We’ve been using the same vaccine formula throughout the pandemic—one created in early 2020 to fight against the original Wuhan variant. But the virus continues to mutate quickly. This means our antibodies are waning fast and (re)infections are coming more often. Marry this with the fact that coronaviruses thrive in the winter, and we likely need an updated strategy going into the fall.
So what’s our next move?
A hard problem to solve
One way to get ahead of the virus is to anticipate the dominant variant this winter, just like we do with the flu each year.
For flu, scientists meet annually to evaluate new circulating strains and determine if an updated vaccine formula is needed. Each year, the WHO makes recommendations in February for the upcoming Northern Hemisphere influenza season. Then it takes about 5-6 months for the vaccine to be available. This isn’t a perfect process, but on average we have 60% vaccine effectiveness each year.
It’s suggested that we adapt this process for COVID-19. And I agree. But I can’t highlight enough how incredibly challenging this is right now. For several reasons:
SARS-CoV-2 is changing 4 times faster than the flu due to high transmission. New variants can emerge and dominate after the vaccine process has begun. This happened famously before the 2009 and 2014 flu season. It could certainly happen with COVID19. This time last year Alpha was dominant. By winter, we went through two new variants of concern.
We have no idea how this virus will mutate. We haven’t had enough time to see ladder-like patterns, like we see with flu. We think Omicron will continue to mutate—there’s a 70% chance we will not have another Omicron-like event—but this is just an educated guess.
For flu, there is just one main vaccine platform (egg-based). With COVID-19 we have a few. Timelines, processes, manufacturers’ experience, and facility capacity vary for each.
Because of the predictive power and manufacturing experience with flu vaccine, no new clinical data is required by the FDA each year. With COVID19, though, the FDA requires vaccine-specific safety profiles and effectiveness data.
The FDA met in April to discuss this very subject. More challenges were discussed than solutions. But reading between the lines, it was clear that if we get another fall vaccine, it would need to achieve three things:
Improve durability. We need something that lasts at least 6 months to get us through a winter wave.
Retain protection against previous variants of concern. With infection-induced immunity, Omicron does NOT protect well against previous variants of concern. We need to make sure our vaccines do in case a previous variant, like Delta or Beta, take hold again.
Protect against future, unknown variants of concern.
Moderna’s answer
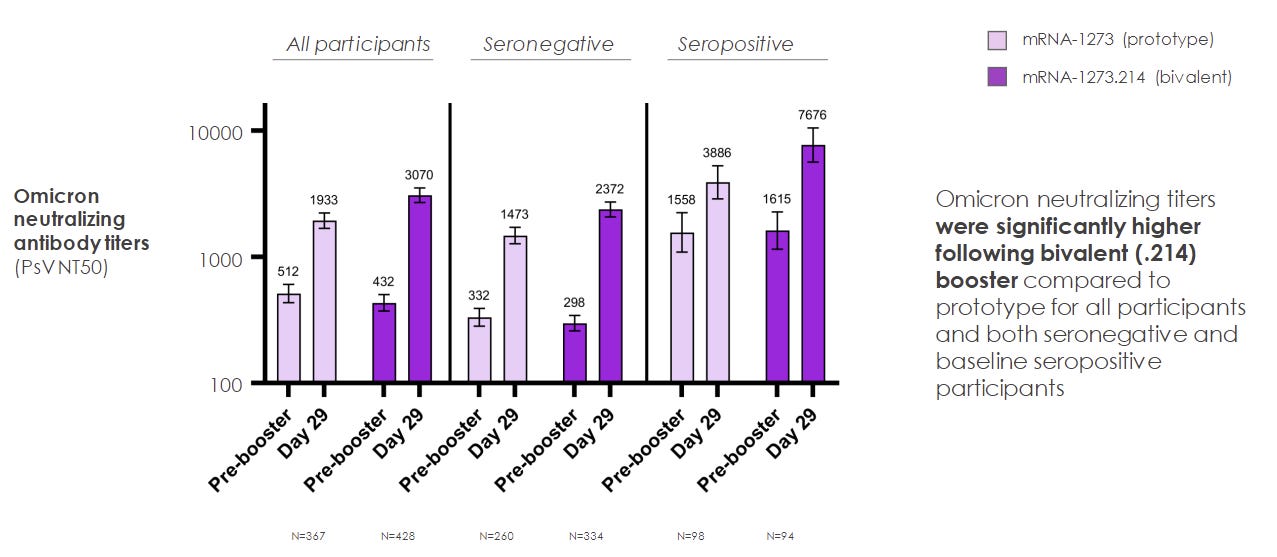
Yesterday, Moderna’s results were released for a booster called mRNA1273.214. This vaccine is 50 micrograms, which is the same dosage as the original booster and half the dosage of the original Moderna series. They tested a bivalent vaccine, which means its formula covers two variants: the original Wuhan virus and Omicron (BA.1). For this clinical trial, 437 people were randomized to get the new vaccine or old vaccine as a second booster. We have a few details (science by press release) on how this trial went:
Side effects were similar to the original booster. The new booster may actually have slightly reduced side effects.
There was an 8-fold increase in neutralizing antibodies (our first line of defense) one month after vaccination.
This was higher than the original booster.
There was a stronger effect among those with previous infection.
The new booster had better protection against all other variants of concern, compared to the original.
We don’t know about durability; we are at the mercy of time. But Moderna said their bivalent Beta-vaccine lasted against Omicron for 6-months+. This probably means the Omicron bivalent vaccine will last just as long.
Unanswered, lingering questions
In all, the new vaccine seems to work great, but we need to see more data than a press release. Pfizer should have a bivalent vaccine coming soon, too. On June 28, the FDA will discuss the new results and overall U.S. strategy for fall. There are some lingering and unanswered questions that I hope are addressed during this meeting:
Booster or series? Moderna’s intent is to treat this as a one-shot seasonal vaccine. However, at the last FDA meeting, it was said that if the vaccine formula changed, it would have to be a whole new series. We need clarification.
Omicron has mutated. This vaccine is made with the first Omicron variant (BA.1). Now we have a BA.4/5 wave in the horizon, which is significantly and meaningfully different from BA.1. How well does the new vaccine work against BA.4/5?
More data. We need to make sure these vaccines also improve secondary defenses like B-cells and T-cells. We’ve seen evidence from monkeys that an Omicron-specific vaccine does not expand the memory of B-cells.
Beta vaccine? Moderna previously released data for a Beta-bivalent vaccine. A side-to-side comparison would be helpful. According to Dr. John Beigal at the NIH, there are really only two antigenic spaces or areas of vulnerability that would allow for another “Omicron-like event”: a virus that is closer to Beta, or a virus that is closer to Delta. Both are very far from Omicron, which perhaps makes an Omicron-specific booster not a slam dunk decision.
Kids. Unless FDA changes the way they evaluate vaccines, kids will never have access to up-to-date boosters. We can’t continue with a process that leaves kids constantly two years behind.
Bigger questions (beyond the FDA) include:
Payment. Congress has not passed COVID19 funding, so we don’t have money to pay for everyone’s new boosters in the U.S. Not everyone would get in line given vaccine hesitancy, but the discrepancy and the implications are important.
Vaccination rate. All of this science is great. But only 48% of people in the U.S. have their original booster. Only 23% of eligible people have their second booster. Why aren’t we leveraging social science as much as bench science to increase effectiveness of vaccine rollouts?
Bottom line
Predicting what happens this fall is challenging. We are trying our darndest to mount a proactive (instead of reactive) response. Given Moderna’s preliminary data, I would expect a bivalent vaccine in fall. Will we have a booster every fall? No idea. It completely depends on how this pandemic progresses.
Love, YLE
Your Local Epidemiologist (YLE)” is written by Dr. Katelyn Jetelina, MPH PhD—an epidemiologist, biostatistician, wife, and mom of two little girls. During the day she works at a nonpartisan health policy think tank and at night she writes this independent newsletter. Her main goal is to “translate” the ever-evolving public health science so that people will be well equipped to make evidence-based decisions. This newsletter is free thanks to the generous support of fellow YLE community members.




ER physician here. We are seeing trickles of COVID and a lot of Influenza-A right now. I’ve never seen Flu this late in the season; never in June. Some Flu cases vaccinated, some not. Why is this? My apology if you addressed this already in prior post. Mark/Tucson, AZ
Thanks as always for your clear, data-based postings.
As a social scientist, I will note that Brandolini's Law has been in play since the beginning of the epidemic (and actually, in a wide variety of science-denying efforts for decades, going back to debates about the health implications of cigarette smoking and beyond).
I think scientists still often tend to shrug their shoulders when confronted with obvious woo and dis/misinformation. It is difficult and painful, and frequently futile to try to counteract people's irrational beliefs. It often takes a life-changing experience for someone to change their mind, especially if they have publicly espoused a contra-factual position. Many people will literally die rather than change.
That said, I think there are a lot of good attempts (including yours) to provide accurate information. The problem is that science-based communications are trying to use logic, facts and rational thinking to counter emotional, "magical" disinformation. Critical thinking is a learned skill, that requires effort and the ability to admit you are wrong and that someone else might be right. It is hard work, and many people were not taught the necessary skills and are too tired/overworked/bombarded by deceptive messaging about everything in their life to have the strength of will to learn to be critical and apply the skill regularly.