
Today the FDA granted full approval to Pfizer/BioNTech’s COVID19 vaccine for people 16 and older. The FDA press release highlighted the rigor this entails:
“The public can be very confident that this vaccine meets the high standards for safety, effectiveness, and manufacturing quality the FDA requires of an approved product.”
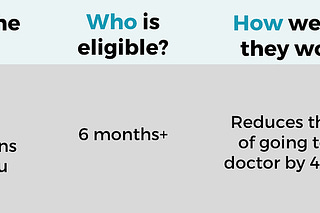
The vaccine also continues to be available under emergency use authorization (EUA) for 12-15 year olds and for the third dose among immunocompromised individuals.
This only confirms what we’ve known for months: the vaccine is safe and effective.
Nonetheless, this. is. worth. celebrating.
This is the first mRNA vaccine to be fully approved. And it’s been a long scientific road to get here. The work began in 1961, when mRNA was first identified as an integral part of our human body.
Then, in the 1990’s, Dr. Katalin Karikó, a Hungarian-born scientist, discovered that mRNA could possibly be used for vaccines. For decades she had convince people to fund her research, which was more than difficult. But her perseverance, leadership, and collaborative spirit prevailed and research resulted in the COVID19 Pfizer/BioNTech vaccine we are using today. (Read more about this story here; it’s fascinating. I hope she’s celebrating with a glass or five of wine).
Before the pandemic, there were (and currently are) many clinical trials testing the applicability of new class of treatments for cystic fibrosis, heart disease, genetic conditions, cancers, diabetes, the flu, and even seasonal allergies. It’s not an understatement to say that mRNA biotechnology will be a game changer for the human race.

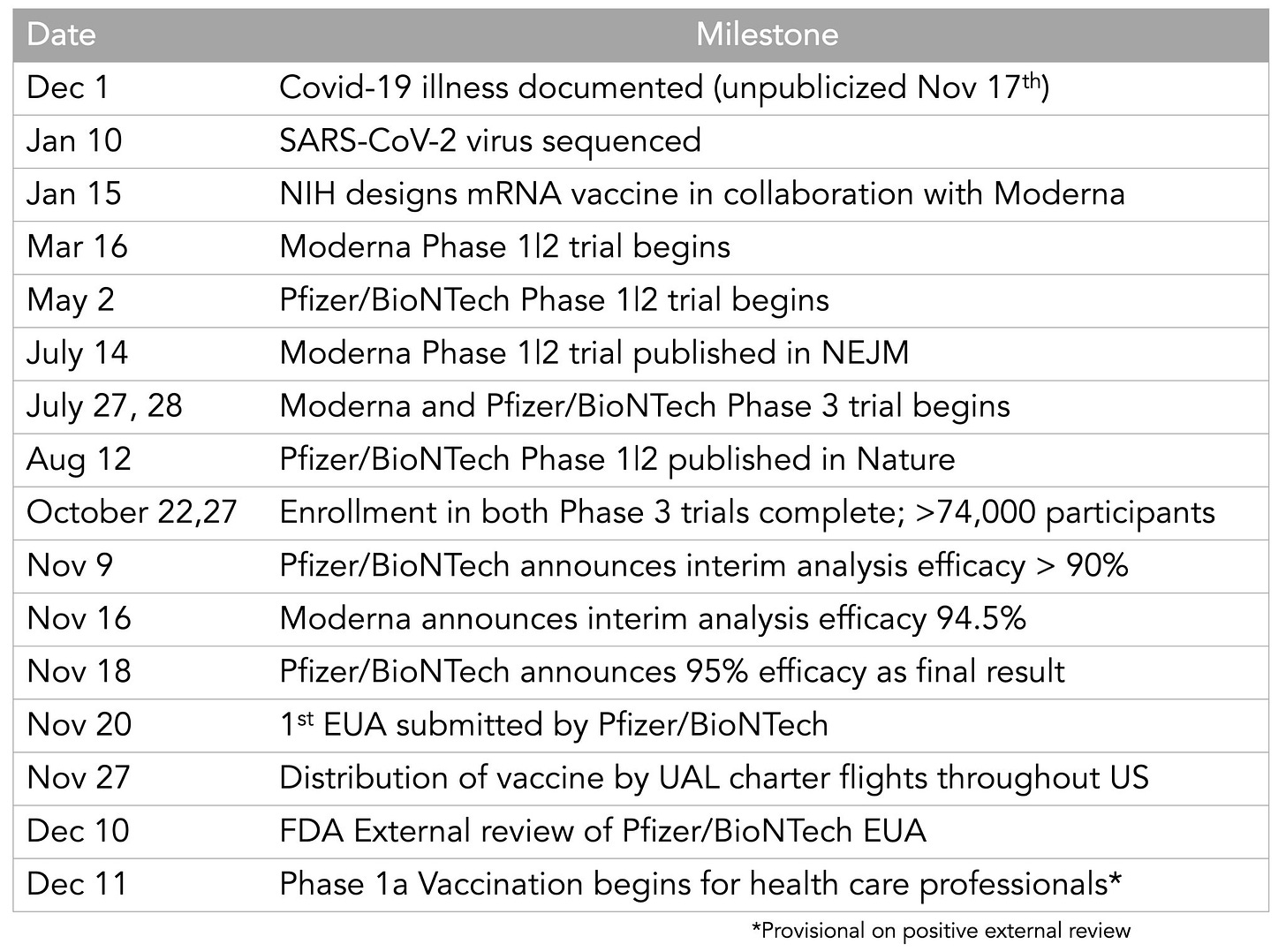
Once the pandemic hit, scientists quickly leveraged this groundwork and adapted it for a COVID-19 vaccine. Speed did not mean rushed. It meant leveraging a whole lot of smart people (scientists and clinical trial volunteers), money, and decades of previous work to get us a vaccine. And we did it in 9 months.
Pfizer was granted Emergency Use Authorization (EUA) by the FDA in December 2020 after accumulating the required 2 months of Phase III data. It was under the assumption that they would apply for a full licensure once they had 6 months of follow-up data (showing vaccine longevity, continued safety) and necessary documents (like manufacturing processes).
On May 7, 2021 Pfizer submitted their application for full approval. Today, the FDA fully approved the vaccine for those aged 16+ years old.
So, what does full approval change?
We should see a cascade of events.
First, we should expect an uptick in vaccinations. According to the Kaiser Family Foundation, 3 out of 10 (32%) unvaccinated adults said they were more likely to get the vaccine if the FDA granted full approval. After crunching the numbers (209,128,094 18+ year olds in the United States and 70.8% vaccinated), we should see 6.2 million adults in line to get a vaccine.
Second, clinicians now have the autonomy to prescribe off-label. Clinicians now have the decision-making power to recommend the vaccine to children aged 11 and younger. I’m sure pediatricians were inundated with phone calls today. Thankfully the American Academy of Pediatrics was quick to react and released a statement today discouraging this practice:
“The clinical trials for the COVID-19 vaccine in children ages 11 years old and younger are underway, and we need to see the data from those studies before we give this vaccine to younger children. The dose may be different for younger ages. The AAP recommends against giving the vaccine to children under 12 until authorized by the FDA”.
Third, the private and public sectors will likely ditch the carrot approach. The stick will probably be coming. A full approval means that employers, insurance companies, businesses, and maybe even hospitals may start getting braver with requirements:
Many employers were hesitant to require vaccination under EUA. The legality of was in bit of uncharted waters. In June 2021, the Equal Employment Opportunity Commission issued guidance stating that employers can mandate COVID-19 vaccinations for employees who physically enter the workplace without running in anti-discrimination laws. But they also said “it’s beyond the EEOC's jurisdiction to discuss the legal implications of EUA or the FDA approach” and employers needed to consider religious and disability-related objections and explore reasonable accommodations. Employers did succeed in vaccine mandates under EUA, though. Houston Methodist hospital was one of the first in the nation to mandate COVID19 vaccines for their employees. This prompted 117 employees (out of 26,000) to file a lawsuit. But, a federal judge said the employees' claim was “false” and “irrelevant” and that it “will make it safer for their workers and the patients in Methodist's care.”
Health insurers may start thinking about higher premiums for unvaccinated people. In June and July 2021, there were 113,000 preventable COVID-19 hospitalizations among the unvaccinated. In two months, this cost the US healthcare system $2.3 billion. That’s not a small bill.
Full FDA approval will surely bring an interesting debate among other businesses too:
Businesses may start requiring proof of vaccination for customers. San Francisco is already requiring proof of vaccination to enter bars.
What about triage-making decisions? This debate came to the limelight last week when Dallas clinicians were discussing a tough scenario: If there is only one ICU bed left, does it belong to the person in a car accident? Or does it belong to the unvaccinated person who needs to be intubated because they didn’t take an effective and safe preventative measure? I doubt it will ever come to this, but an interesting debate to bring back to the classroom.
Bottom Line: The first full approval of mRNA biotechnology is a game changer. Both for scientific discovery and for getting us one step closer to ending this pandemic.
Cheers, YLE










Does this mean providers may purchase doses independently of the federal vaccination program? If yes, does this mean consumers can now have to be careful to make sure their vaccine is being provided through the program to avoid a copay if insured or paying full price if not? If no - if all vaccine still goes through the program - is off-label legal? If a provider goes through the program, they have to follow the program rules or they are "stealing" the vaccine.
I'm in Wake County in North Carolina, and we're a little confused about how Delta would change public health measures for schools.
Our school district takes their advice from the NIH-funded ABC Science Collaborative, which published a recommended plan for school districts on June 30, 2021 (https://abcsciencecollaborative.org/wp-content/uploads/2021/06/ABC_year-in-review_29jun2021-final.pdf). Overall the report seemed to adhere to last year's best practices and research findings, and not take into account the increased infectiousness of Delta. Specifically, they don't recommend any SARS-CoV-2 screening testing because, "No existing data support the need for screening testing to ensure safe, in-person education when masking is in place" (Page 11).
However, I've noticed a some of the more progressive school districts implementing mandatory testing of students and staff (LAUSD), as well as researchers recommending it in addition to masking (https://covsim.hosted-wordpress.oit.ncsu.edu/files/2021/08/covsim-covid-19-school-policies-part-02.pdf).
It was also my understanding that regular SARS-CoV-2 Screening is recommended by the CDC and NC DHHS (e.g, https://covid19.ncdhhs.gov/media/2242/open) during times of high community transmission (which, I would think would be now).
My understanding is that the original authors of the report (chairs are Zimmerman and Benjamin) believe that masks are equally as effective regardless of the strain. And that testing is unnecessary in schools even when community transmission is high.
Have you covered this difference in recommendations -- specifically screening testing in schools vs. not screening? Thank you!