We are seeing a tsunami of respiratory illnesses and, in its wake, severe disease and overcrowded hospitals. This is mainly driven by RSV, with flu picking up steam. COVID-19 infections have yet to start rising, but we still expect these to uptick soon.
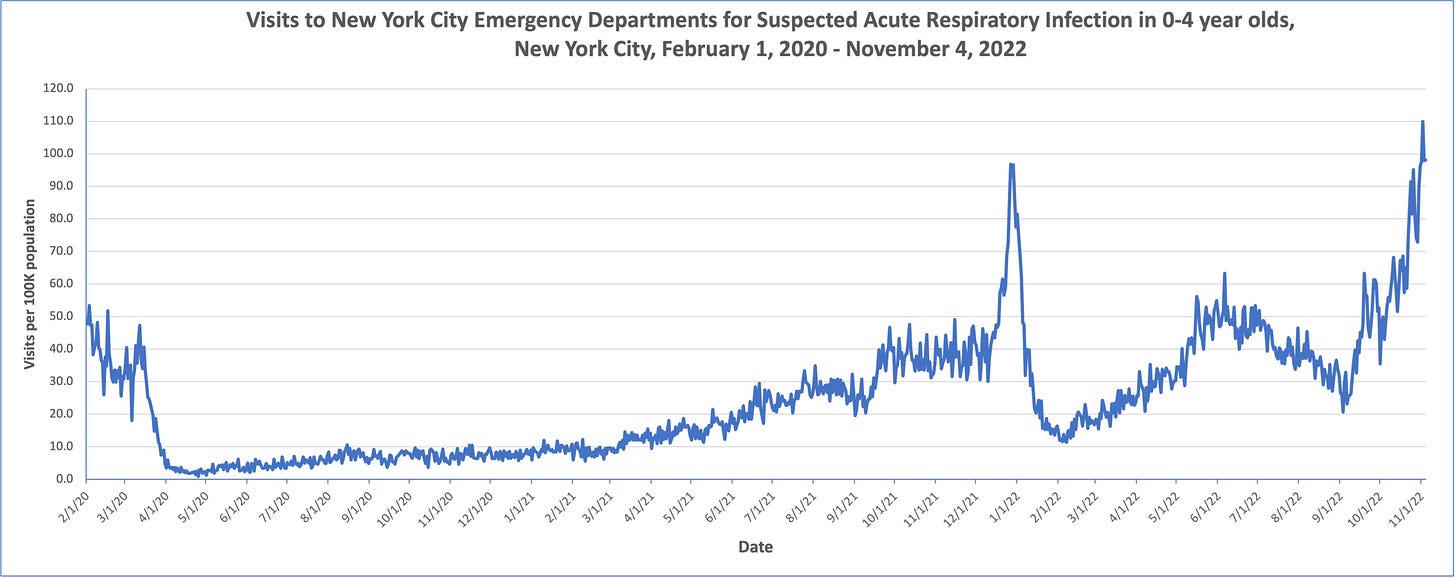
Children are getting hit particularly hard. Emergency department visits for 0 to 4 year-olds, for example, are the highest they’ve been throughout the pandemic—including the first Omicron wave last winter—with numbers continuing to rise.
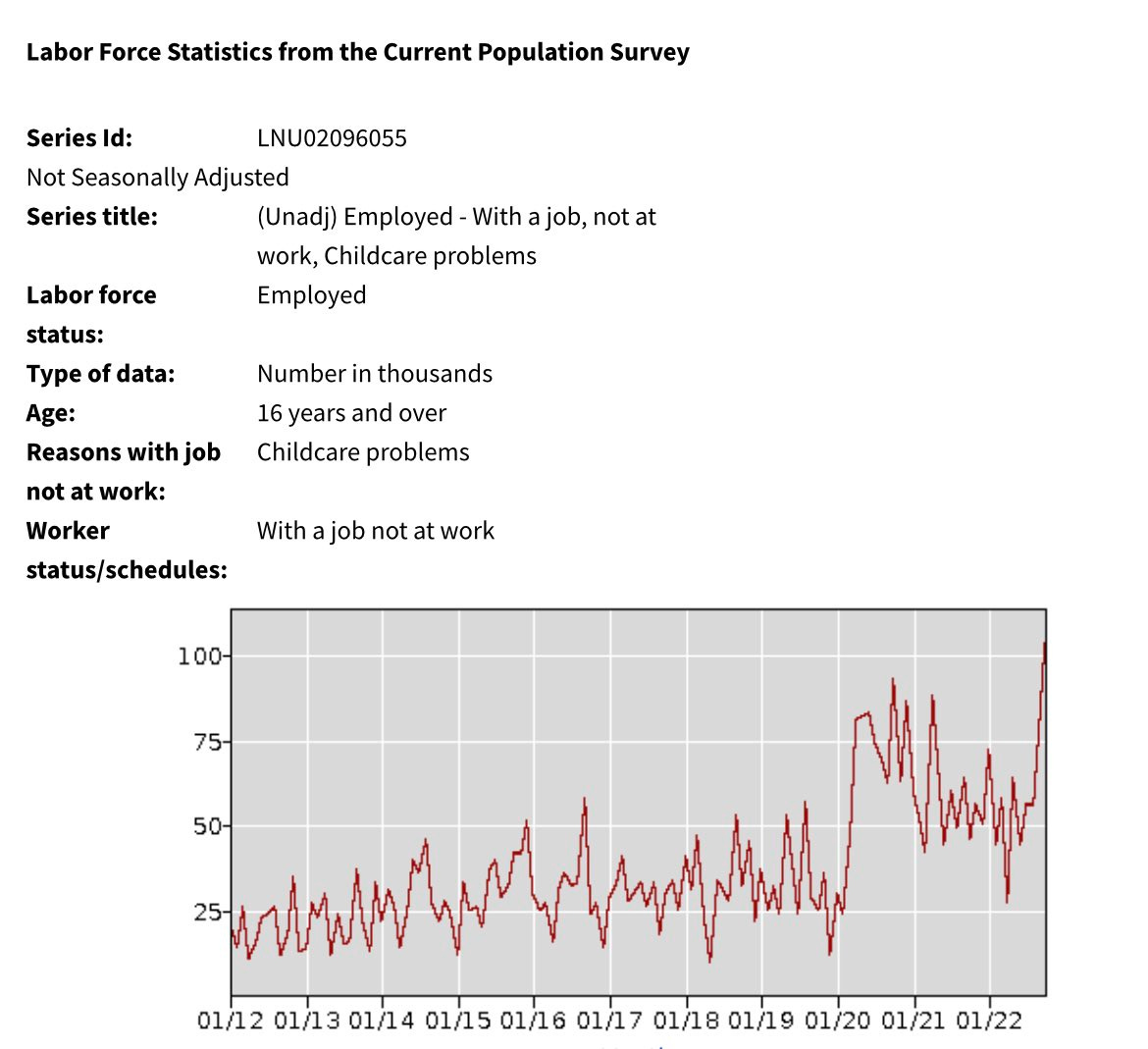
This, of course, is impacting parents across the country. The latest Department of Labor data found absences from work due to childcare problems hit a record high last month—higher than during the past two years of the pandemic. If you’re home with a sick kid right now, you’re not alone.
With a wave of RSV infections comes a wave of questions. Here is what we do (and do not) know about RSV.
What is RSV?
RSV stands for respiratory syncytial virus. It’s an RNA virus, so it mutates quickly.
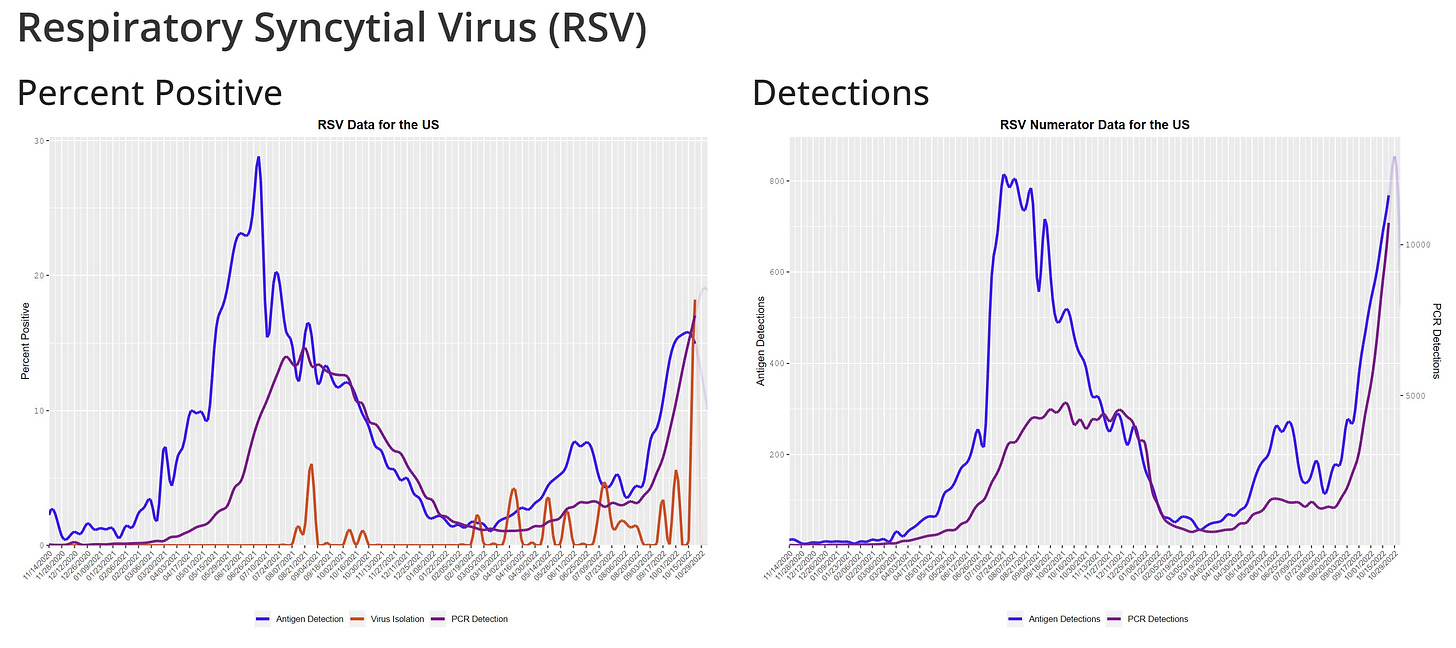
Historically, RSV hit during the winter. However, the pandemic really threw off viral dynamics. During the first two years of the pandemic, RSV increased during the summer months although at lower than typical rates. It appears RSV is back on track, although it is earlier compared to pre-pandemic years.

On average, one infected person will infect three other people (R0=3; which is far less contagious than COVID-19 but more contagious than flu). People are typically infected 4 to 6 days after exposure and are usually contagious for about a week. People can be contagious a day or two before they start showing signs.
RSV infects cells within our airways. After entering our cells, our immune system sends fighter cells, which cause inflammation and thus symptoms. We have two main airways that can be infected:
Upper airway, where infection causes cold-like symptoms, like a runny nose.
Lower airway (like lungs), where infection causes difficulty breathing.
How is RSV transmitted?
There are really two main transmission routes:
Respiratory droplets: droplets from coughs and sneezes that contain the virus, but can fall to the ground after a couple feet of travel.
Fomites: viral particles that can survive many hours on hard surfaces such as crib rails and toys.
With the pandemic, we (scientists, parents, everyone) can’t help but think that aerosols (droplets that stay in the air) are also a main driver. More research is needed, as the latest data was from the 1980s. There is also quite a bit of debate regarding the main mode of transmission.
Who is at risk?
Anyone can be infected with RSV, and it is very common. In fact, 1 in 4 adults will be infected each year. By the age of 32 months, 100% of children have antibodies. This means that without a vaccine, it’s very likely that your child will get RSV in the first few years of life.
The majority of people have mild symptoms that typically mimic a common cold. Some people (but not all) get a fever.
RSV can cause severe disease, though, mainly among two groups:
Young children. 5 out of 1000 children under 5 years of age will be hospitalized. This is a higher rate than for flu or COVID-19. The younger the child, the more likely hospitalization is. This is because their airways are just so tiny and can’t let air flow through when inflamed. When a child is hospitalized, the average hospitalization stay is 5 days and ~7% require ICU admission. Among those hospitalized, most children were previously healthy. Before the pandemic, RSV killed 100 to 500 U.S. children under age 5 each year.
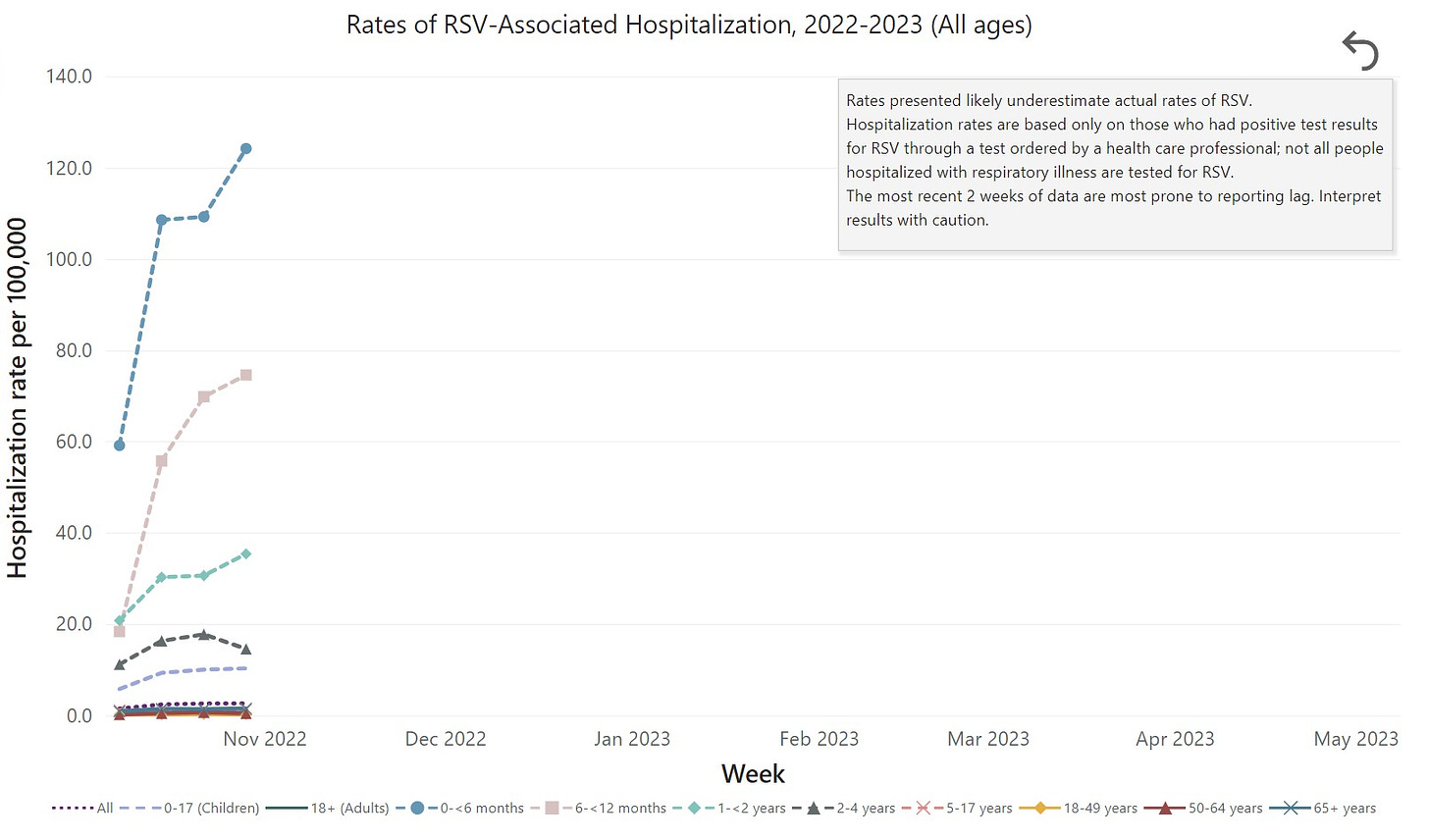
(Source: CDC RSV-NET) Older adults. Each year, between 60,000 to 120,000 older adults in the United States are hospitalized, and 6,000 to 10,000 of them die due to RSV infection. Just like COVID-19, RSV is rough on older adults because their immune systems are weaker and they are more likely to have underlying health conditions, like heart or lung disease.
Is there an RSV test?
Yes, there are PCR and antigen tests for RSV. (Antigen tests work best on kids compared to adults.) But the tests require a laboratory to process results.
There is one at home test that can differentiate between flu, RSV, and COVID19. But, you need to mail it to a lab for results.
Is there treatment?
There is no medication specifically to combat RSV. The only treatment is to help alleviate symptoms (for example, using oxygen in the hospital).
We are working on antivirals, but just like with COVID-19, they are very difficult to make. There is a drug called nirsevimab made by AstraZeneca, though, that had very promising Phase III clinical trial results for infants. The FDA may approve this soon.
We do have monoclonal antibodies, called Synagis. This is not a vaccine, but an injection given once a month throughout RSV season. By proactively injecting antibodies, the risk of serious lung infections decreases. This medication is super expensive and in limited supply, so it’s saved for people with the highest risk.
How long is someone protected after infection?
Unfortunately, not long. RSV is fantastic at evading immunity. This means children and adults can get RSV multiple times, even during a single season.
One fantastic study found that when scientists followed kids over time, the severity of infection didn’t decline until the children had RSV at least three times. After initial exposures, though, repeat infections are less severe in adulthood (before older age).
Why don’t we have a vaccine?
Two reasons:
We had a vaccine trial back in the 1960s that was a disaster. Kids who got vaccinated were at higher risk for severe disease than those who didn’t. Two kids died. Scientists have since figured out the problem (called antibody-dependent enhancement).
The virus’s key into our cells has been historically tricky to target with a vaccine.
But there is good news. In 2013, there was a scientific breakthrough and we figured out how to create an effective and safe vaccine. This past month, we got results from Pfizer’s clinical trials of a bivalent (targets two variants) protein-based (not mRNA) RSV vaccine tested pregnant women. The vaccine was safe and effectively made antibodies that moved across the placenta. Pfizer found high efficacy against severe disease in infants from birth through the first 90 days (81.8%) and 6 months (69.4%) of life. Pfizer plans to submit for FDA approval by end of the year. If approved, this will be the first RSV vaccine, and it will be a game changer.
We also got great news about a RSV vaccine for older adults from two manufacturers (GSK and Pfizer): 82% efficacy rate for GSK and 86% for Pfizer.
Immune debt?
These two words have been floating around parent groups causing a ton of emotional debates on the heels of the pandemic. To be clear, “immune debt” has no official definition and means many things to many people. Here is my epidemiological perspective.
The pandemic delayed first infections of common viruses, like RSV, due to shut downs, social distancing, masking, etc. We saved thousands of lives doing this until we could get a COVID-19 vaccine. This was the right call. However, that phenomenon pushed a larger population-level effect of the common viruses that we are seeing now. We always expected a resurgence. This resurgence is NOT caused by the COVID-19 vaccine itself (as some disinformation is insinuating).
But there are things we don’t know yet. Could previous COVID-19 infections impact children’s immune systems? Maybe, but we don’t have evidence on this either way. This needs to be carefully studied.
Bottom line
The situation right now isn’t great for kids or older adults. It’s not great for hospitals. It’s not great for caregivers. You can help people around you. Do the same things you do with COVID-19—stay home while sick and mask in public. Wash hands and toys—this will help with RSV. Also, don’t let people kiss your baby.
This RSV surge reinforces the need to reduce the burden of common viruses, too, which take an enormous toll on our society.
Love, YLE
“Your Local Epidemiologist (YLE)” is written by Dr. Katelyn Jetelina, MPH PhD—an epidemiologist, data scientist, wife, and mom of two little girls. During the day she works at a nonpartisan health policy think tank, and at night she writes this newsletter. Her main goal is to “translate” the ever-evolving public health science so that people will be well equipped to make evidence-based decisions. This newsletter is free thanks to the generous support of fellow YLE community members. To support this effort, subscribe below:



I work at a very small pediatric office in Alaska. This past week we have been inundated with sick kids, most all of them testing positive for RSV. I want to know if RSV is transmitted on surfaces. When Covid first started and no one was giving us correct information about how it spreads (even though they knew)there was a lot of hints that it spread on surfaces and we were wiping down everything. In the beginning we would see one family at a time and when they left I would wipe down and sanitize every surface I could. When it became clear that it was transmitted mostly through the air all that cleaning mostly went away. I’m wondering if I should start sanitizing everything again to prevent the spread of RSV in our office. I’m so overwhelmed with regular work, Covid vaccine stuff, and phone calls about sick kids, but I am more worried than ever about someone getting sick just coming into our office. it should be a safe place not a place where you get sick when you come in for a routine check up or something else not related to a respiratory virus. I am not a nurse or a trained professional, but I’ve been working for my boss for 14 years and have a lot of on the job experience.
I feel isolated most of the time as I really haven’t changed my routine since the pandemic started. I still wear a mask everywhere (even though most people don’t anymore). I don’t go to the movie theater, bars. or restaurants. I really only have one contact that I do not wear a mask around. I really want to connect with people like me if there are any to share experiences and gain knowledge.  Any help or advice would be very appreciated. 
Excellent article, thank you. There is often a significant toll taken on adults with RSV, too. One example from my practice - a single Mom with two kids feeling very sick with RSV, one of whom is in the hospital right now. She also feels quite ill, with flu-like cough, body aches, and fever.
On the Covid front, I'm sure you saw the VA study this week about Paxlovid helping to reduce Long Covid. Dr. Topol had a great run down, and I did my best from a primary care perspective:
https://mccormickmd.substack.com/p/to-paxlovid-or-not-to-paxlovid
Drop us your thoughts when you have a moment sometime, as your advocacy for the antiviral swiss cheese layer has been very helpful this whole time!