Tomorrow a much anticipated 3rd shot discussion will occur at the FDA centered around one question: Does the general population need a 3rd mRNA dose? This should be a fascinating, scientifically driven, heated debate. I have no idea how it’s going to end. I will be in attendance and, of course, provide you with some cliff notes.
In the meantime, another important question has risen to the surface: Do Pfizer and Moderna people need a 3rd dose? Or just Pfizer people? In other words, is there a meaningful difference between Moderna’s and Pfizer’s protection against COVID19?
Subtle Differences
Throughout the pandemic, I’ve always lumped Moderna and Pfizer together. For example, if there was evidence that Pfizer worked against a variant, then Moderna surely worked too. The two mRNA vaccines are incredibly similar, but they’re not identical. There are a few subtle differences between the two:
The formulation: The fat bubbles that carry the mRNA are a bit different. In the Figure below, you can see that A (Pfizer) has a slightly different pattern than B (Moderna);
The dose of RNA is different: Moderna has a much higher dose (100 mcg) compared to Pfizer (30 mcg);
Different vaccine schedule: Moderna doses are 4 weeks apart, while Pfizer doses are 3 weeks apart;
Pfizer was approved in the United States (and around the world) a few weeks (or months) prior to Moderna.
At first, these small differences didn’t impact vaccine effectiveness. Both were extremely great at protecting against asymptomatic, mild, moderate, and severe disease.
But the story might be changing
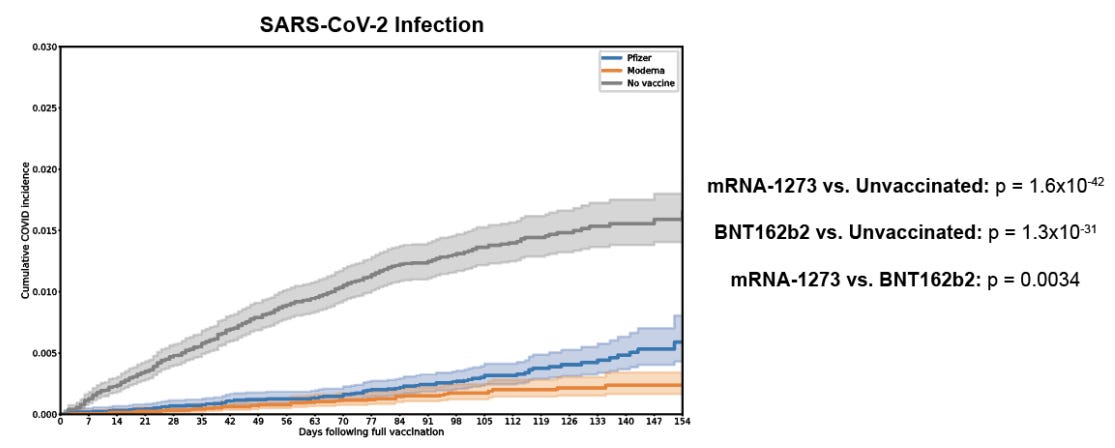
Last month, the Mayo Clinic released a preprint of a very large study of 645,109 patients followed after vaccination (January - July 2021). The scientists wanted to describe breakthrough rates among vaccinated with Moderna, vaccinated with Pfizer, and unvaccinated. How were the vaccines holding up?
Both vaccines continued to work great against hospitalization, ICU admission, and death (there were no deaths in the study). This was the case in January 2021 and this was the case in July 2021. This didn’t changed.
Effectiveness against any infection (so mild to moderate disease), though, was lower for both vaccines in July (76% effectiveness) compared to January (86% effectiveness)
Interestingly, Pfizer’s effectiveness decreased faster over time (i.e. more breakthrough cases) compared to patients vaccinated with the Moderna vaccine (i.e. less breakthrough cases).
Nonetheless, both vaccines were much better at preventing infections compared to no vaccine (unvaccinated patients).
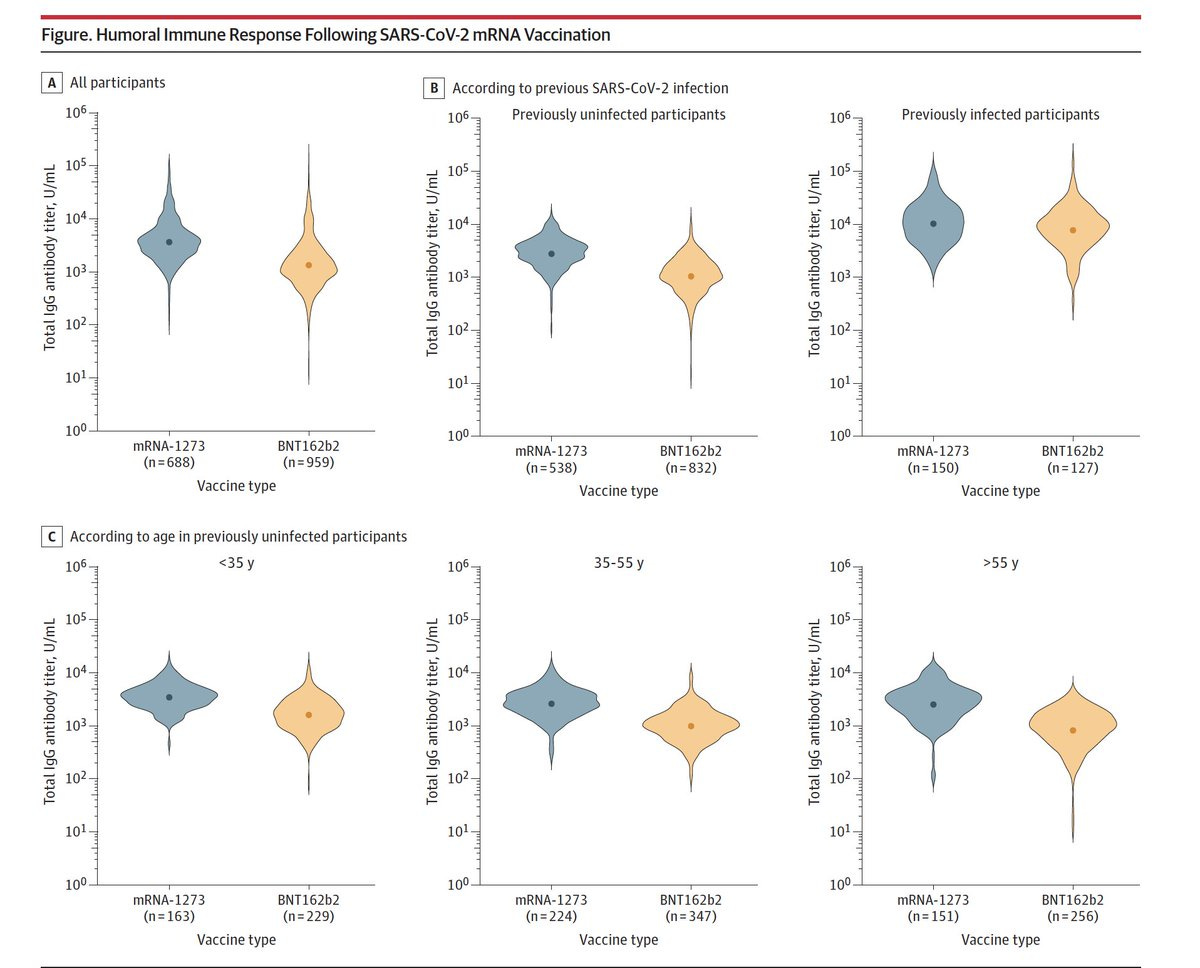
We saw this in another study too, which tested 196 elder nursing home residents in Canada after vaccination. Interestingly, residents’ with Pfizer mounted a 3.89-fold fewer neutralizing antibodies than residents’ with Moderna. We can visually see this in the Figure below. Moderna is on the left (blue) and Pfizer is on the right (yellow). The black dots in the blue are significantly higher than the black dots in the yellow. This was most apparent with the Beta variant (first discovered in South Africa; also called B.1.351).
On August 30, a Belgium study was published in JAMA. The scientists looked at antibody levels against the spike protein in 1,647 workers at a Belgium hospital. Levels among those who got two doses of the Moderna vaccine averaged 2,881 units per milliliter, compared with 1,108 units per milliliter among those who received two Pfizer doses. The immune response was even greater for vaccinated people who had been previously infected. So the number of antibodies were higher, but as you may know, those numbers aren’t really meaningful. We don’t know what antibody number you need to say “you’re protected”.
And, finally, a Qatar study largely found the same thing.
So, is there really a difference?
Maybe. But we don’t know why yet. This could be due to…
…higher dosage of RNA in Moderna compared to Pfizer. The higher the dosage may possibly explain the longevity of the response (or strength against Delta).
…the 4 weeks between doses in Moderna compared to the 3 weeks in Pfizer. The more time between doses, the stronger the response. We’ve seen this time and time again (and may explain why we need a 3rd dose).
…timing. Moderna was offered later than Pfizer. That time difference, on a population-level, may be influencing this difference. In other words, Moderna may start decreasing too, it just hasn’t had the time to like Pfizer has.
…Or this could be nothing. The aforementioned studies had limitations (like all studies do), which may bias the conclusions. We need more studies showing the same thing among different populations to be more confident. We also need to figure out the “why”.
Most importantly, though, both vaccines continue to work amazingly against hospitalization and death. And this, ladies and gentleman, is causing the heated scientific debate among scientists. We cannot possibly stop all breakthrough infections; we will be boostering forever. If both vaccines are working against hospitalizations and deaths, does it make sense to get a 3rd dose? What is our end game?
Be back tomorrow with some cliff notes!
Love, YLE







My husband is immunocompromised. He had no detectable antibodies after 2 doses of Moderna. He had a booster, but we aren’t confident it helped him much. A breakthrough infection for me could be fatal for him.
I have several autoimmune illnesses, and have had post-viral illnesses that last months to years. Already have POTS as a result of Ehlers Danlos Syndrome. Long Covid is a real possibility for me. Yes, we mask, everywhere, with n95s. Still, give me that shot. I will take it as soon as it becomes available.
It seems we'd be so much better off with a third dose because we know for a fact that the first two were way too close together to be optimal. So we could just stop with 3. OTOH, what's wrong with a yearly shot? We do it for the flu.