young adult males within the first week after receiving the mRNA vaccine
The risk of adverse cardiac outcomes were 1.8 – 5.6 times higher after SARS-CoV-2 infection than after mRNA COVID-19 vaccination among males ages 12 – 17 years
Interval of 8 weeks between vaccine doses may further lower myocarditis risk
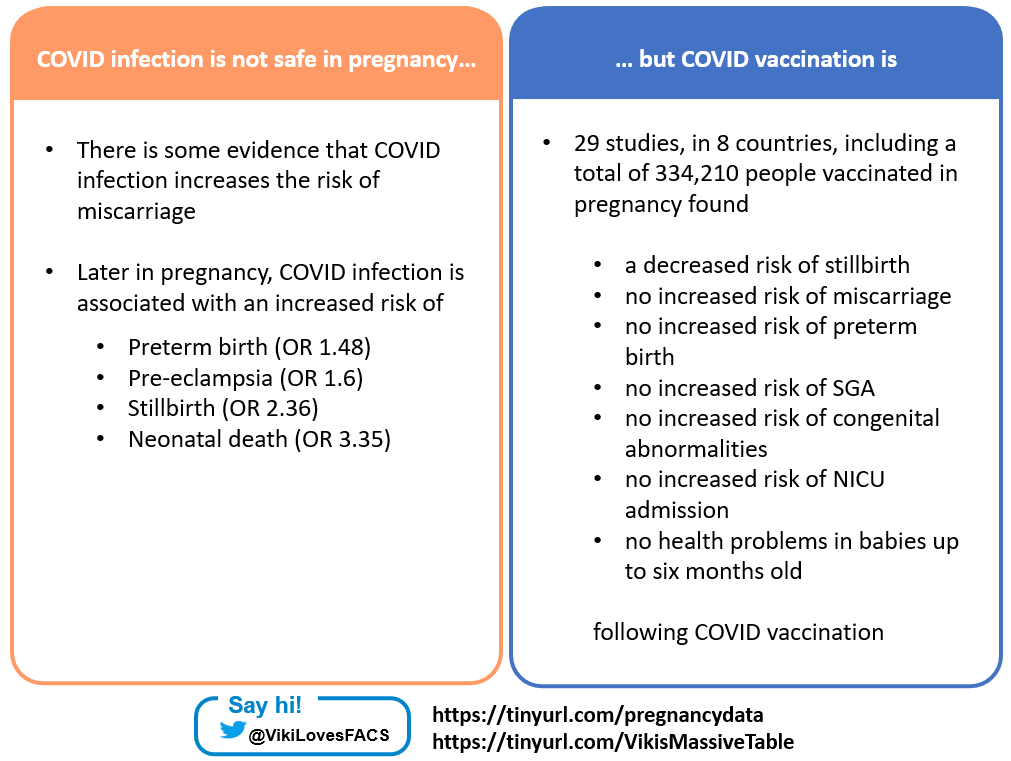
Pregnancy safety data and effectiveness
ACIP provided an update on the safety of COVID-19 vaccines for pregnancy. This data continues to look solid. At this point, there is literally no question that the vaccines are incredibly safe during pregnancy and incredibly important for the mother and fetus/child. A previous post of mine covered a lot of the specific scientific studies, but this is what the CDC had to update. Here were their takeaways:
The CDC tested for outcomes by vaccine type and timing of vaccination and found no evidence of any differences. In other words, it’s safe if pregnant people get Moderna or Pfizer. It doesn’t matter which one.
For the first time (that I’ve seen), CDC presented the effectiveness of mothers’ vaccines on newborn hospitalizations. Overall, effectiveness of the mother’s vaccination in preventing hospitalization of the child after infection was 80-90% during the Delta wave and 60% during the Omicron waves.
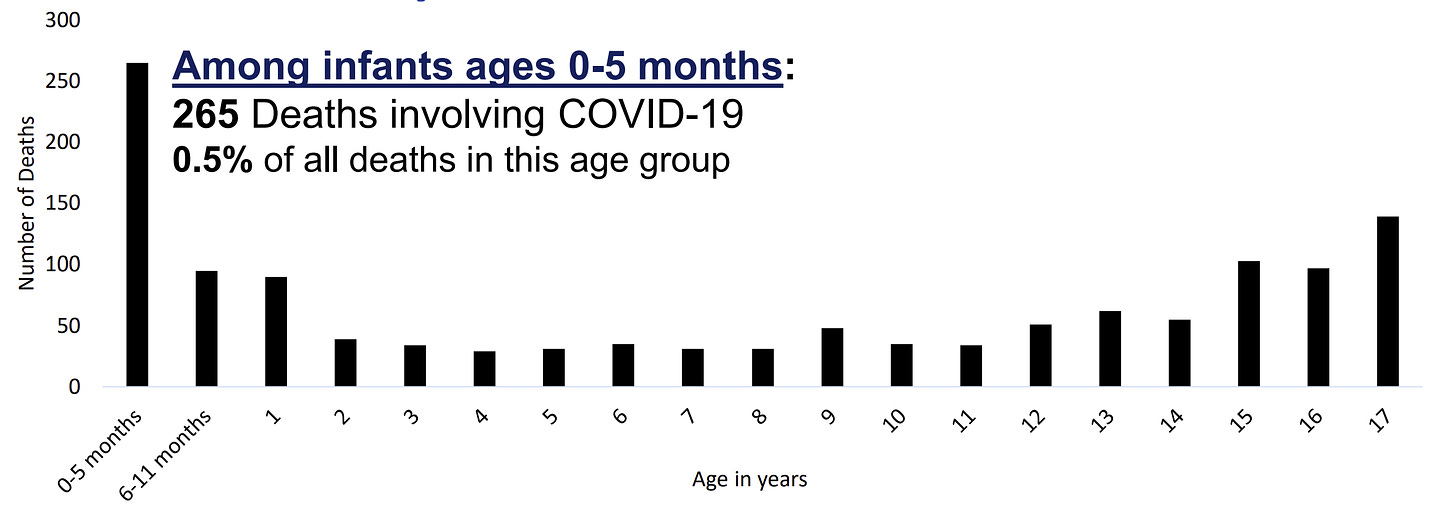
This is fantastic news, especially given infection among children aged 0-5 months is leading to much higher hospitalization rates than the flu (see graph below). Among those hospitalized, only 24% had an underlying health condition.

Also, the rate of deaths from COVID-19 infection is higher in this group. Among infants aged 0-5 months, 265 deaths involving COVID-19 have been reported. We need to get more pregnant people vaccinated.
Other updates
Parents and pediatricians may be interested in some other news that was presented at the ACIP meeting:
Polio vaccines, and specifically the oral vaccines, are being considered in the United States given that our current vaccines do not stop transmission. Nothing was decided, but another vaccine recommendation for everyone may be coming down the pipeline.
RSV vaccines, made by GSK and Pfizer, presented results from their clinical trials. Effectiveness looks nothing short of amazing: 82% efficacy rate for GSK and 86% against severe disease for Pfizer. There may be a rare safety signal of Guillain-Barré syndrome (1 in 15,000 children) for both of them. We really need RSV vaccines.
Bottom line
No surprises from the ACIP meeting. Vaccines are safe. They are effective. Everyone over the age of 5 is now eligible for the fall COVID-19 booster, so get one!
Have a great weekend,
YLE
“Your Local Epidemiologist (YLE)” is written by Dr. Katelyn Jetelina, MPH PhD—an epidemiologist, data scientist, wife, and mom of two little girls. During the day she works at a nonpartisan health policy think tank, and at night she writes this newsletter. Her main goal is to “translate” the ever-evolving public health science so that people will be well equipped to make evidence-based decisions. This newsletter is free thanks to the generous support of fellow YLE community members. To support this effort, subscribe below:





Hi YLE - Thank you for the great info as always! Can you shed some light on why other countries have come to different recommendations, as it relates to kids, for the COVID vaccine? Several countries either aren't recommending the vaccine and / or boosters for this age group. There is of course misinformation out there (mainly driven by media), but there are several ethical countries who have landed on a different recommendation for their youth.
As the prior Director of the Office of Pediatric Therapeutics at FDA, and the Office which administered the safety reviews of newly approved products by the Pediatric Advisory Committee of FDA, I would suggest that we NOT be saying we know the LONG-TERM safety profile for myocarditis in adolescent males, nor be reassuring re long term outcomes-we simply do not know nor have the data. At this point we have absolutely no idea what myocarditis, caused by what is probably an autoimmune process, will mean when these young men are in their 30's or 40's or 50's. What we should be saying is, at this point, the risk of the virus causing severe illness in healthy (non-immunocompromised) males of this age group is ------ (low) vs the risk of myocarditis which will result in hospitalization is_____ (lower) ,with a known short term outcome that is encourageing. Though we see no evidence of KNOWN permanent damage in the majority of cases, there is no long term outcome information at this time. ALL confidence will be lost in government agencies if we are not careful in how we define the risk-benefit in this specific population for this immunization. Obviously young males with immunecompromised systems or other conditions that make them more likely to have a severe outcome from a Coronovirus infection should NOT be lumped into this approach as they have a higher risk of a poor outcome if infected. . Population statistics can be misleading when dealing with subpopulations. Thank you for doing such a great job at addressing this evolving epidemic. Dianne Murphy, MD, AAP (retired)