XE— a new sister lineage of Omicron— has peppered the headlines this week. And while it’s important for scientists to track every change of the virus, I don’t think the public needs to be anxiety-ridden every time this virus changes. This is what viruses do to survive, and we should anticipate this. In fact, Omicron mutating may be good news for us.
XE (And XG, XR, Xl, etc., etc.,)
XE is not a new variant of concern. Instead it’s a recombinant or a combination of BA.2 and BA.1. As like what happened with “Deltacron,” XE was likely created when someone was infected with two different viruses at the same time. We are seeing more and more recombinations now because distinct viruses are circulating (Delta, BA.1, BA.2) at the same time.
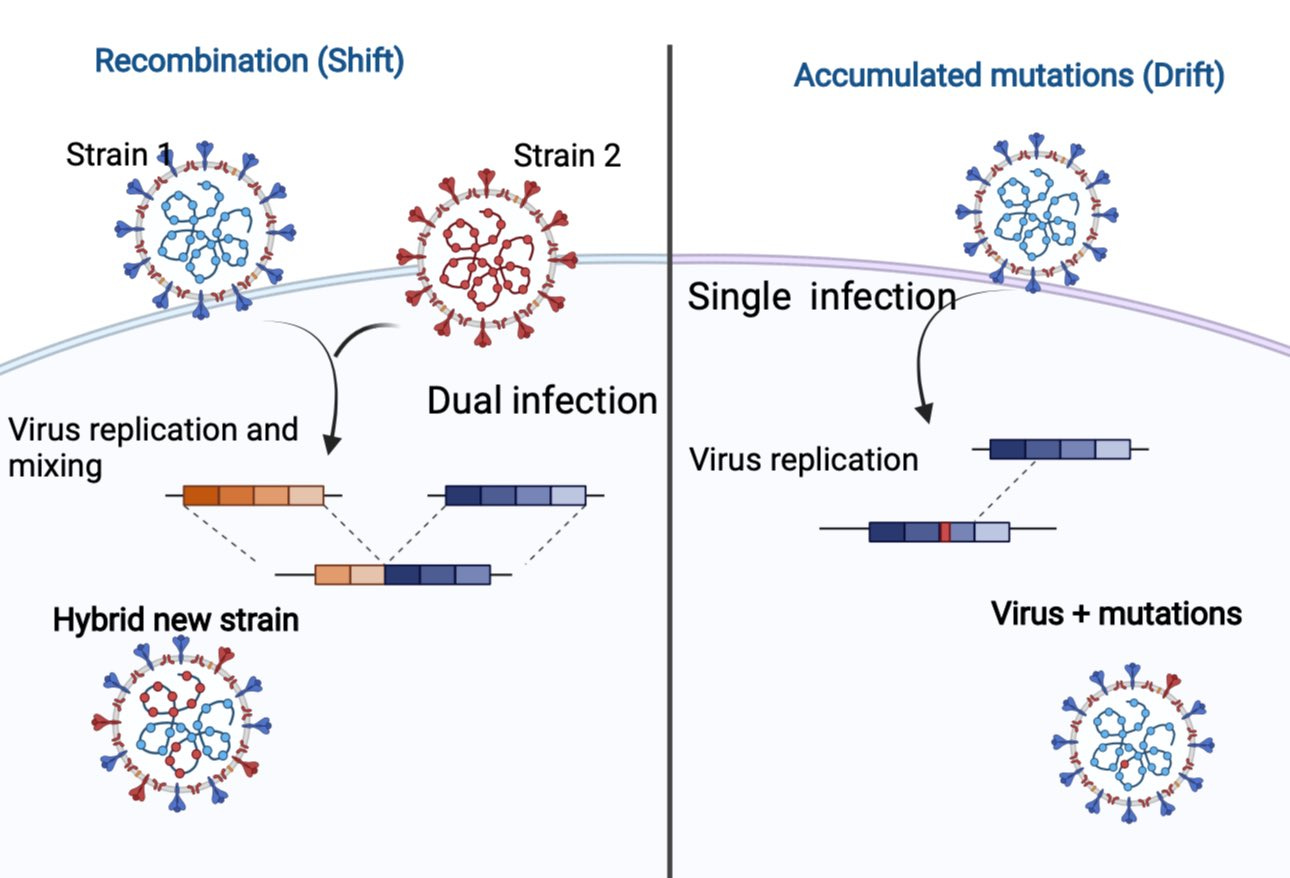
Because someone can be infected with two viruses at the same time, the two sublineages can enter a person’s cell at one time. Then, when the virus tries to replicate inside the cell (to further spread to other cells), the genetic material can be mixed up. This is different from a mutation from a single infection, as depicted from the figure below.
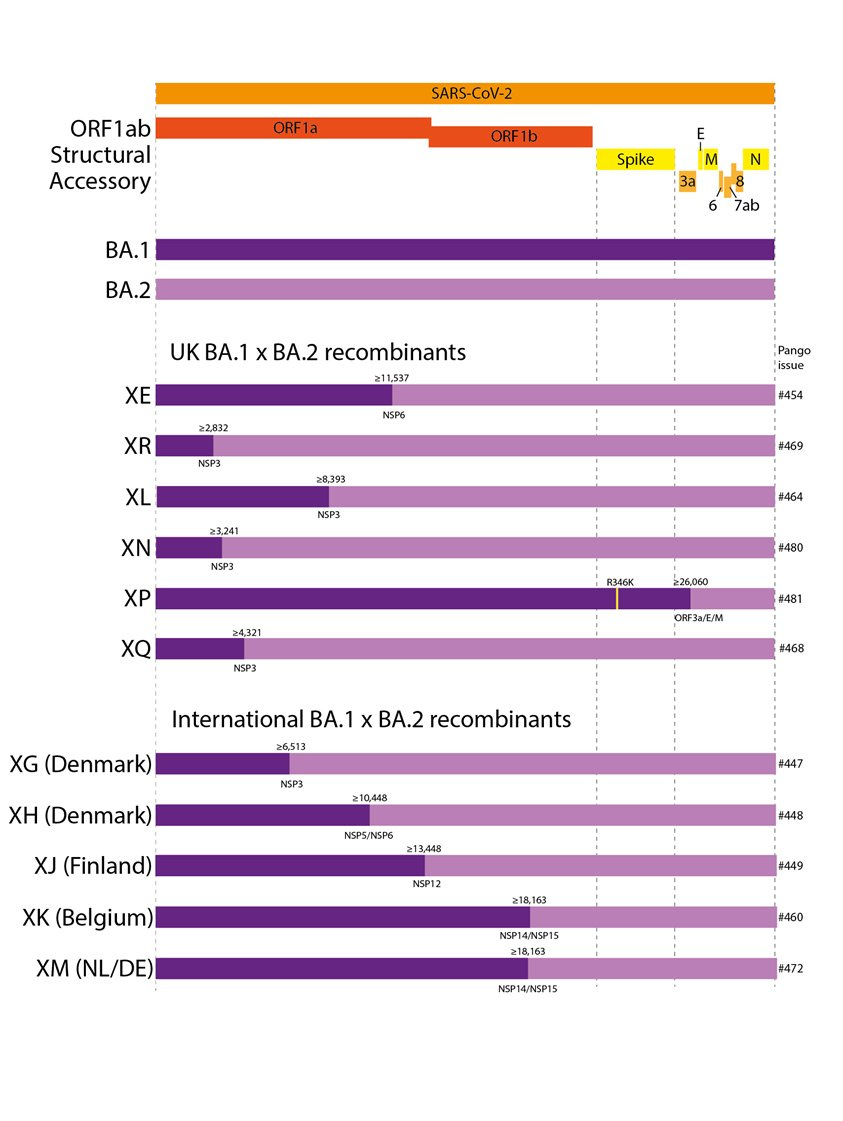
XE has BA.2’s spike protein copied and pasted onto the 5' part of BA.1. We have documented BA.1 and BA.2 mixing in other ways, too, which has resulted in other sublineage names like XR, XN, XP, XQ, etc., etc. Virologist Tom Peacock made the fantastic figure below displaying the phenomenon.
XE was first detected in England in mid-January and has caused more than 600 cases in England (which is <1% of cases). As of March 22, 763 XE cases had been identified in the greater U.K. It’s also been identified in India, China, and Thailand.
Since March 25, XE has shown modest growth advantage over BA.2. Latest estimates from the U.K. are showing a 10% increase of transmissibility over BA.2 (and BA.2 has a 40% increased transmissibility over BA.1, or the original Omicron). This means XE is slightly more contagious than the other sublineages.
The good news is that because the spike protein determines immune invasion, infection-induced defenses that people acquired against Omicron and/or our vaccinations should still work against this new recombinant.
The WHO said they won’t give XE a Greek letter name and will still consider it Omicron until “significant differences in transmission and disease characteristics, including severity, may be reported.” These differences haven’t been found so far. At the end of the day, XE is still considered Omicron.
Omicron mutating could be good news
While it would be wonderful if this virus just disappeared, this isn’t going to happen. It’s going to continue to mutate, especially given the high transmission levels across the globe.
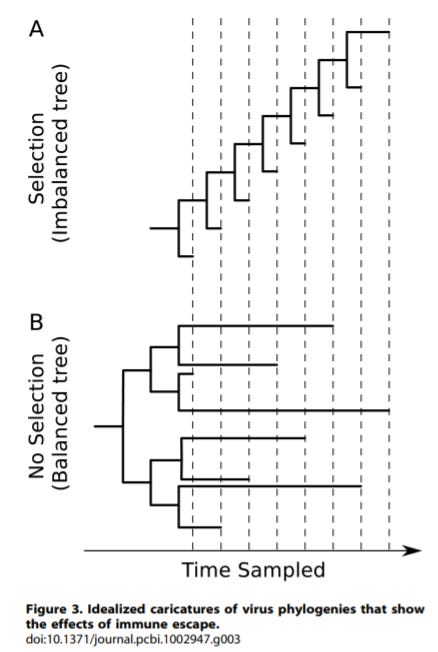
Unfortunately, two years into this pandemic, this virus hasn’t provided any hints about where it’s going. Like I’ve written before, coronaviruses typically evolve in a ladder-like pattern. The flu does this, too. In other words, there is one major lineage, and every few years, a new variant sweeps and the others go extinct. (See Panel A in the figure below for a depiction).
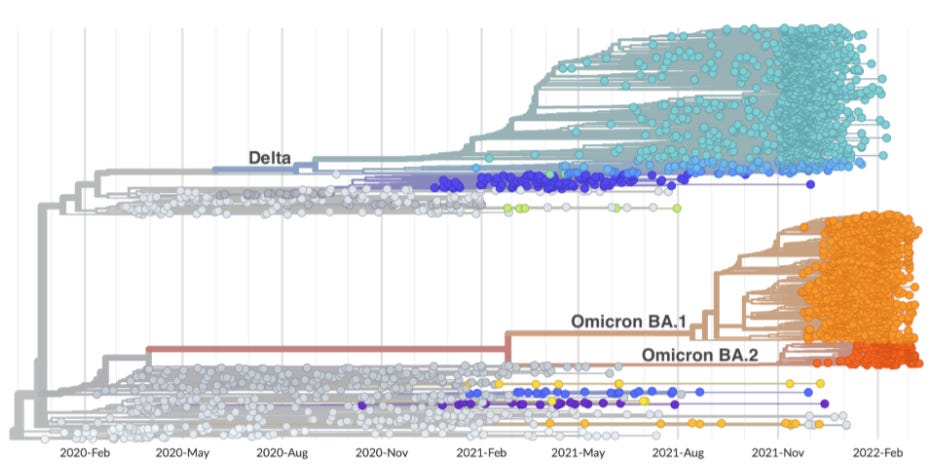
But we haven’t seen this pattern with SARS-CoV-2. The next big variant hasn’t been coming from the last: Omicron didn’t come from Delta, and Delta didn’t come from Alpha. Instead, SARS-CoV-2 evolution looks like Panel B in the figure above. And this is incredibly puzzling.
But this may be because we just haven’t given it enough time. It’s only been two years, and other evolutionary trees, like the common cold, also had two-year time frames in which there were no ladder-like changes.
If SARS-CoV-2 starts evolving in a ladder-like pattern (something we would eventually expect) from Omicron then it will have more “flu-like” drift in evolution. This means that SARS-CoV-2 will inch towards more immune escape and higher transmissibility. This, coupled with seasonality, will determine attack rates. But it won’t be huge, unpredictable jumps like we saw with Delta → Omicron. And if we have more “flu-like” drift with SARS-CoV-2, this would be good news for two reasons:
We won’t have sweeping attack rates for a while. That’s because ~50% of Americans were infected by Omicron in 10 weeks. (Which is completely mindboggling. We’ve never seen a virus burn through a population at this rate. As a comparison, the flu infects 10-20% of a population in a span of 20ish weeks.) Large infection-induced immunity coupled with vaccine coverage will no doubt help build an immunity wall.
If SARS-CoV-2’s future becomes more predictable, then we’ll be able to anticipate mutations and prepare. For example, we could then plan to develop, roll out, and distribute updated vaccines like we do with the flu every year. There was an 8-hour discussion about this very topic at the FDA this week.
The virus is changing incredibly quickly, but a huge event in the next 12 months isn’t likely
We just don’t know what will happen next, though. Dr. Trevor Bedford, evolutionary virologist, made two big points during his presentation to the FDA this week.
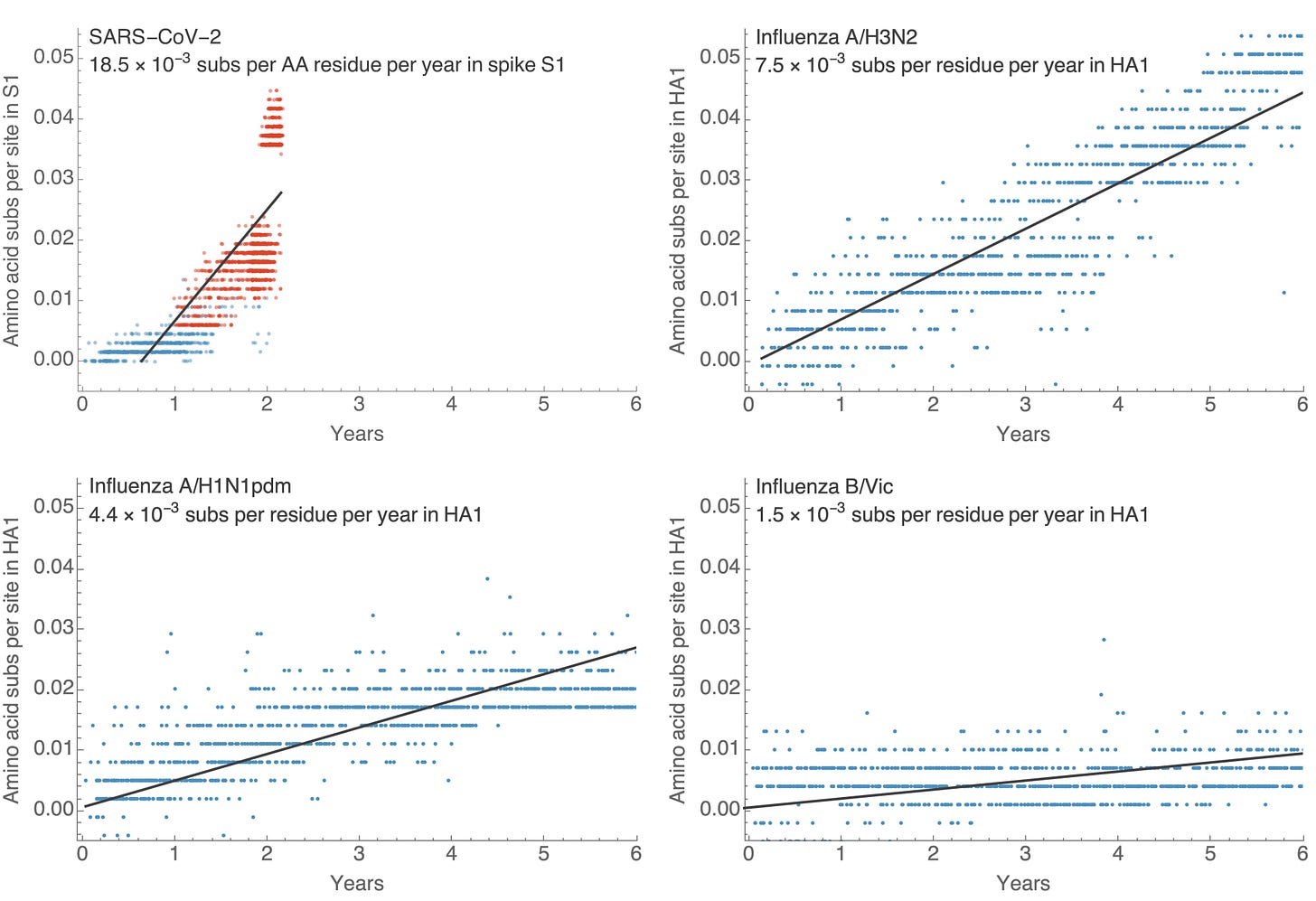
First, he made it clear that the virus is mutating incredibly quickly. It’s changing about four times faster than the flu. In his figure below, you can see the SARS-CoV-2 graph is far more steep than the other three graphs depicting the rate of influenza mutations. This means that in just two years, SARS-CoV-2 has accomplished the same level of evolution compared to five years of H3N2 (flu virus). We hope that once we finally get transmission under control, the rate will eventually be slower than the flu.
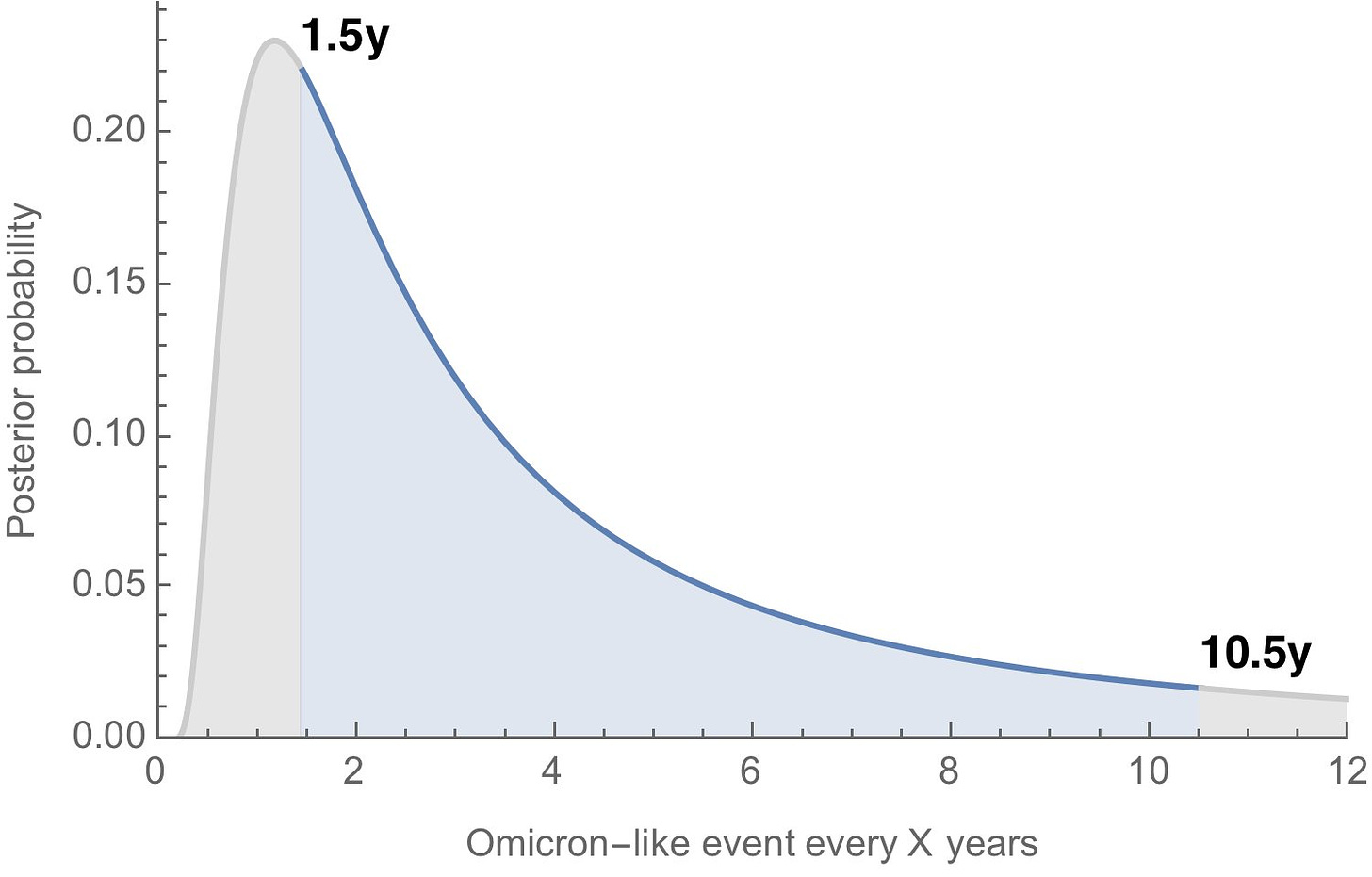
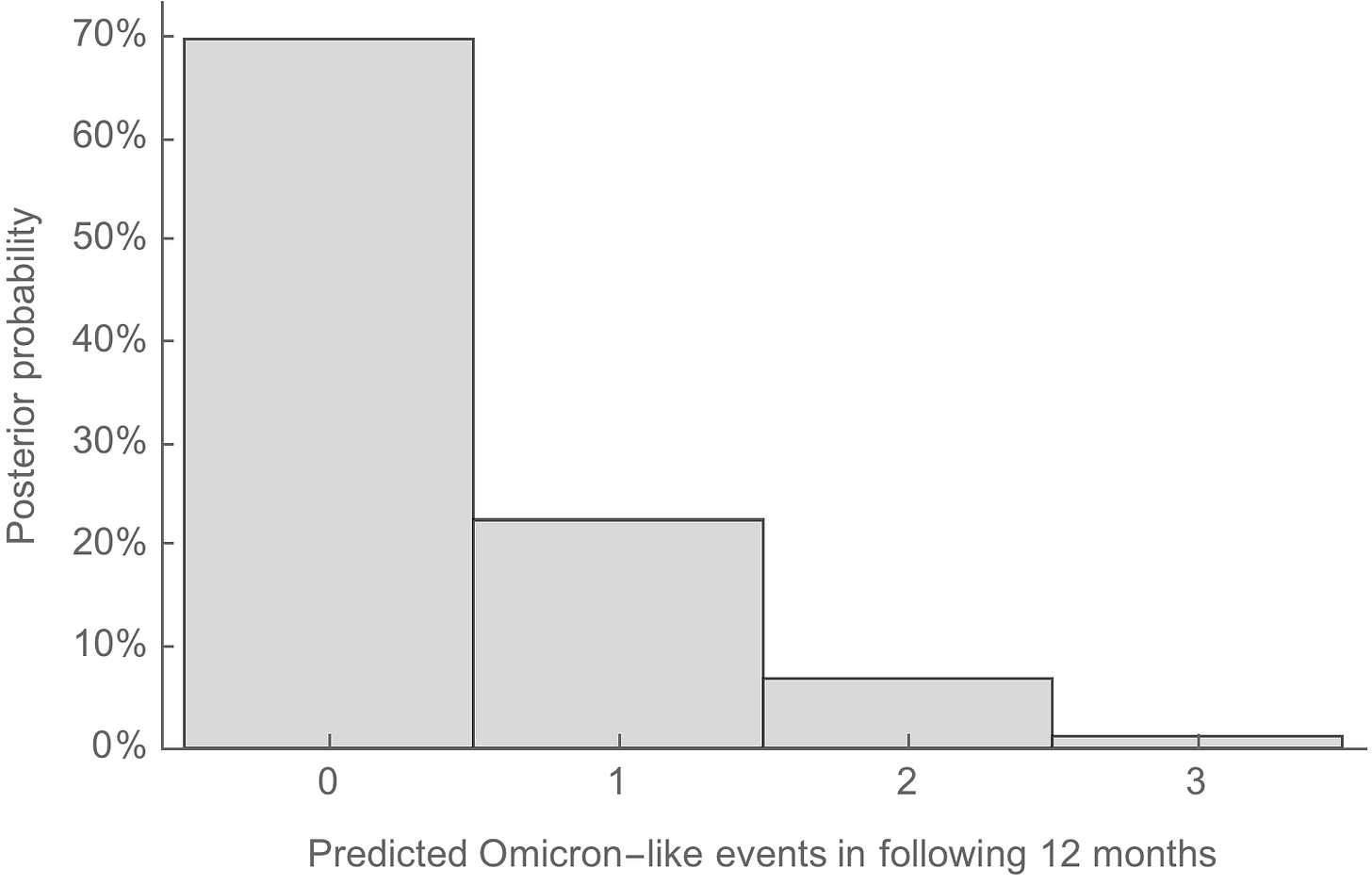
Second, while we expect with high certainty a “flu-like drift” of SARS-CoV-2, an “Omicron-like event” or a huge evolutionary jump can take place again, too. Unfortunately (or fortunately) we only have one data point over two years (i.e. Omicron), so our guesstimates have a high level of uncertainty. Dr. Bedford estimated that an “Omicron-like” event will happen every 1.5 to 10.5 years. We don’t know if this is a rare occurrence or a more common event. But, in the next year, Dr. Bedford estimates there’s a 70% chance we will not have another Omicron-like event.
For the next “Omicron-like event,” according to Dr. John Beigal at the NIH, there are really only two antigenic spaces or areas of vulnerability this could happen: a virus that is closer to Beta, or a virus that is closer to Delta. Both very far from Omicron, which perhaps makes an Omicron-specific booster not a slam dunk decision.
Bottom line
We know that the virus is going to combine and mutate. XE is just another example. If Omicron continues to mutate, it may be a silver lining, because then we may finally be able to better predict where this virus is going and how to proactively prepare for it. In the meantime, we need to try and keep transmission down as best as possible so this virus doesn’t have the opportunity for another “Omicron-like event.”
Have a great weekend,
YLE
“Your Local Epidemiologist (YLE)” is written by Dr. Katelyn Jetelina, MPH PhD—an epidemiologist, biostatistician, professor, researcher, wife, and mom of two little girls. During the day she has a research lab and teaches graduate-level courses, but at night she writes this newsletter. Her main goal is to “translate” the ever-evolving public health science so that people will be well equipped to make evidence-based decisions. This newsletter is free thanks to the generous support of fellow YLE community members. To support the effort, please subscribe here:


Katelyn, you really are more than a local epidemiologist. An "LE" wouldn't "call" with periodic valuable updates! Thank you.
Suggestion for a future post:
An update on your views of Long Covid.
What is the reasoning behind "we expect with high certainty a “flu-like drift” of SARS-CoV-2" ? It seems like everything you said (and I've read elsewhere) is that viral evolution hasn't fit any known models or patterns. Omicrons BA.1 and BA.2 are as different from each other as Alpha, Beta, Gamma, and Delta are from one another, so that isn't ladder like change yet. Is there something about a lot of recombinants that supports“flu-like drift” I'm missing?