Your votes are in from Monday! We had a tie on your preferred topic for this week’s deep dive between a bird flu (H5N1) update and the implications of RFK Jr. going after ACIP.
Here’s the latest tea on H5N1.
TLDR: The animal outbreak marches on, and you may notice it on your grocery bill. Risk to the general public remains low, but there are a few things you can do. Because of the administration change, there are some shifts in the response. But overall, bird flu isn’t something that should be taking up too much head space right now given (*waves hands around*) everything else.
H5N1 keeps spreading among animals and thus to humans
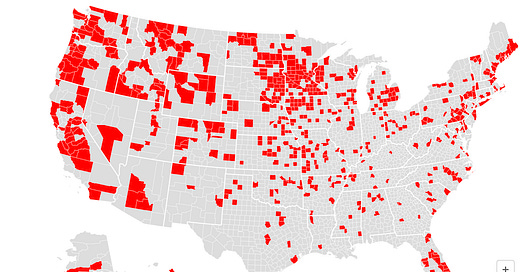
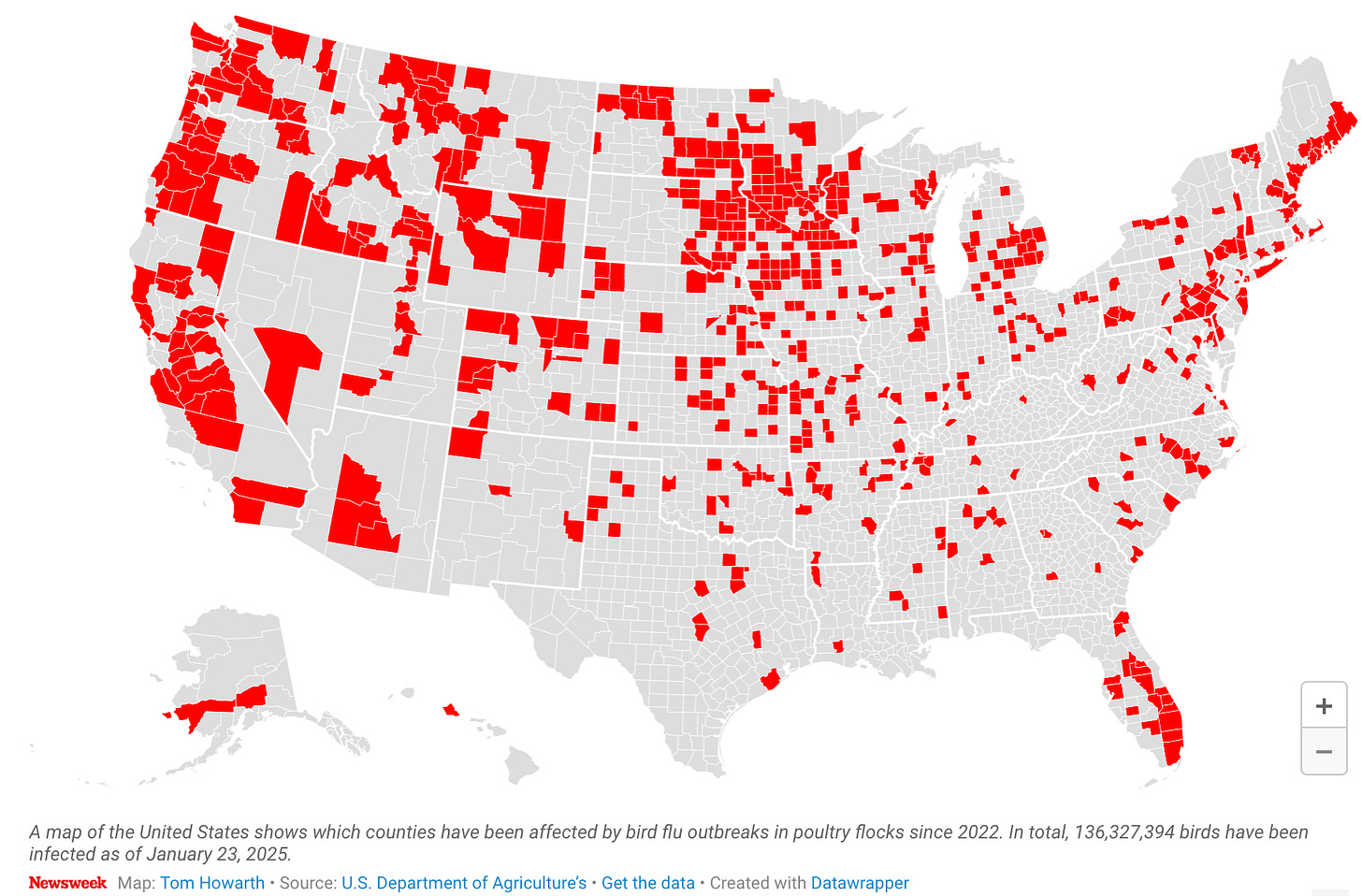
H5N1 hasn’t stopped spreading. It’s in wild birds worldwide and is causing outbreaks in poultry and dairy cows, with quite a few human cases.
Here is the latest animal tally of infections:
12,064 wild birds
973 dairy herds
166,012,718 poultry—a big reason why eggs are hard to find and expensive
Spread among animals, particularly those in close physical proximity to humans, means we continue to see “spillover” infections to humans. In other words, the virus keeps jumping from animal to human, which is bad because every time it jumps, the virus can mutate.
The U.S. human infection tally is:
70 confirmed human infections (+ 7 probable)
Among those, 3 hospitalized
1 person in Louisiana died
People are still mainly getting sick from direct exposure to sick dairy cows (41 people) or sick poultry (24 people). Thankfully, we have not seen human-to-human transmission, and the virus hasn’t mutated to do so yet.
Testing is still limited, and we now know we’re missing cases, especially the milder ones that don’t make people seek care. CDC went to a veterinarian conference and asked bovine (dairy) vets to donate blood to see if they had H5N1 antibodies (and didn’t test positive for H5N1 infection). 3 out of 150 had antibodies; in other words they were infected without knowing it.
Will it burn off? The billion-dollar question
USDA hopes H5N1 (bird flu) will burn off among dairy cows. This is a possibility: the virus could stop finding more animals to infect, eventually hitting dead ends, leading to the disappearance in dairy cows.
However, the probability of this is getting low for two reasons:
Reinfection. Preliminary evidence shows that cows can get reinfected, and if that’s the case, this can keep going in circles around cows.
Multiple entry points. All this started with one wild bird infecting one dairy cow, the virus slightly changing, and then spreading like wildfire. However, evidence shows it wasn’t just a one-off event in Texas. We now have two other documented cases of wild-infected dairy cows in Nevada and Arizona.
This will probably not die off in birds. H5N1 was established in wild birds 25 years ago.
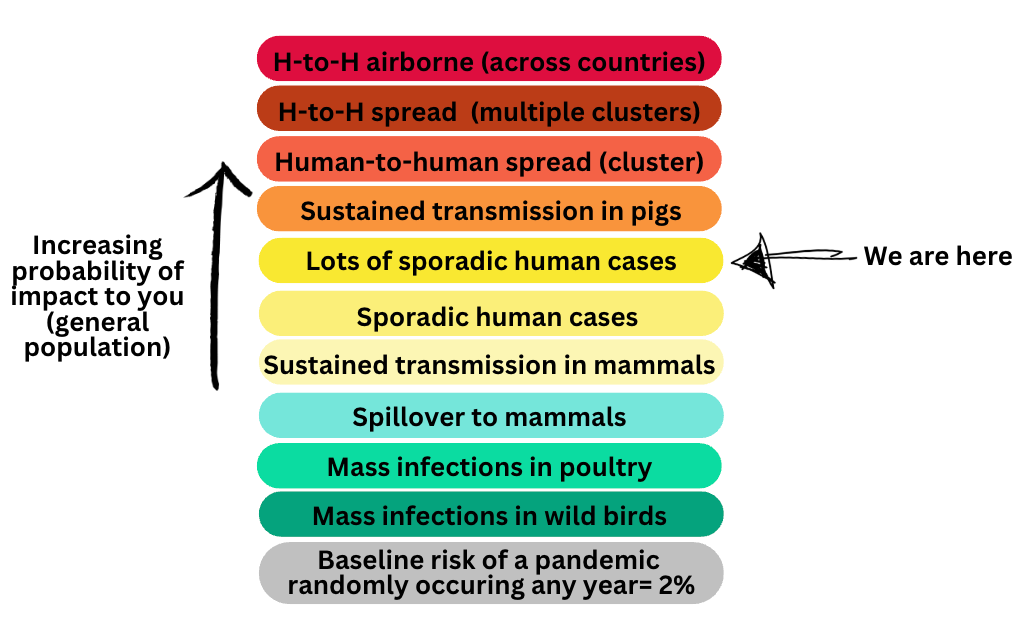
What about pandemic risk?
Any year, there is a ~2% risk of a pandemic because viruses jump from animals to humans all the time. Given the H5N1 developments, the risk has increased a bit. (I wager it’s around 8%.) We could stay at this level forever, it could burn off, or the situation could continue to evolve. Flu rapidly mutates, so there is no way to know. Currently, CDC rates the risk of this ever becoming a pandemic as “medium.”
I mapped the scenarios below for you. The orange and red scenarios below are when my sensors will be going off (and would have the most implications for you).
New administration changes
With any new administration, priorities shift, people are replaced, and tactics can change. Two important developments have unfolded in the past month:
A new sheriff is in town
The Office of Pandemic Preparedness and Response was started in 2023 by Congress and lives within the White House. Its main purpose is to coordinate across government arms. This is needed because each arm of government (like CDC, FDA, and USDA) has its own priorities, legal authorities, conflicts, etc., making a multi-pronged response to, for example, bird flu a mess. This office must remain, by law, but it could be stripped of funds (a loophole essentially making it nonexistent).
Many of us were pleasantly surprised that the new administration maintained this office. Moreover, they tapped Dr. Gerald Parker to head it. He is highly respected in the public health and biosecurity worlds and a great choice. He’s a veterinarian from Texas A&M and has extensive experience in the federal government.
His challenges will be the same as those of the last administration: limited authority (federal arms don’t have to listen to him) and a small budget ($6 million). So how much influence or effectiveness he can/will have is unclear.
A new approach to egg prices? Not really.
Eggs are over $8 per dozen, and Americans feel this in their grocery bills. One big reason is H5N1—it runs like wildfire through poultry farms. In the past 30 days, avian flu wiped out 19 million birds in Ohio, Indiana, Florida, and New York farms. In Ohio alone, there was just a 3 million-bird loss. Bird flu is near 100% fatal for birds and, if it does hit a flock, culling (i.e., mass killing) is the current approach so it doesn’t spread further. This increases egg prices and stresses the supply chain.
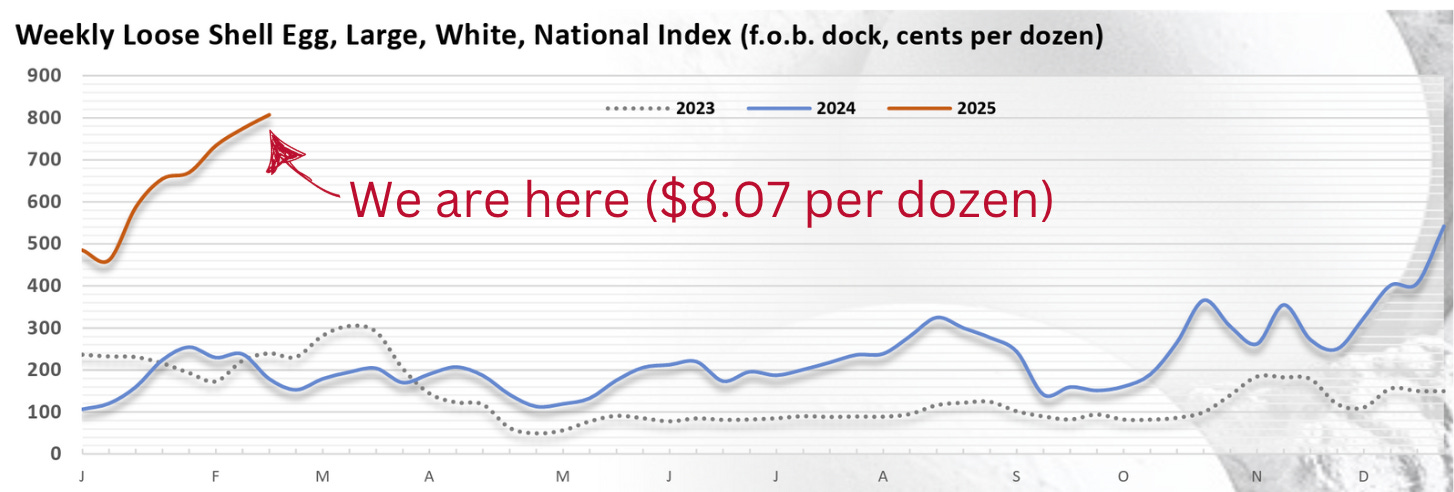
On Wednesday, the administration published its H5N1 5-step plan in response to these egg prices. Honestly, it’s not some big shift like they were making it out to be last week on the news. Briefly, they are putting $1 billion into biosecurity and farmers:
$500 million to help poultry producers implement biosecurity
$400 million in financial relief to farmers whose flocks are affected
$100 million in research and development of vaccines and therapeutics for birds
Remove regulatory burdens on egg producers
Import more eggs
I don’t think there’s much here that would quickly reduce the price of eggs besides imports.
Note that there is nothing here about cattle or risk to humans, which signals they are approaching this primarily as an issue of economic concern rather than health. The new administration is reviewing whether to pull $590 million in funding that Moderna received to develop an mRNA human vaccine for bird flu.
What can/should you be doing?
H5N1 is something to watch, but don’t let it consume too much of your mind. The risk lies with agriculture workers and those who come into contact with sick birds.
For the general public, here are some things to keep in mind:
Backyard flocks:
If you have a backyard flock, you should take precautions to reduce the risk of spreading disease:
Keep your flock contained: isolate your birds from visitors and other birds.
Prevent germs from spreading by cleaning shoes, tools, and equipment.
Reduce the risk of transmission by avoiding sharing tools and equipment with neighbors.
Know the warning signs of infectious bird diseases among the flock, including fatigue, abnormal drop in egg production, swelling or discoloration of the eyelids/comb/wattles/shanks, stumbling or falling down, diarrhea, or unexplained death.
If one of your birds is sick or dies unexpectedly:
Avoid contact with the sick or dead bird. Assume other birds in the flock and their enclosures, droppings, feeders, and water sources are also infectious. (If you can’t avoid contact completely, take steps to protect yourself.)
If possible, isolate the bird from other animals and pets. (Don’t let your dog near it.)
Immediately report sick or dead birds to your state veterinarian or the U.S. Department of Agriculture (1-866-536-7593).
Bird feeders: Birds that gather at feeders (like cardinals, sparrows, and bluebirds) do not typically carry H5N1. The USDA does not recommend removing backyard bird feeders for H5N1 prevention unless you also care for poultry. The less contact between wild birds and poultry (by removing sources of food, water, and shelter), the better.
Raw milk can potentially cause severe disease, but there have been no human cases yet. (Lots of cats have died this way, though.) It also comes with other typical risks, like bacteria.
Hunters are at high risk for H5N1, especially if they don’t use PPE while handling dead birds. A Washington study showed that 2% (4/194) of hunting dogs tested positive for H5N1.
Domestic animals—cats and dogs—can get H5N1 if they contact (usually eat) a dead or sick bird or even its droppings. H5N1 can survive in bird droppings for up to 18 hours. Domestic animals can also get it from raw food, unpasturized milk, and their humans. It’s very deadly to cats (it doesn’t seem to be as much to dogs).
Bottom line
The H5N1 outbreak marches on, and you may notice it on your grocery bill. There are a few things you can do. If the risk changes (which it can quickly), I will let you know. But overall, this isn’t something that should be taking up too much headspace yet.
Love, YLE
Your Local Epidemiologist (YLE) is founded and operated by Dr. Katelyn Jetelina, MPH PhD—an epidemiologist, wife, and mom of two little girls. Dr. Jetelina is also a senior scientific consultant to a number of non-profit organizations. YLE reaches over 340,000 people in over 132 countries with one goal: “Translate” the ever-evolving public health science so that people will be well-equipped to make evidence-based decisions. This newsletter is free to everyone, thanks to the generous support of fellow YLE community members. To support the effort, subscribe or upgrade below:




Excellent summary and analysis.
What do you make of the decision to cancel the annual flu vaccine panel?