
Oof, we are coming out of the holidays and seeing the impact on viruses: there is a lot of sickness out there. I’d wager that we are around peak respiratory season. While a few patterns are unusual, this is a pretty middle-of-the-road season overall.
Here is your state of affairs.
Influenza-like illnesses: Very high
The climate of respiratory health in the United States (the CDC coined “influenza-like illnesses”) is very high. Over the holidays, exponential growth finally kicked into gear, given changing temperatures and seeing people we wouldn’t normally socialize with.
Today, about one out of six pediatric visits to the doctor is for fever, cough, or sore throat. This is nothing unusual, though, as we are closely following pre-pandemic patterns.
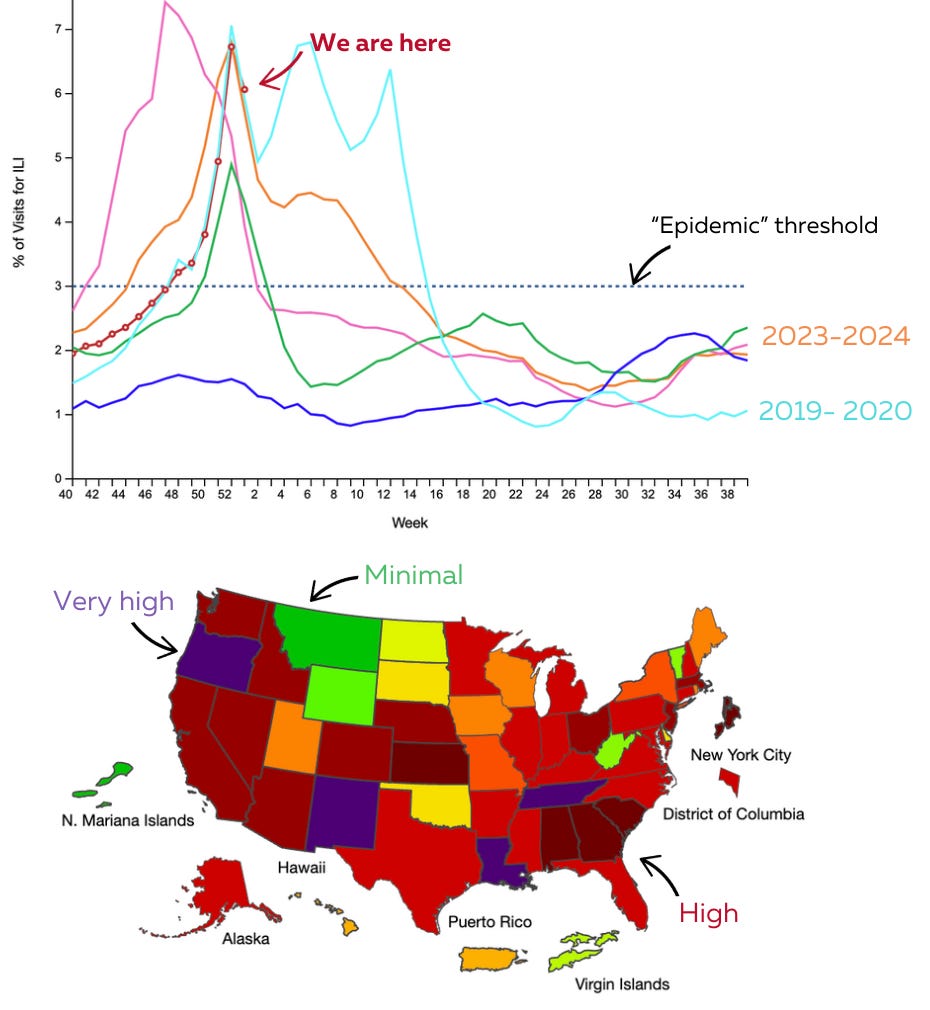
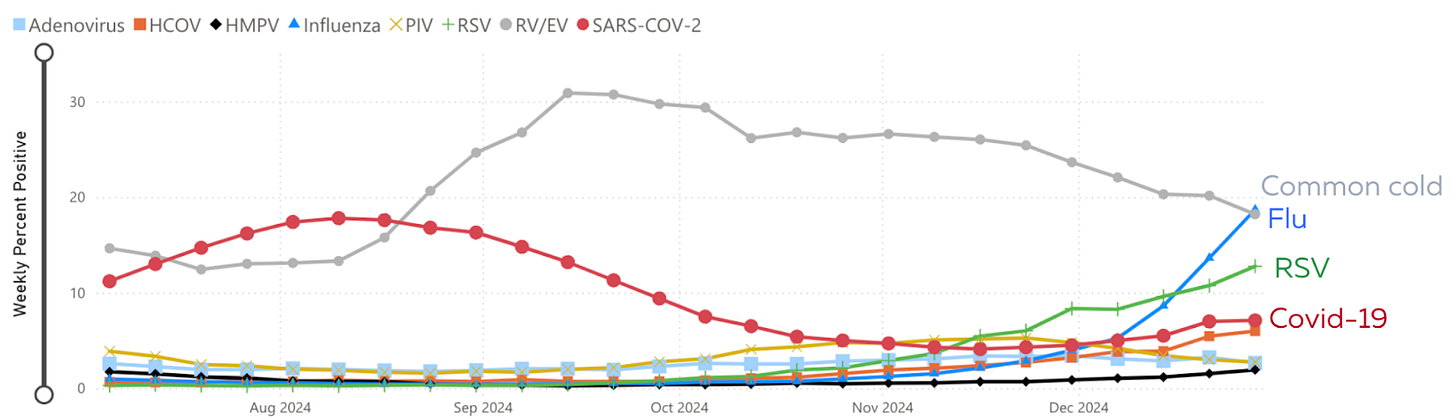
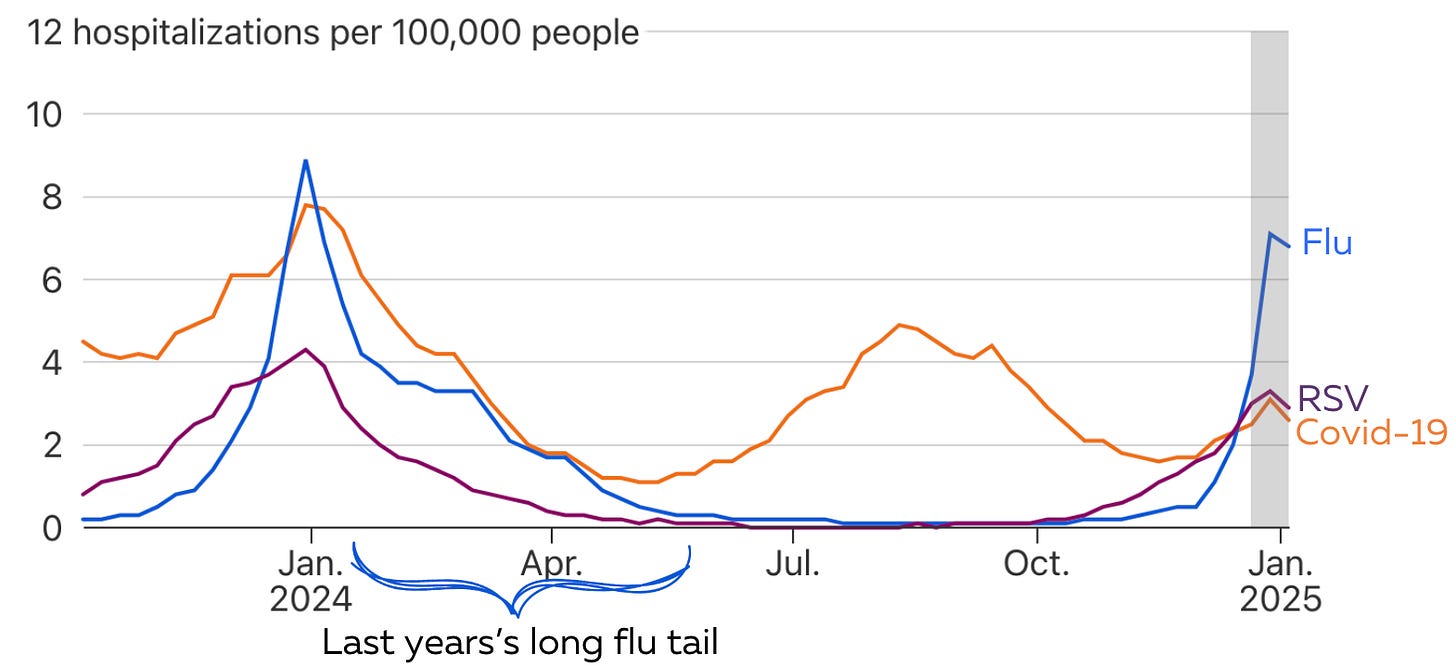
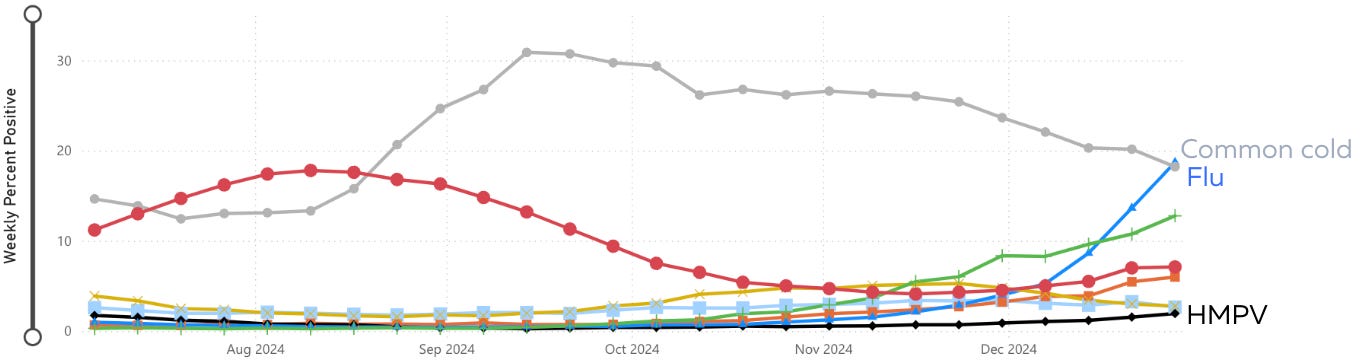
What virus is the main culprit behind these symptoms? Common cold and flu, with RSV and Covid-19 following behind.
Now for a deeper dive into the “big three.”
Flu: High but slowing down
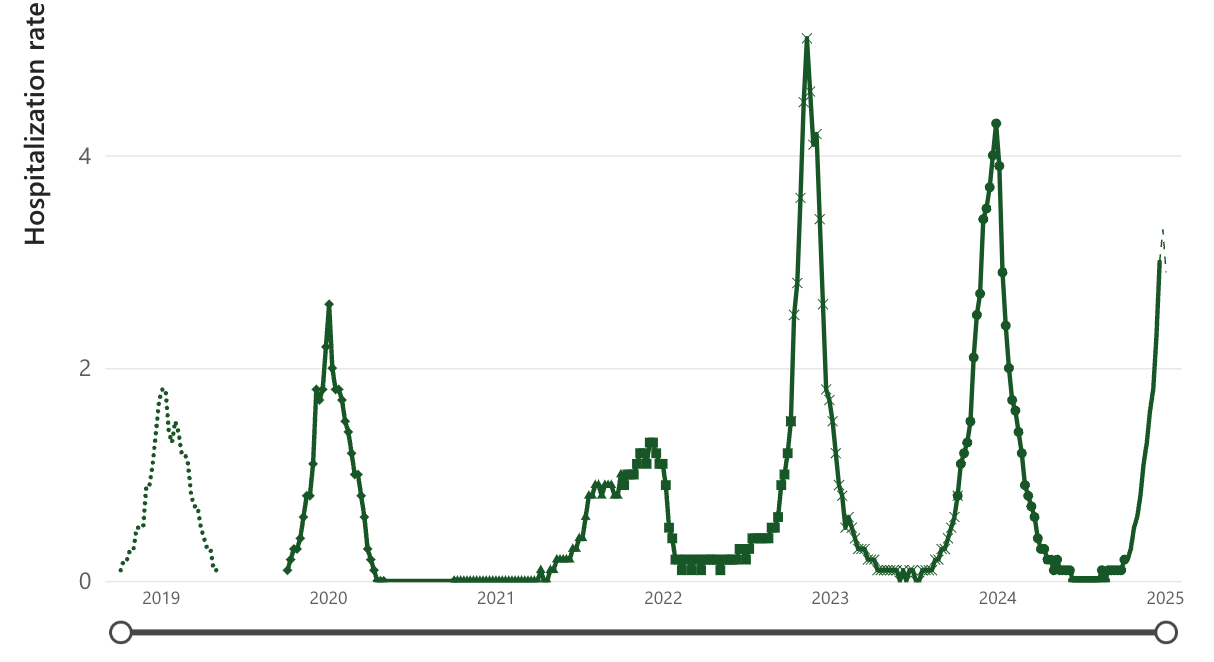
Flu continues dominating the scene, accounting for more than double the number of emergency room visits and hospitalizations.
The latest numbers suggest that flu peaked. It may have, but we aren’t in the clear yet. Typically, we get two waves of flu– first, the Flu A strain takes over, and then Flu B comes in late winter or early Spring. This causes a long tail of flu (see last season above, for example).
Covid-19: High and increasing
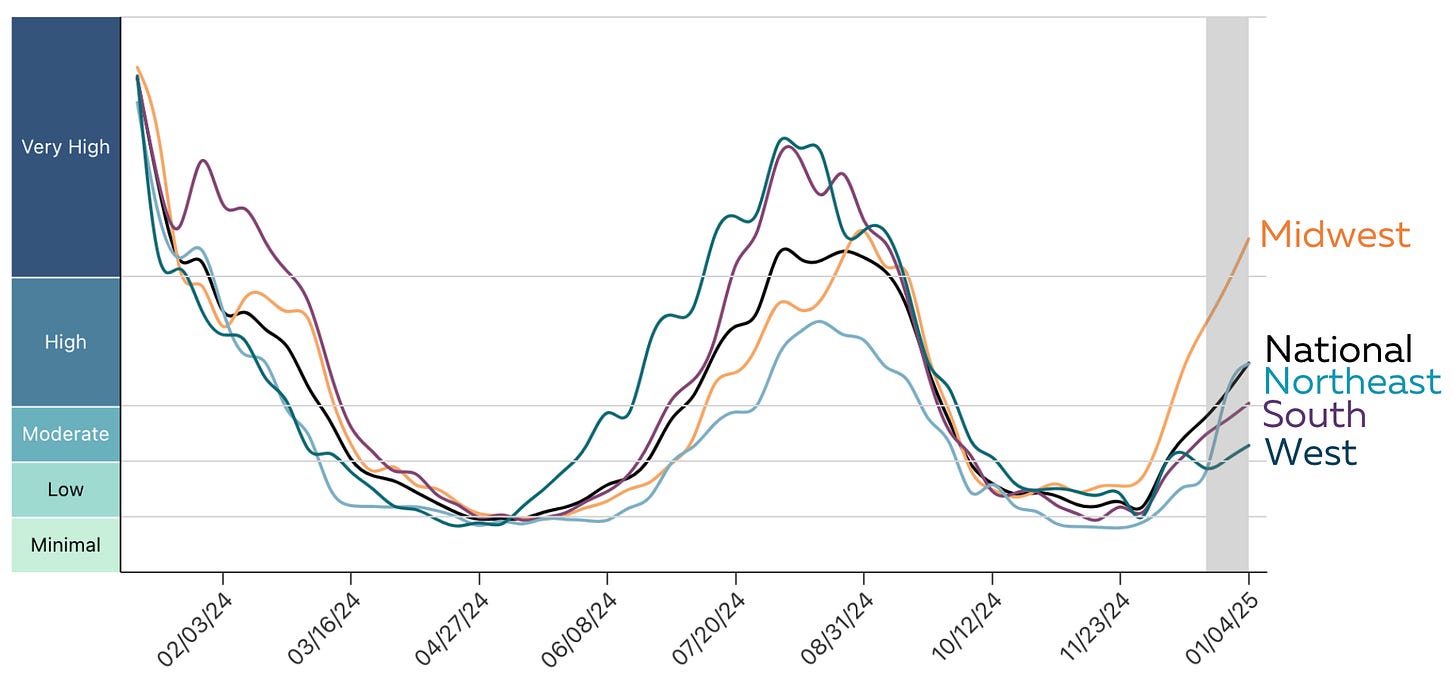
Covid-19 levels in wastewater (a good indicator of community spread) are rising across the U.S., most starkly in the Midwest with “very high” levels and a recent uptick in the Northeast.
Over the past four years, Covid-19 has taken off during the winter. However, this year’s metrics—wastewater, percent positivity, emergency room visits, and hospitalization—are much lower than in previous winters. This unusual pattern is due to several things:
Big summer wave, so there is lots of built-up immunity.
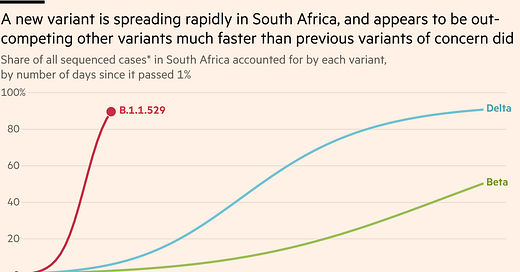
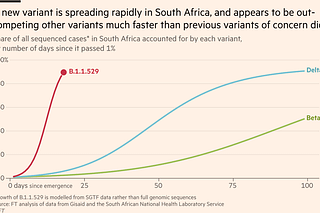
The virus hasn’t mutated in a huge way.
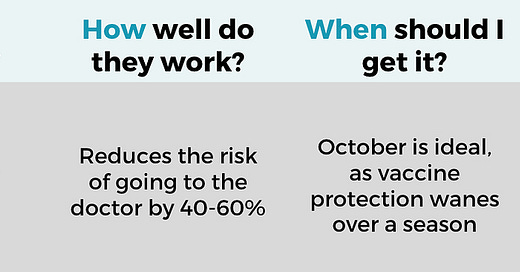
More are vaccinated. For example, 12% more people over 65 years old were vaccinated for Covid-19 this year than last.
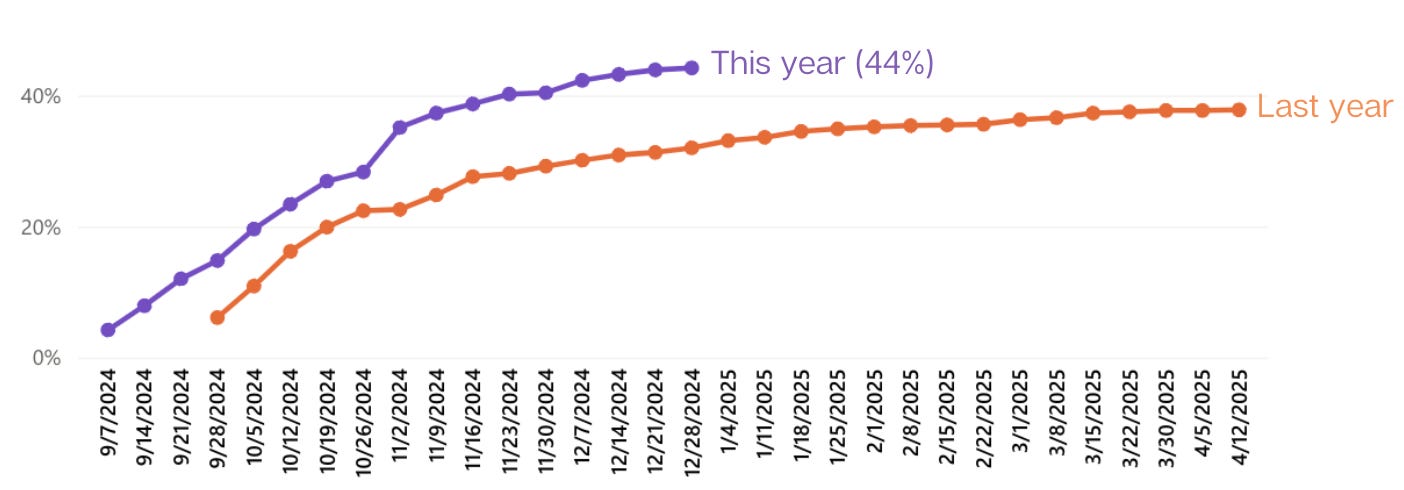
Some metrics even show signs of Covid-19 already peaking. We’ll see if this trend continues, but if it does, we will have had our mildest Covid-19 winter yet. I don’t think anyone is complaining.
RSV: Declining
RSV is still around, but activity is declining. Hospitalizations lag cases, but pediatric severe diseases have peaked, and adults should follow soon.
Interestingly, we still see higher RSV rates than before the pandemic. Research suggests this is largely due to increased testing, but it could also be due to two years of low activity—population-level immunity among our kids is still catching up. However, the broad case that Covid-19 is doing something to our immune systems to cause more severe disease from other viruses is weak.
Other things going around
HMPV made headlines in China and India, causing a global stir. But this is an old virus (discovered over 40 years ago) in the same family as RSV. It’s always more active during late winter/early spring but causes less severe disease than the flu or Covid-19. Because it comes every year, our population has a high level of immunity. Regardless, levels are still low in the U.S. (see black line below). This is not a virus to worry about.
Norovirus (think vomiting and diarrhea) continues to have a higher-than-normal season. We don’t know why, but typically, the virus mutates ever so slightly when this happens. Norovirus is extremely contagious—if you have kids in school, it may come home to you. It’s most likely to spread through surfaces, so bleach surfaces and wash those hands.
Bottom line
There are a lot of sick people out there. Other than Covid-19 infections, this winter seems to largely mirror pre-pandemic times.
It’s not too late to get vaccinated—even if things start to peak, we are only halfway through the journey. Continue to wear that mask in crowded indoor areas and, if possible, get that indoor air moving; it will help.
Love, YLE
Your Local Epidemiologist (YLE) is founded and operated by Dr. Katelyn Jetelina, MPH PhD—an epidemiologist, wife, and mom of two little girls. During the day, Dr. Jetelina runs this newsletter and consults with several nonprofit and federal agencies, including CDC. YLE reaches more than 296,000 people in over 132 countries with one goal: “translate” the ever-evolving public health science so that people feel well-equipped to make evidence-based decisions. This newsletter is free to everyone, thanks to the generous support of fellow YLE community members. To support the effort, subscribe or upgrade below:













Thanks, as always! Would you consider an updated post on the case for covid broadly messing with the immune system (or not)? I am with you that a return to pre-pandemic viral trends is a good sign that we are generally doing pretty ok, but the immune system damage argument is one I hear repeated all the time. I think I get where it is coming from, but I also think many of those studies are pre-vax and wild type or early variants and we may need to update our priors. This is a hard line to tow, and I appreciate you continuing to keep us updated!
Thank you for all your work. My husband and I got the updated Covid vaccine in September as we finally were caught by it last March. Hoping we'll still have some protection from it when we travel in February - will still be masking on plane and indoor areas!