The start of the school year is here. To us parents, this signals the start of runny noses, fevers, tired kiddos, and lots of Bluey.
Here is your state of affairs and things we can do to prevent disruptions this fall.
Going into the school year
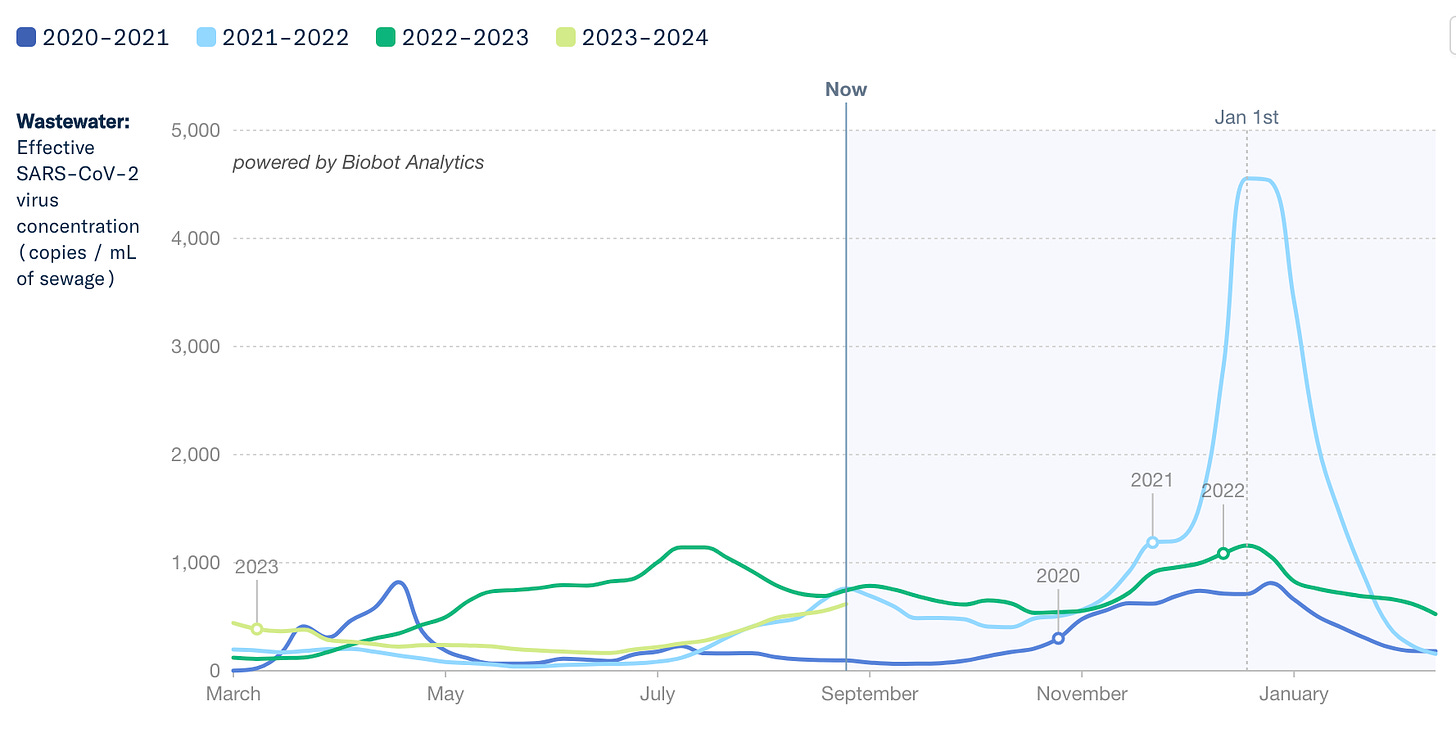
We are in the middle of a Covid-19 wave. This isn’t necessarily because school started, but rather was jumpstarted in summer due to behavior change (hot weather —> moving inside), a mutating virus, and waning protection.
Currently, wastewater levels are on par with what we saw this time last year.
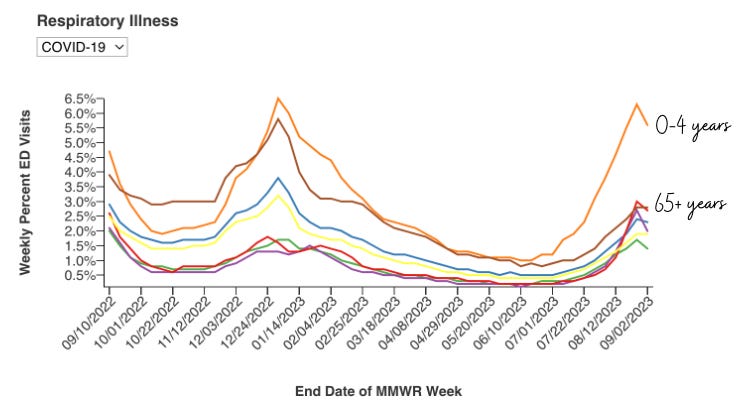
As expected, ED visits are following infections. Covid-19 still accounts for the highest percentage of ED visits for those under 1 year old.
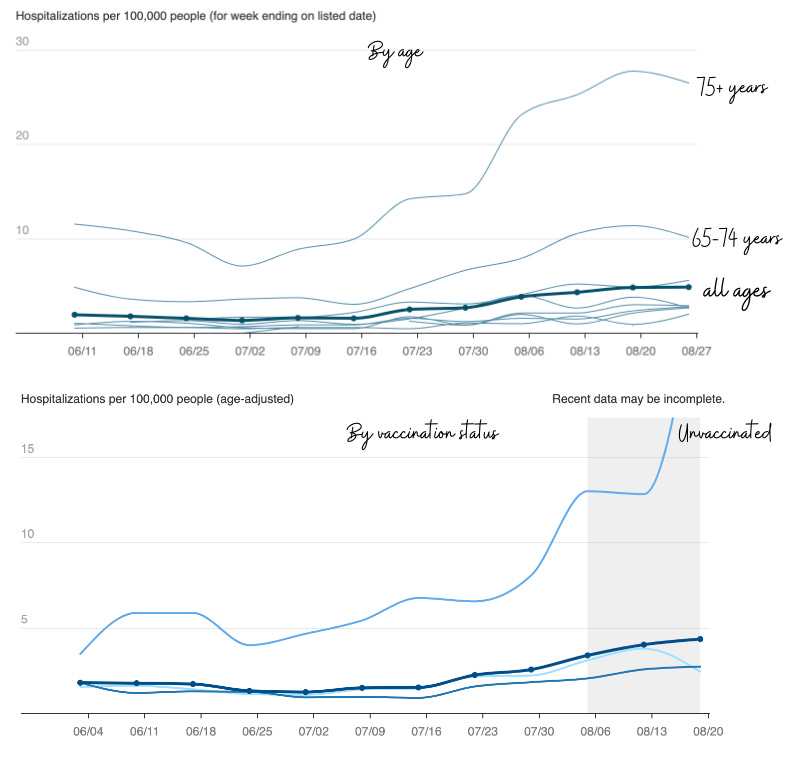
Hospitalizations lag ED visits but remain high among older adults and unvaccinated people (who presumably had a prior infection at this point).
Start of school
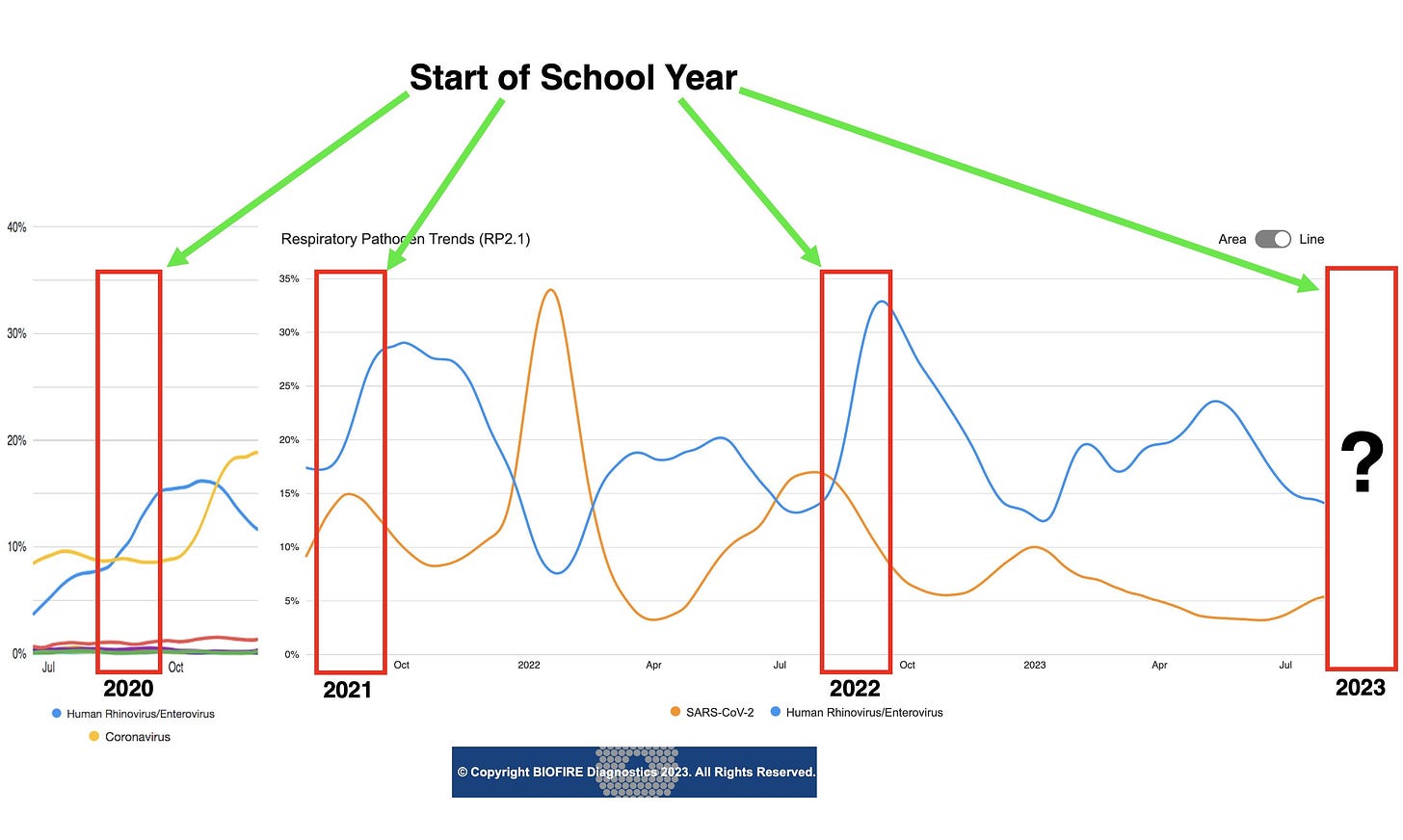
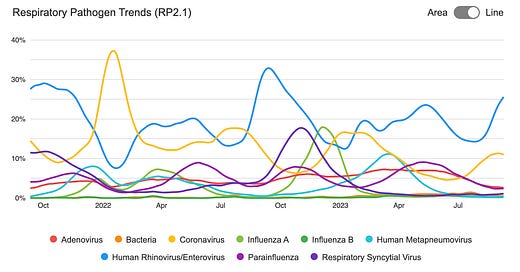
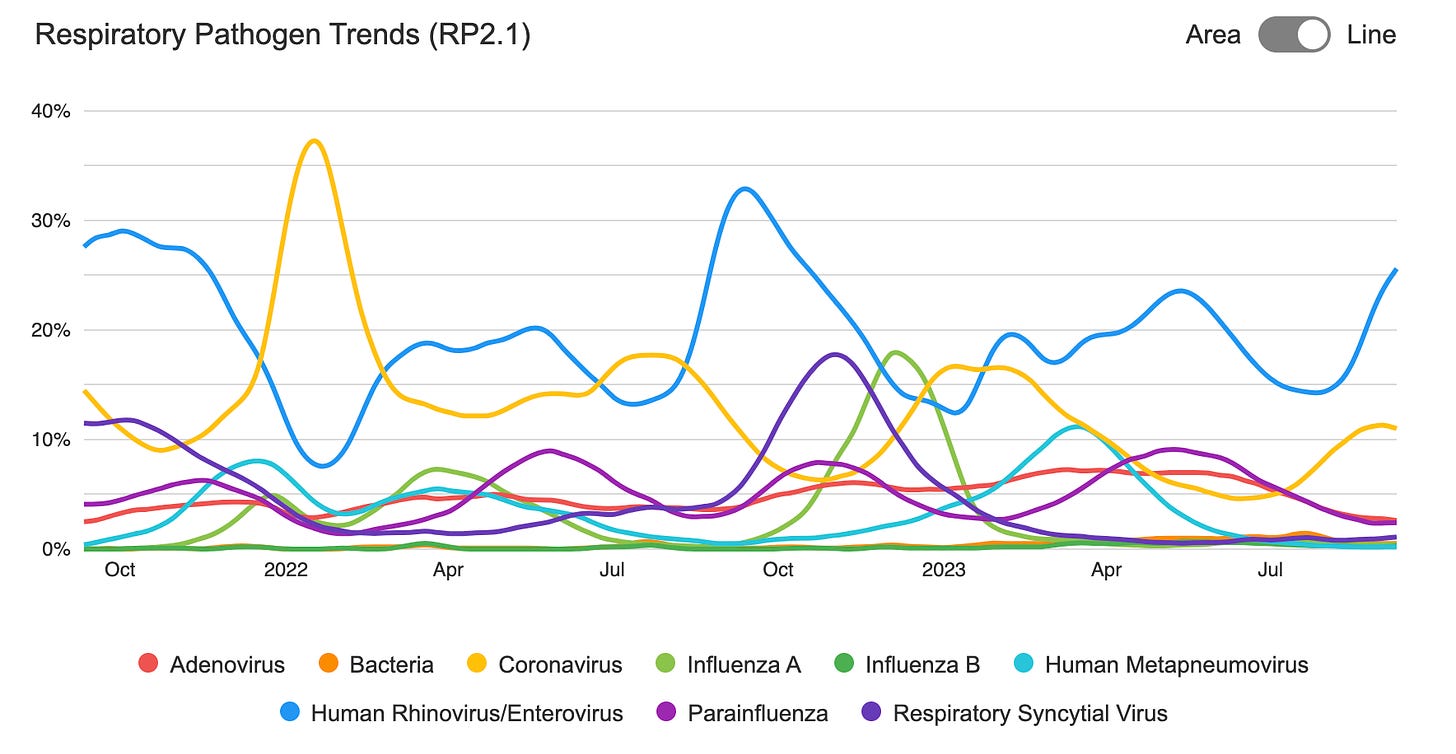
As school starts, rhinovirus (common cold) and enterovirus (including hand, foot, and mouth disease) increase. This year is no different, with quickly increasing rates of illness.
Interestingly, an increase in rhinovirus/enterovirus has coincided with a decrease in COVID-19 infections throughout the pandemic. Time will tell if this trend continues.
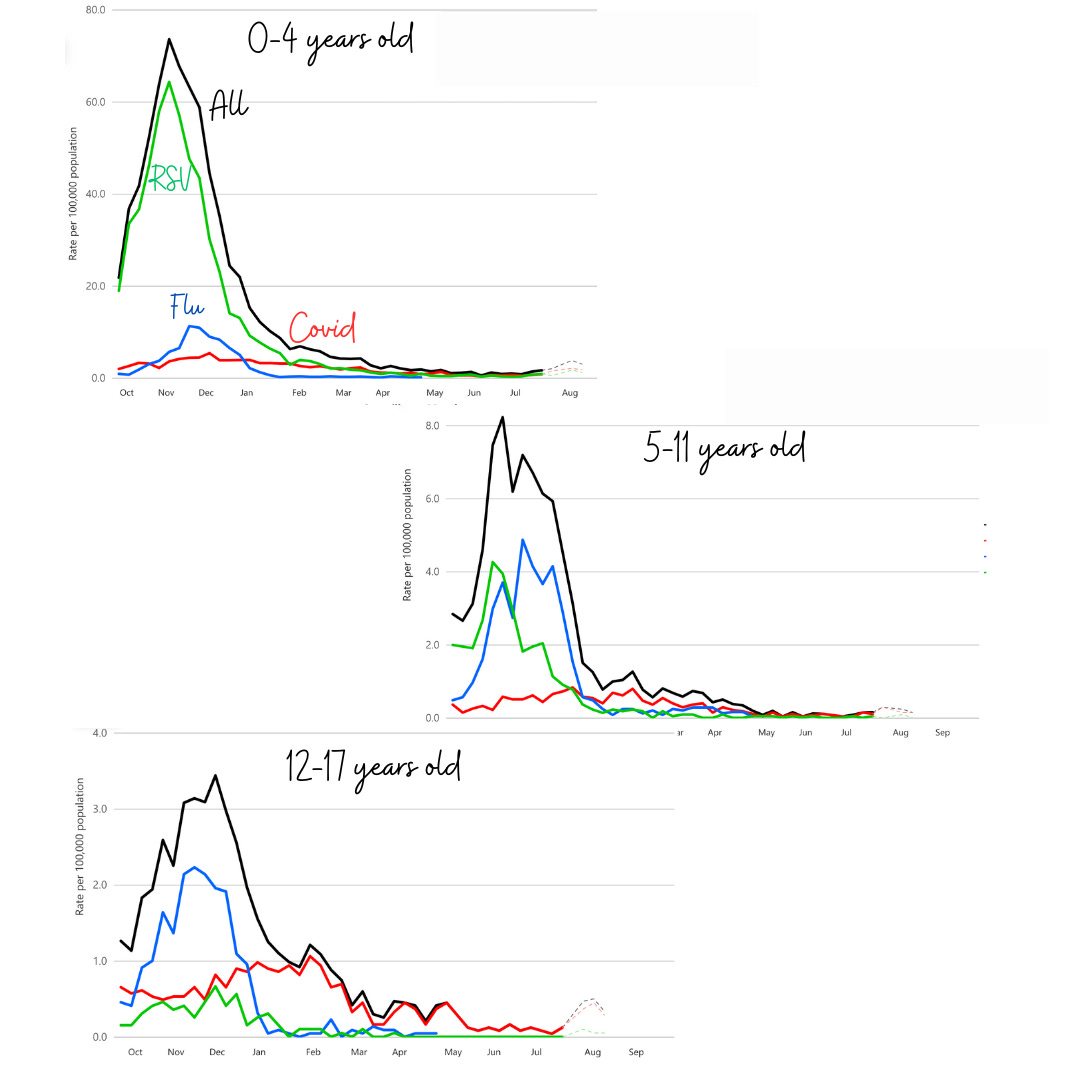
Flu and RSV activity is still low. Earlier this week, though, the CDC warned physicians of increased RSV activity in the Southeastern U.S. This typically signals the beginning of RSV season, in which the virus will subsequently spread to the Northeast and West over the next two months.

What to expect?
If this season mirrors the last, we will have unusual patterns of respiratory viruses:
RSV peaking in early November
Flu peaking in late November
Covid-19 peaking in late December
Nonetheless, expect illness. Last year, 1 in 4 students swabbed were positive for at least one virus in November. The severity of the threat depends on the virus and age bracket, as seen below in hospitalizations last year.
What can we do?
Improve air quality. Improve air quality. Improve air quality. This is a powerful tool, as it happens in the background: an institutional-level intervention that works passively and invisibly on the individual level. One study found infections were 40% lower in schools that improved air quality.
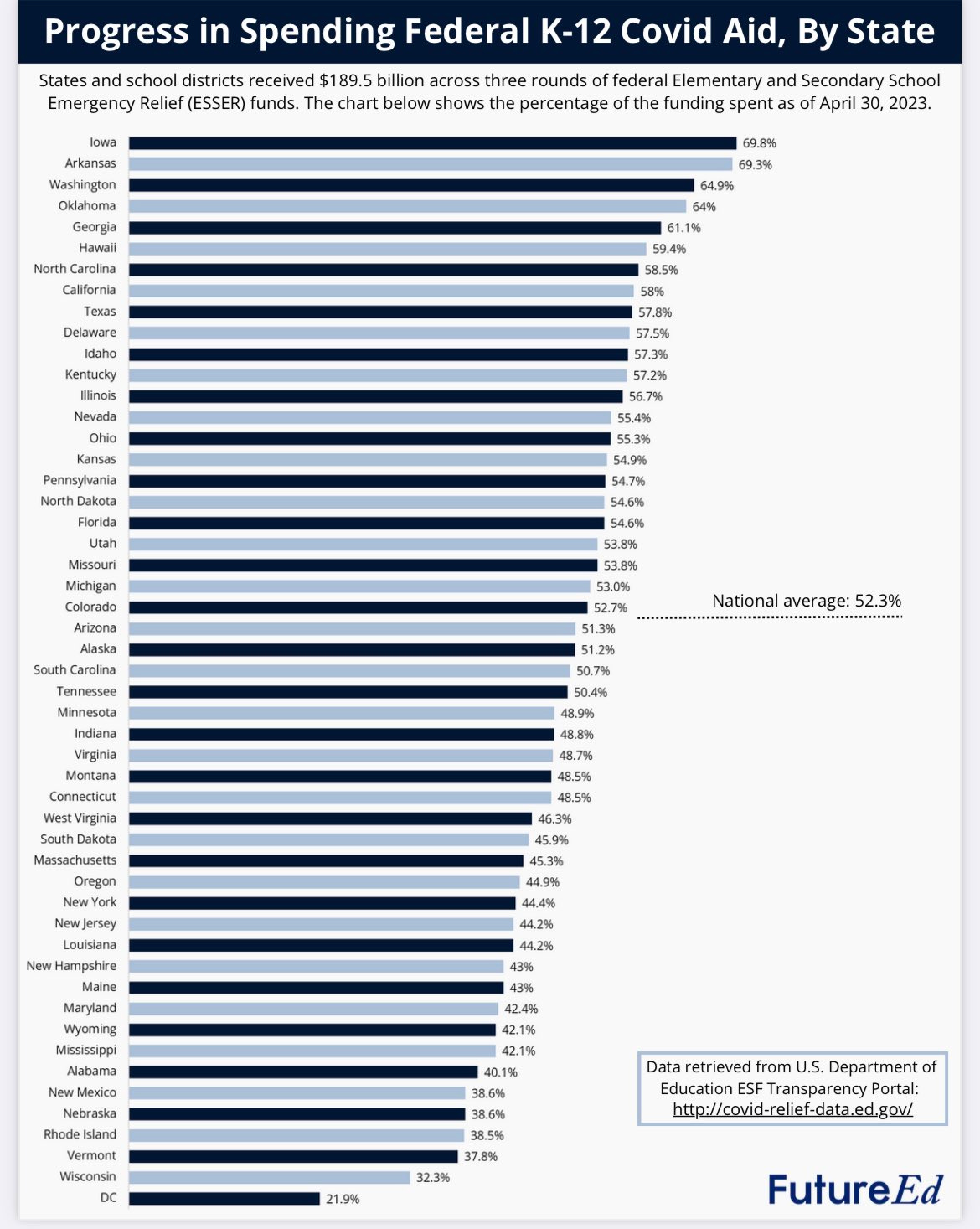
Advocate for your kids’ schools to optimally upgrade their ventilation system. Last year, 70% of schools reported upgrading their ventilation, but mostly with low-cost solutions like opening windows.
We can do better. A large Italian study found a 74% lower risk of infection in schools that upgraded systems compared to students in classrooms with just open windows.
There is federal money for this. But, as of April 2023, only 52% of the K-12 Covid aid money was spent.
At home, make sure to replace your filters after all the wildfire smoke this summer. Smoke particles reduce the performance of filters by 95%. This is because of the electrostatic charge wildfire particles carry.
Vaccinations
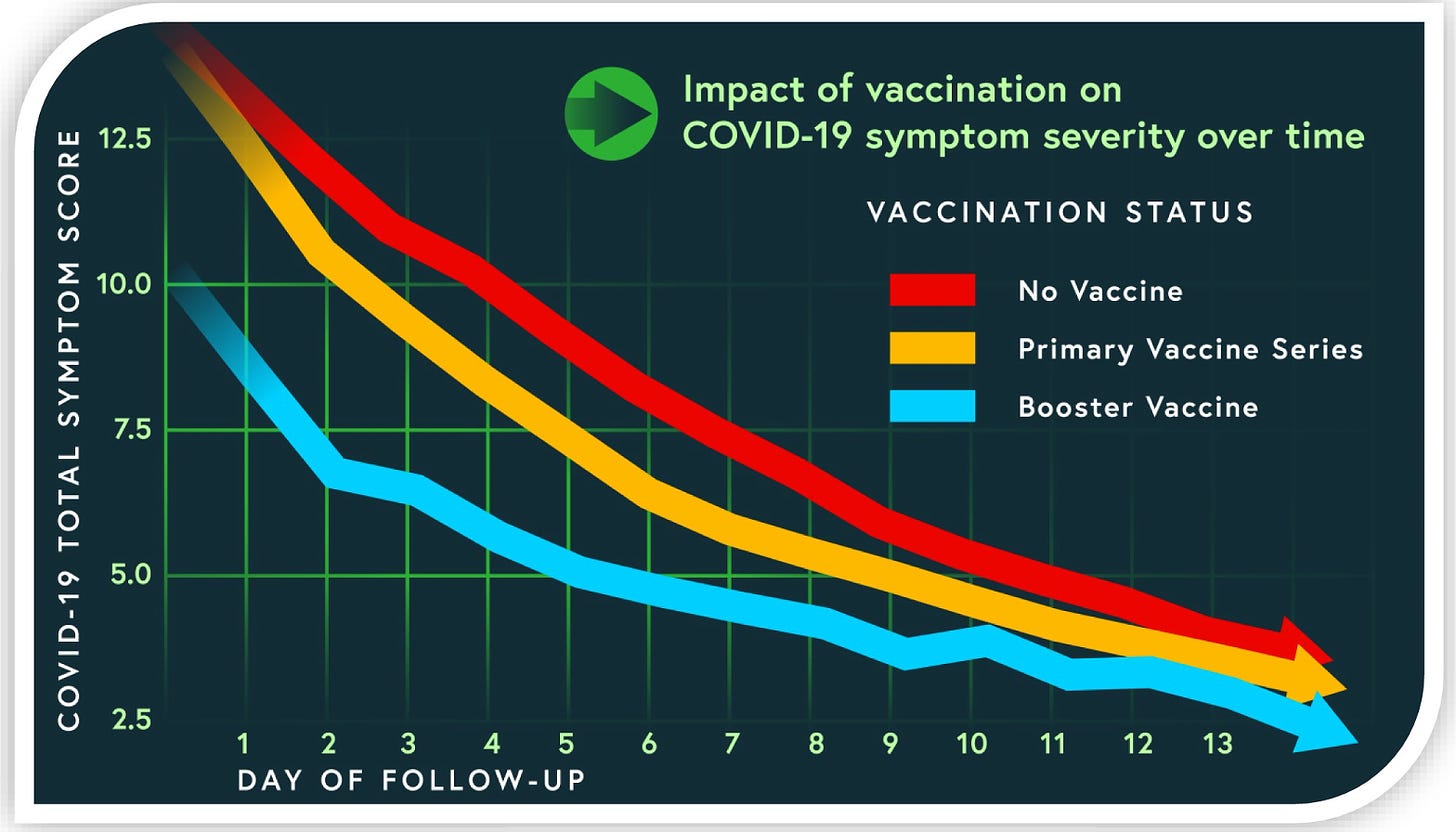
For the first time, we have vaccines for the big three (RSV, Covid-19, and flu). They help against severe disease, symptom severity, and keeping kids in school. Here are the options this fall.
A few parent-specific notes:
Flu vaccine: While protection wanes for older adults, it doesn’t wane as quickly for children. They should get one now.
Covid-19 vaccine: We should know next Tuesday who is eligible. Last fall, it provided 80% protection against emergency room and urgent care visits among children. Even if you’re not worried about severe disease, the vaccine reduces the severity and length of symptoms.
Masks reduce viral particles emitted and inhaled. In one of the best mask studies I’ve seen, school mask mandates also reduced transmission and absences. However, feasibility is challenging, given our increasingly individualized response and political inertia. If I had a healthy teenager, I wouldn’t push one in school unless required, school was about to close, or hospitals were crumbling because of too much illness.
Antigen tests are a great tool to know when someone is no longer infectious. Be wary of false negatives at the beginning of symptoms, though.
Bottom line
Fall is here, school is in session, and viruses continue to thrive. This seems like a revolving door, but we can slow it down—for our children’s health and learning, our sanity, and to help reduce the burden on schools, grandparents, and hospital systems.
From one parent to another, may the force be with you.
Love, YLE
“Your Local Epidemiologist (YLE)” is written by Dr. Katelyn Jetelina, M.P.H. Ph.D.—an epidemiologist, wife, and mom of two little girls. During the day, she is a senior scientific consultant to several organizations. At night, she writes this newsletter. Her main goal is to “translate” the ever-evolving public health world so that people will be well-equipped to make evidence-based decisions. This newsletter is free, thanks to the generous support of fellow YLE community members. To support this effort, subscribe below:





Disagree on the recommendation not to push masking for currently healthy children as this blatantly disregards the risks of Long COVID resulting in no longer healthy children. Particulalry when you corrently point out how little states have done to address indoor air quality in schools (which would benefit much more than just COVID/other airborne illnesses, to include allergens and overall cognitive function once CO2 levels are lowered to healthy levels). Disappointing to say the least.
The very different NYC hospitalization rates for unvaccinated adults vs vaccinated adults are still shocking to me - vaccination STILL making a big difference.
Very interesting about home air filters becoming 95% less effective due to charged wildfire particles. Amazing how much of the smaller particle/virus filtration may be electrostatic versus mechanical apparently.
And finally, I am bracing myself for disappointment regarding the CDC meeting. In an interview with PBS, Dr. Offit (whom I respect greatly) stated that he believes the new boosters should only be recommended for 75 yo and up:
https://www.pbs.org/newshour/health/your-fall-guide-to-covid-rsv-and-flu-vaccines
As an FDA advisor, he has a lot of influence and expertise...
Yet the game is not just reducing risk of hospitalization and death, but also reducing long Covid burden and disability, community spread, and boosting some modicum of herd immunity, even if temporarily through the anticipated peak Dr. Jetelina is talking about this December perhaps.
I don't think there is enough data out there to definitively determine whether boosters reduce long Covid, but just because enough studies haven't been done doesn't mean we can't take a small intuitive leap of faith?
Vaccination absolutely reduces long Covid risk, perhaps around 40% reduction according to this meta-analysis:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9905096/
The same analysis showed up to 20% of people already experiencing long Covid reported improvement in symptoms after a booster.
Maybe I'll find time to leave public comment about this for the CDC meeting, but if anyone else has a similar (and more evidence based!) assessment regarding boosters and long Covid, please advise or leave a public comment by tomorrow. Any known studies on this would be greatly appreciated.
https://www.federalregister.gov/documents/2023/08/25/2023-18288/advisory-committee-on-immunization-practices