Here’s an update on our three, global public health emergencies. I’ve included an update on flu, too.
COVID-19
Globally, deaths from COVID-19 are on the decline, again. During a media briefing last week, WHO Director General Tedros provided a reaction: “We have never been in a better position to end the pandemic. We are not there yet, but the end is in sight. (But)… a marathon runner does not stop when the finish line comes into view. She runs harder, with all the energy she has left… Now is the worst time to stop running.”
No one knows where this finish line is exactly. In the U.S., whispers suggest the end of the public health emergency will be in mid-2023, with signals that we are moving to privatize tests, treatments, and vaccines. Yesterday, Biden suggested on 60 Minutes that the “pandemic is [already] over”. This is hard to believe given an average of 400 Americans are dying each day. But, as I’ve written before, the “end of a pandemic” isn’t purely epidemiological, but also physiological, cultural, political, and moral. Essentially we’re collectively deciding where we place SARS-CoV-2 in our repertoire of threats. To me, this winter will be a true test as to whether we are still in an “emergency” phase, at least if we define this by deaths, hospitalizations, and healthcare capacity (opposed to infection or long COVID).
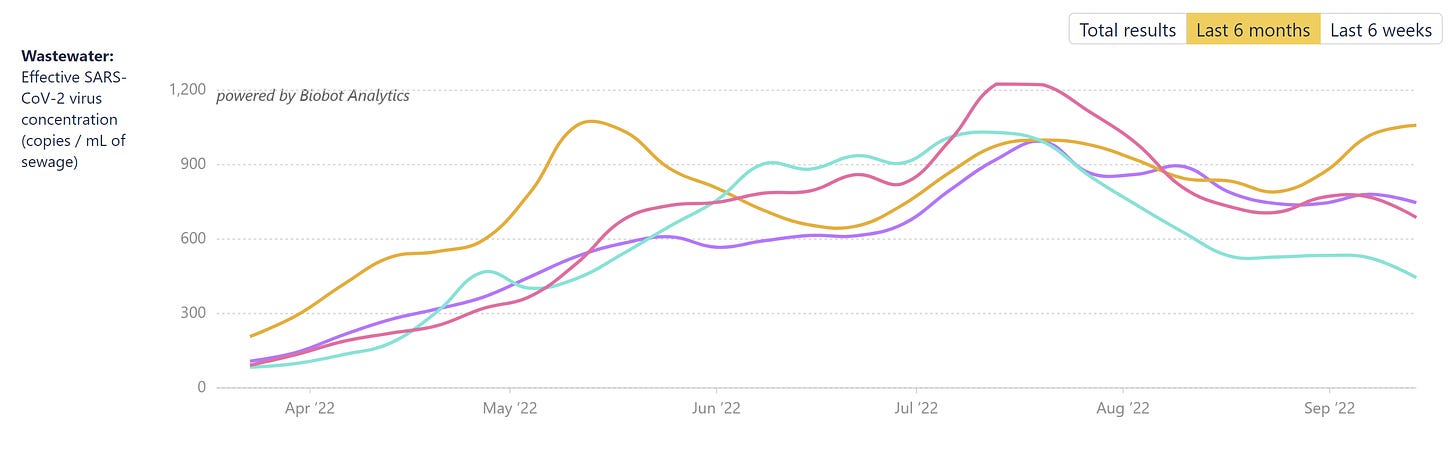
Currently, the Omicron subvariant BA.4.6 is taking hold in the U.S., and we are getting the first signs that it can outcompete BA.5. Wastewater levels have begun to rise in the Northeast where BA.4.6 is most prevalent. Also, for the first time last week, cases of BA.4.6 started rising while BA.5 cases started falling. We don’t think BA.4.6 will cause a big wave, as it doesn’t have mutations on the spike protein to escape our immunity, but coupled with behavior change and weather change, I guess anything is possible.
SARS-CoV-2 continues to mutate, and there are a few Omicron variants, like BA.2.3 and BJ.1, on the horizon with potentially concerning combinations of mutations. But evidence thus far is extremely limited. Most eyes are on BA.2.75.2, which is a second generation subvariant and has three additional spike protein mutations. Two preprints have shown substantial immune escape, even compared to BA.5. This means it has the potential to cause future waves. The number of BA.2.75.2 cases is still very small across the globe, but counts are doubling every week. If this growth rate continues, BA.2.75.2 may be one that causes the much anticipated winter wave.
Monkeypox
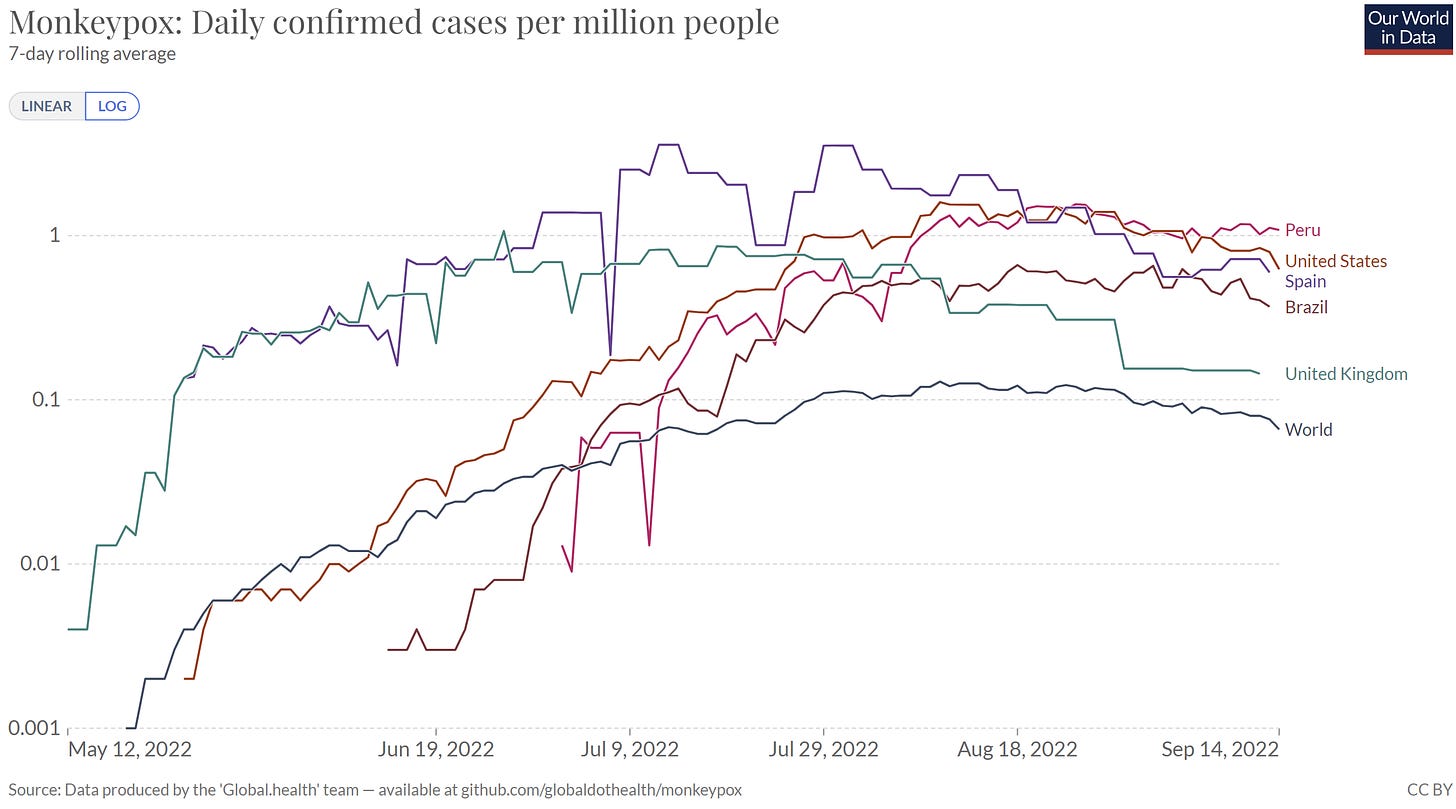
Monkeypox (MPX) is getting under control as global cases continue to decline. Even in places like U.S., Peru, and Brazil, case growth has plateaued and even decelerated. This. is. fantastic. news. And we have to applaud the gay community for working tirelessly in communication, outreach, and vaccination. But we still have a long way to go. MPX is a very different virus than COVID19, so our goal needs to be containment and nothing less. We can do it.
There have been 24 MPX global deaths, and last week we confirmed the first American death among a severely immunocompromised person in Los Angeles.
In the U.S., the CDC has started releasing rapid data summaries and technical reports. They have been fast, clean, and data driven. This shift in science communication is nothing short of fantastic and I hope a reflection of CDC’s new direction. The reports provide the best picture we have of MPX on a national level.
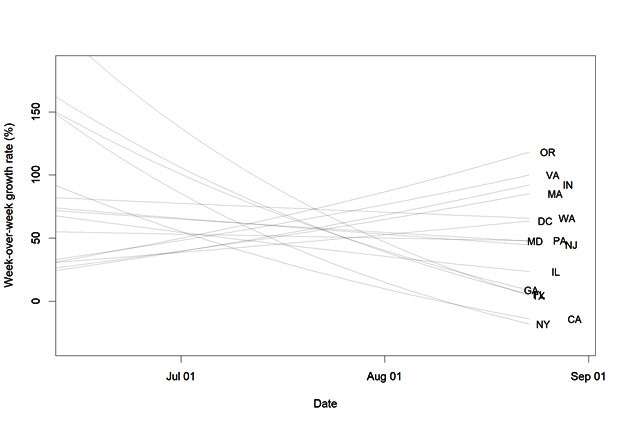
While we have a national decline in MPX cases, this comes with substantial variation by state. States like OR, VA, and MA are seeing a fast incline in cases, while the original case leaders, like NY and CA, continue to decline in MPX cases.
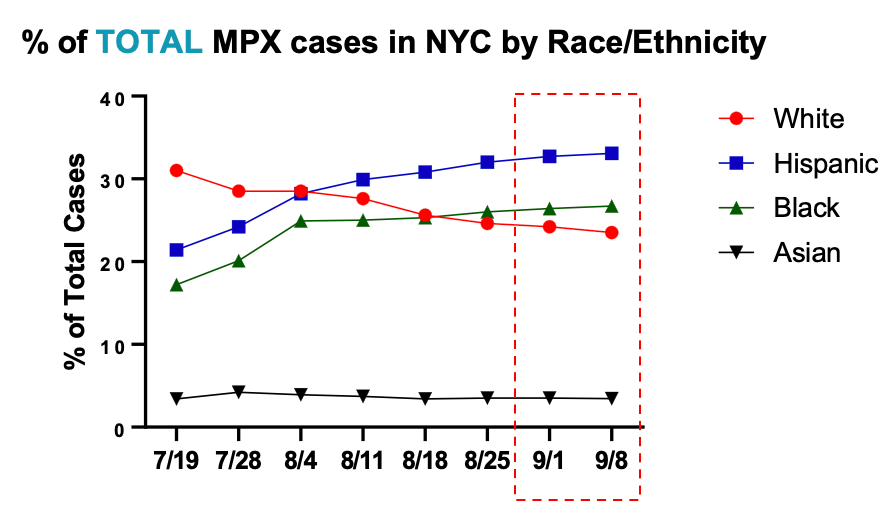
Unfortunately, this also comes with substantial variation by race and ethnicity, as we continue to see immense inequities in cases, testing, and vaccinations. For example, in New York City, cases among Hispanic people continue to rise while cases among non-Hispanic White people are clearly on the decline.
North Carolina’s last equity report showed a clear vaccine allocation imbalance: 70% of cases were among Black men and Black residents only received 24% of vaccinations. This calls for more culturally nuanced vaccine education, outreach, and behavioral communication. I’m excited to hear what CDC’s new initiative, the MPX Vaccine Equity Pilot, will offer.
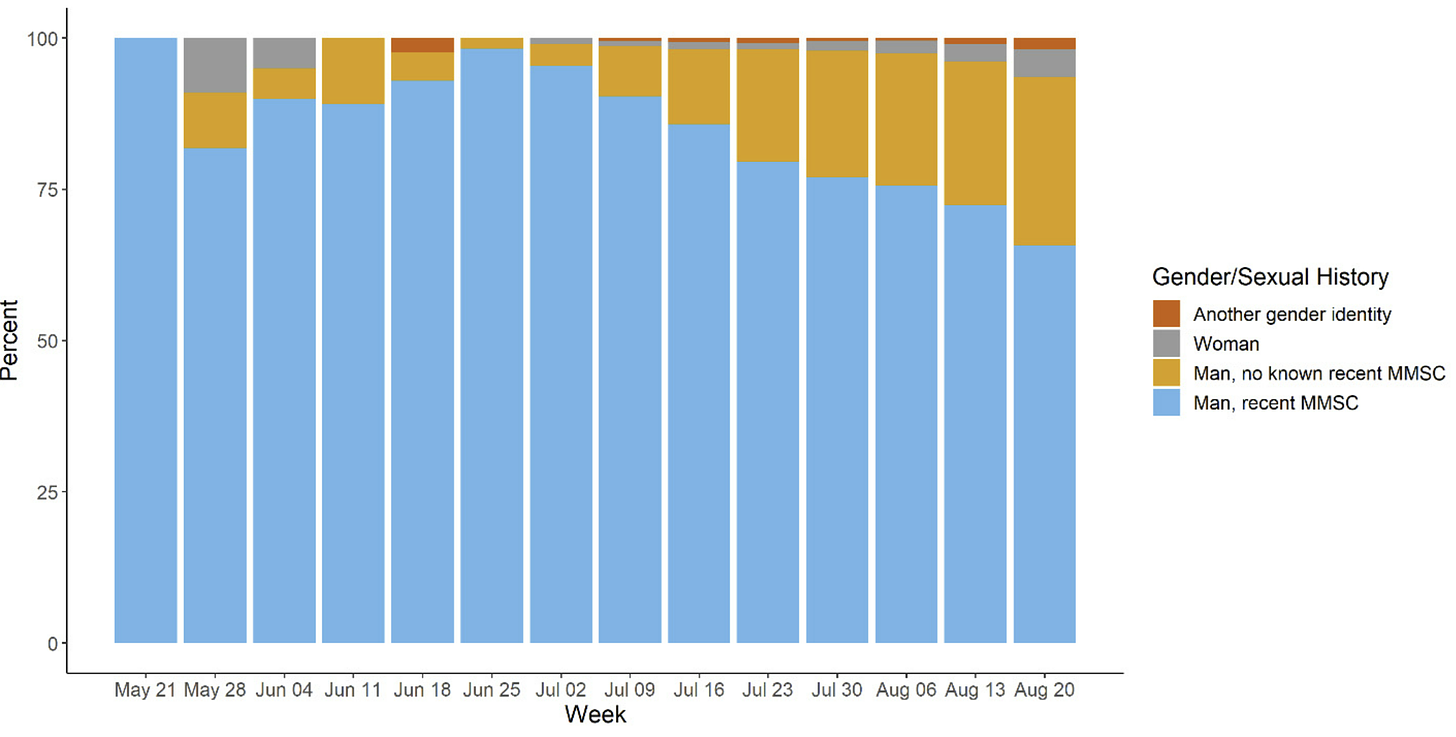
Global signs continue to point to an MPX outbreak among men who have sex with men (MSM), with WHO data showing 95% of cases as MSM. In the latest U.S. technical report, cases among men who have not had sex with men are increasing. Interestingly, female cases are not also increasing. This unusual pattern is probably due to the y-axis—the number of cases among MSM are decreasing so other categories are increasing. But only detailed contact tracing data can help us understand whether MPX is infiltrating other social networks.
Polio
According to the Global Polio Eradication Initiative, the paralytic case in New York last month is genetically linked to two cases in Israel and one case in London. This suggests a large, international, and silent outbreak.
New York recently declared a state of emergency following the detection of polio virus in a fourth county’s wastewater. Unfortunately, this means there’s enough circulating polio virus with enough genetic mutations that the WHO added the U.S. to a list of countries with active circulating polio. This is a list that no country wants to be on. It’s both a remarkable and an incredibly disturbing moment in public health.
Certain workers in NY can now get a polio booster, even if they’ve previously been fully vaccinated for polio.
Flu
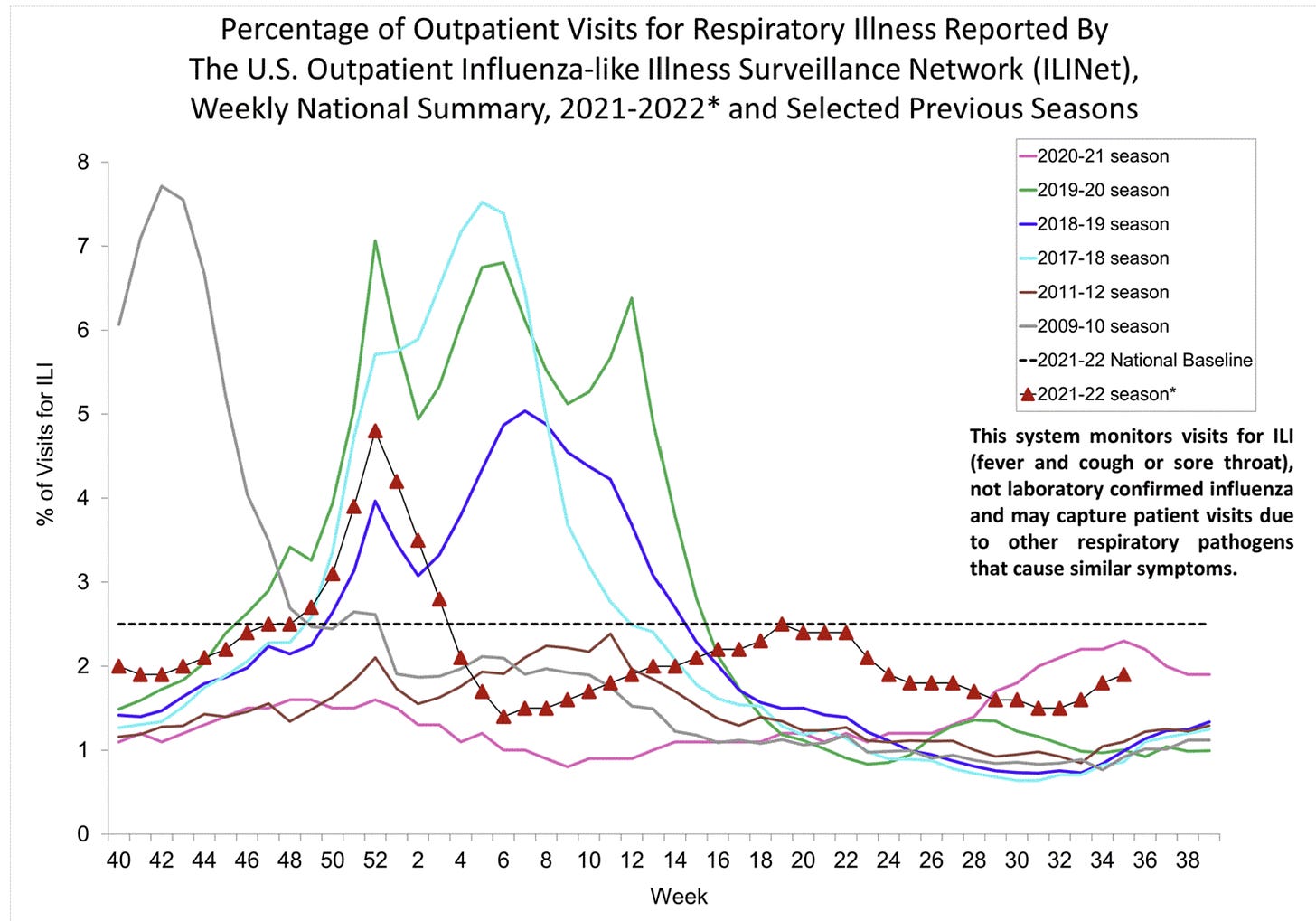
Finally, flu. The flu season in Australia wrapped up, and it wasn’t pretty. This is notable because, historically, Southern hemisphere patterns predict what is to come in the Northern hemisphere.
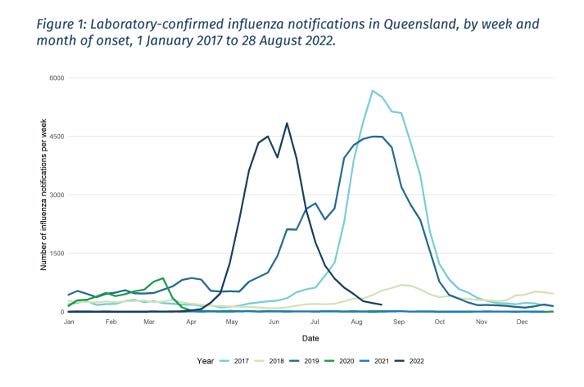
U.S. flu activity remains low, as is typical this time of year, but flu season is just around the corner. Given the Southern hemisphere’s warnings, we predict that this activity will change. However, right now, the only predictable thing about viral behavior is that it is unpredictable.
Bottom line
The dynamics of all these viruses continue to change. Stay healthy by getting up-to-date on your vaccines, which now includes a COVID-19 bivalent and flu shot. If you’re eligible, get your polio and monkeypox shot, too. Our immune systems could use all the help we can get going into the winter season.
Love, YLE
“Your Local Epidemiologist (YLE)” is written by Dr. Katelyn Jetelina, MPH PhD—an epidemiologist, biostatistician, wife, and mom of two little girls. During the day she works at a nonpartisan health policy think tank, and at night she writes this newsletter. Her main goal is to “translate” the ever-evolving public health science so that people will be well equipped to make evidence-based decisions. This newsletter is free thanks to the generous support of fellow YLE community members.




I think Long Covid and other long-terms effects of infection (e.g., organ damage) need to be an important part determining whether or not we’re still in an emergency phase of the pandemic - or in a pandemic at all. It shouldn't be just about deaths, hospitalizations and healthcare capacity.
I got the updated booster as soon as possible and am counting the 14 days. But now with the other variants rising, are we still vulnerable? I was going to be dancing in the streets and going to movies and restaurants again after living like a monk.