As Omicron subvariants sweep the globe, the international death toll started rising for the first time in seven months. Although deaths still remain low, a 39% increase in death toll is noticeable. This increase is mainly driven by Southeast Asia (+20%), followed by the Eastern Mediterranean (+15%) and Americas (+7%).
Hospitalizations have doubled in Europe and no peaks have been seen yet for countries like France, U.K., Greece, or Italy, although hospitalizations do look to be slowing down. Notably, Australia has surpassed their previous Omicron peak for hospitalizations, and many systems are reaching capacity. Japan hospitalizations are also on the rise, which is not a surprise given that they just reported 152,538 new coronavirus cases—the biggest one-day increase on record.
United States
BA.5 was slower to claim dominance in the U.S., but now accounts for 78% of cases. And, like clockwork, once it claimed dominance, wastewater trends went upwards in all regions of the U.S. Interestingly, this uptick may be short lived as wastewater recently slowed and even reversed in some places. Case trends continue to give all sorts of weird signals, but test positivity rates seem to have peaked, too. This could be the top of the wave, which would be a surprising but welcome reprieve.

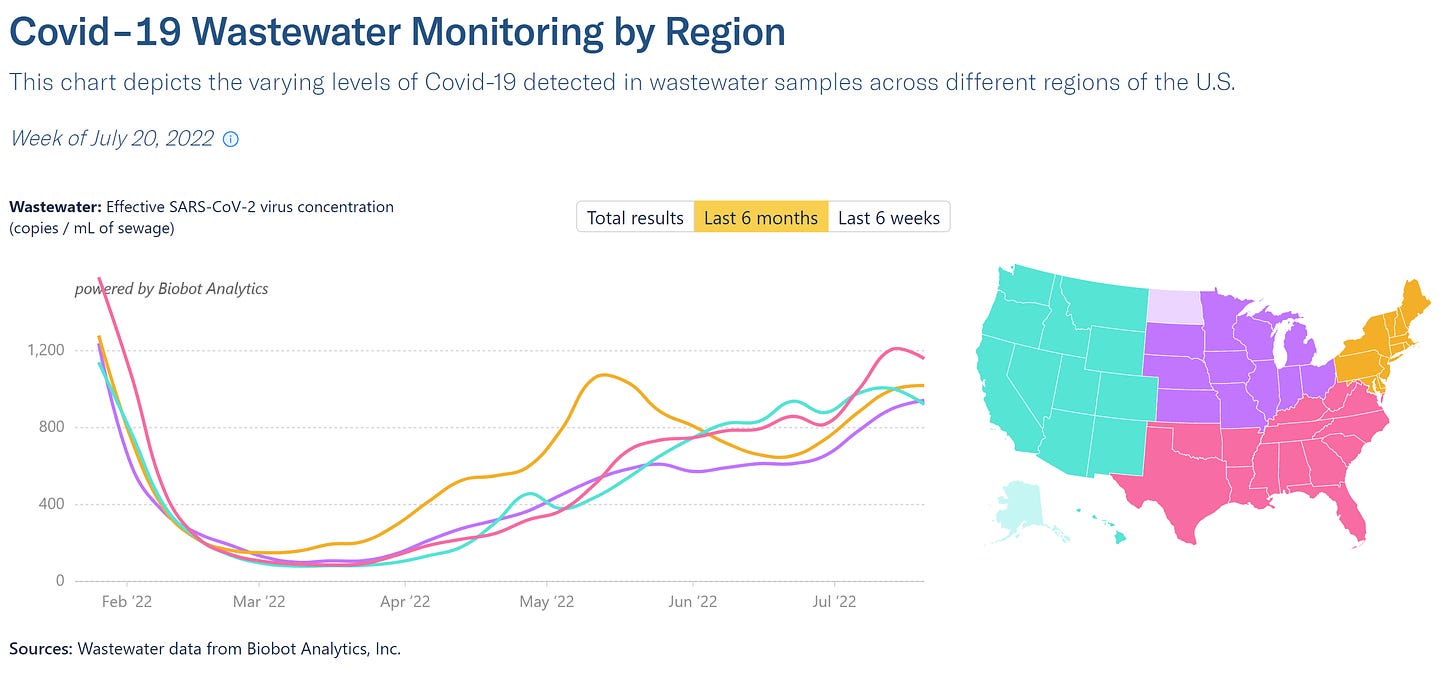
My eyes have been specifically on the pink line above—the South. With the combination of low booster rates, a heatwave (i.e. people headed inside), little BA.2.12.2 wave, low Paxlovid uptake, and little-to-no testing, severe disease may sneak up, just like we saw with Delta last summer.
On a national level, hospitalization trends continue to steadily increase. And this will continue as hospitalizations lag case trends. More than 43,000 people are in hospitals with COVID-19 on an average day. Notably, many of the acceleration leaders for hospitalizations are in the South: Arkansas, Louisiana, West Virginia, Kentucky, and Georgia.
Although hospitalizations are increasing, we are clearly in a different phase of the pandemic in regards to severe disease:
Case hospitalization rate continues to decrease over time, especially given dramatic underreporting.
ICU admissions—one proxy of severe COVID-19—remains relatively steady, regardless of an increase in hospitalizations overall and a highly transmissible virus sweeping the community.
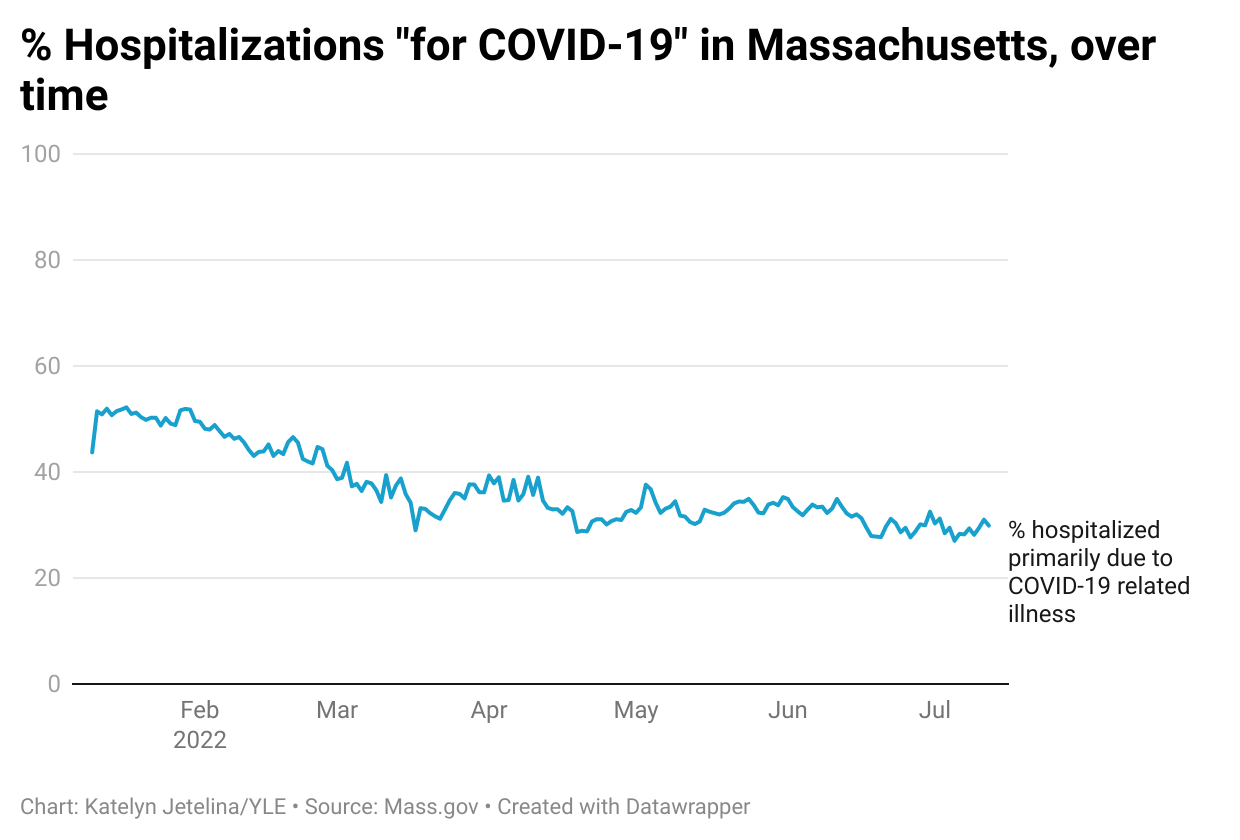
“For” COVID-19: We do not have a great picture of hospitalizations “with” vs. “for” COVID-19, but some jurisdictions, like Massachusetts, have been tracking this since January 2022. Today, of all COVID-related hospitalizations, about 30% are “for” COVID, and the percentage has steadily declined since January 2022 (when they started tracking this).
It’s important to note that this doesn’t mean the 70% “with” COVID-19 hospitalizations are irrelevant to the pandemic. COVID-19 could be complicating health issues, causing people to be in the hospital. Also, people bring COVID-19 to the hospital; hospital-acquired COVID continues to be steady.
Vaccination status. The vast majority of people in hospitals are older and unvaccinated or not up-to-date with their vaccines. Below are the current hospitalization rates in Los Angeles county.
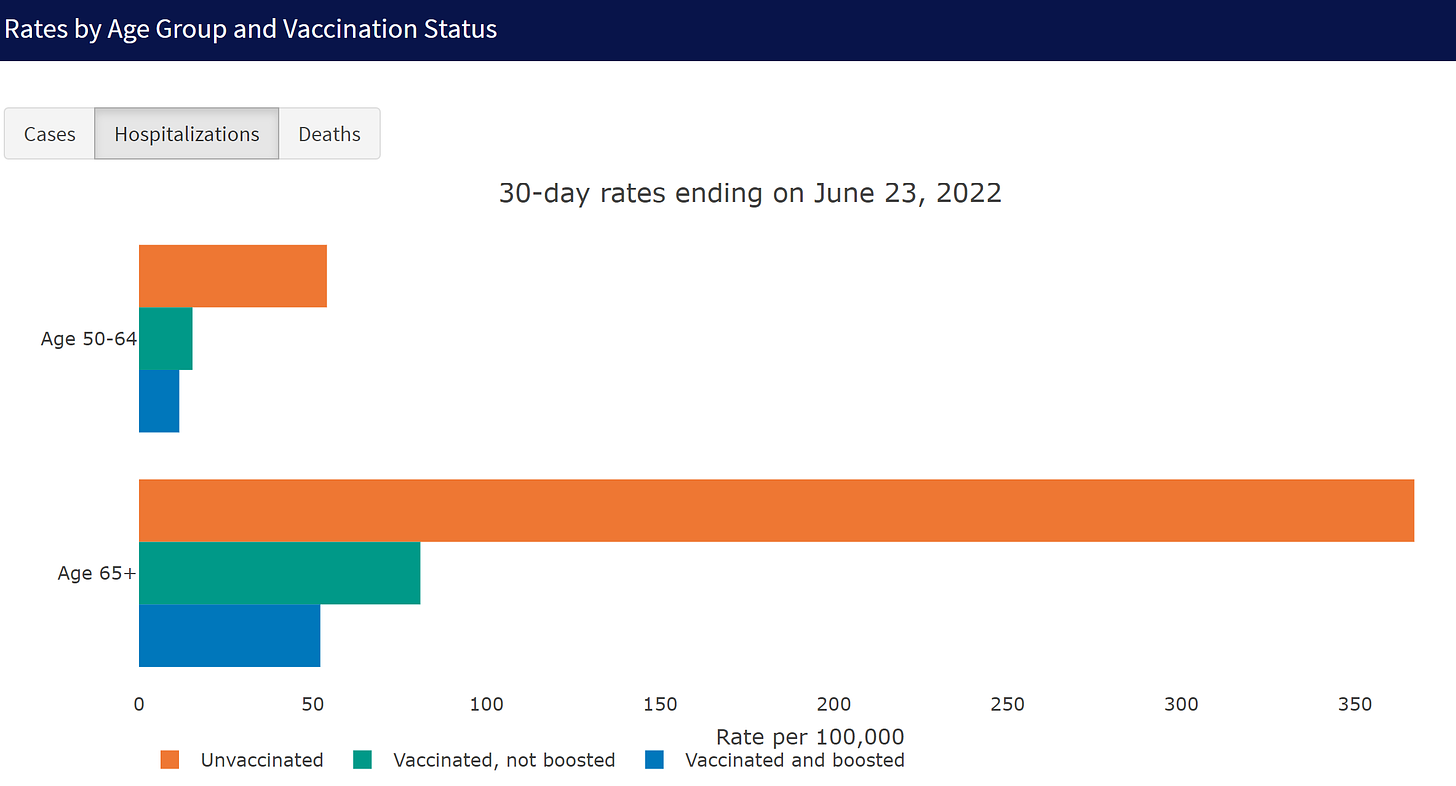
(County of Los Angeles Public Health; Source Here)
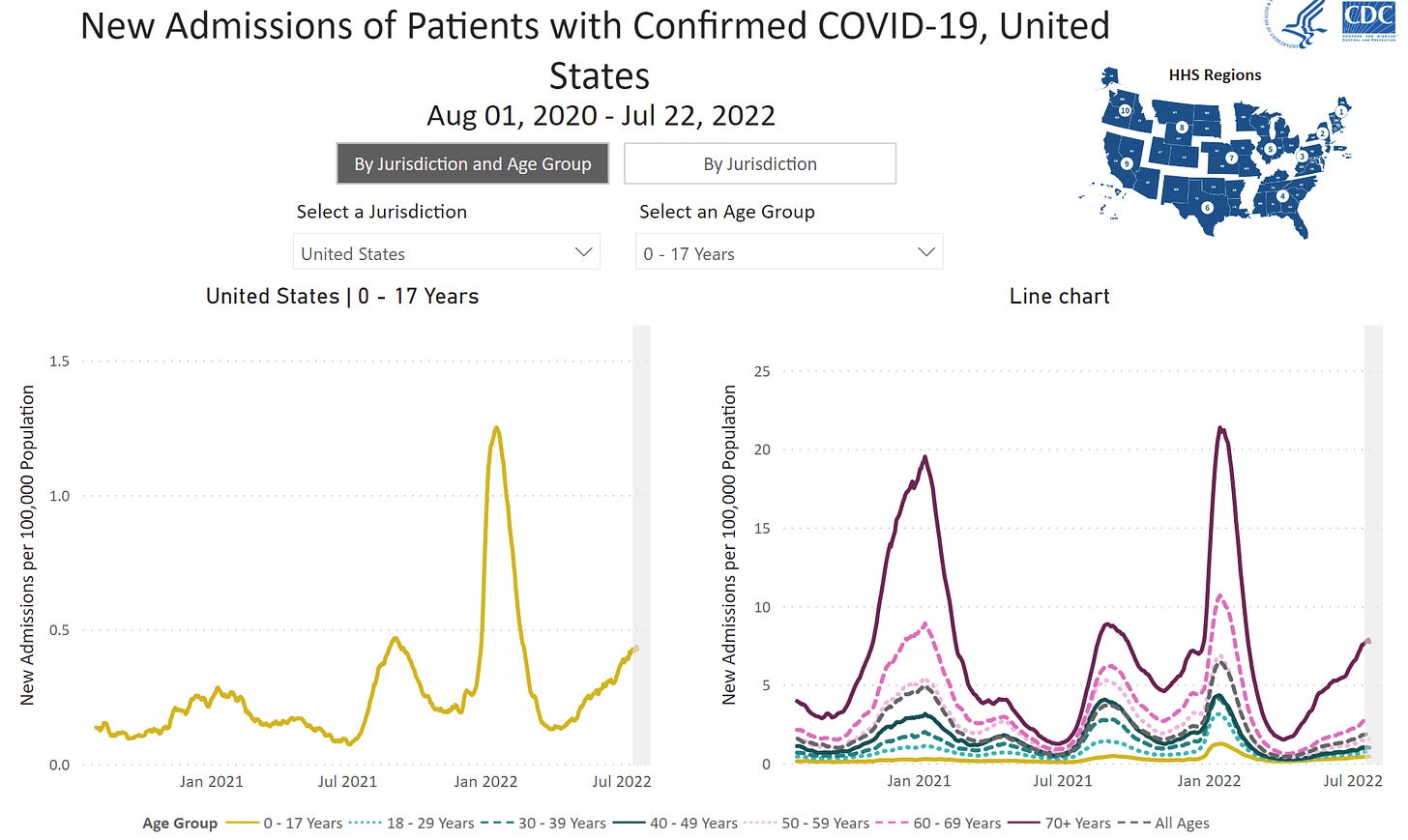
The national picture mirrors that of LA: The rise in hospitalizations is driven by 70+ year olds (see figure below). The hospitalization gap between this group and other age categories continues to widen, too. Unfortunately, even some fully vaccinated groups remain at risk for hospitalization. These groups will continue to remain at high risk until transmission calms down.
On the other side of the spectrum, pediatric hospitalizations remain relatively low compared to adults. But their hospitalization rate just passed the Delta peak, while other age groups are still far below it. This is likely explained by low vaccination rates among children.
Unfortunately, more than 400 people are still dying each day from COVID-19. After a few weeks of reprieve, excess death started to creep up again as BA.2.12.2 took hold in mid-May. Excess mortality data is delayed, so it will be important to continue to track this. With a new virus in our repertoire, an “acceptable” level of death is still a national conversation we need to have.
Bottom line
We are in the middle of a wave, and the world is feeling it. There are signs that BA.5 cases peaked in the U.S., but we need to ensure this trend solidifies. The story of severe COVID-19 continues to change for the better. If you don’t want to get sick or want to protect the vulnerable around you even if they are vaccinated, like grandparents, you need to continue to ride this wave responsibly.
Love, YLE
In case you missed it:
“Your Local Epidemiologist (YLE)” is written by Dr. Katelyn Jetelina, MPH PhD—an epidemiologist, biostatistician, wife, and mom of two little girls. During the day she works at a nonpartisan health policy think tank, and at night she writes this newsletter. Her main goal is to “translate” the ever-evolving public health science so that people will be well equipped to make evidence-based decisions. This newsletter is free thanks to the generous support of fellow YLE community members. To support the effort, please subscribe here:








I 'm really disappointed and worried about the number of experts being given media attention as they put their focus at how well we are doing against the virus, rather than focusing on the damage still being done and what can be done to combat it. Over 400 deaths a day is 150 thousand deaths a year - about 5 times the number of flu deaths in an average year. Where is the government money and will to keep fighting this disaster. Where is the financial support for new vaccines, including possible "universal" vaccines and nasal vaccines, and more anti-viral treatments? The effort to deal with Covid has gone from "warp speed" to a crawl. Where is the money and why have the CDC and FDA been allowed to return to the glacial speed which characterized their former review processes? The "new normal" is to sound the praises of our "successes" and encourage complacency. I am sorry to say that your article - as honest and informed as your writing always is - will be utilized as another expert opinion to add to the current analysis of the virus as mostly conquered and now something we'll just have to learn to live with. That is probably not your opinion but it will be read that way. Please emphasize how much more can and should be done, not just relying on individuals to protect themselves from a society which has apparently abandoned a sense of social responsiblity.
I apologize if this comment seems too strident and critical. I do appreciate your work very much which is why I am so upset at reading another article that seems to lend strength to those who want to "put it behind us".
Is there a decreased risk of severe disease at the individual level? This is something I have struggled to understand. I know many people have had COVID and/or had vaccines, which reduces their individual risk. But if you are a person who has not had COVID and is immunocompromised and high risk, is the disease really any less severe than it was 2.5 years ago? With precautions completely gone and transmission very high (at least where I live), it's hard not to feel like there is no hope for these people.