The ACIP meeting for spring boosters convened yesterday. You know the drill; here are your Cliff notes.
Bottom line upfront
CDC and FDA are trying to simplify COVID-19 vaccine recommendations. (Verdict is out if they actually did this for kids). From now on, people are “up-to-date” if:
6+ years old: 1 bivalent (i.e. fall Omicron vaccine) dose. Regardless of vaccine history. Period.
<6 years old:
Moderna: at least 2 doses, including 1 bivalent.
Pfizer:
5 years: 1 bivalent.
Under 5 years: at least 3 doses, including 1 bivalent.
If you meet this criteria, there is nothing you need to do right now. You can stop reading.
But this happens to be only 1 in 6 Americans (2 in 5 of those who 65 years and older). A ridiculous number of Americans are not up-to-date with COVID-19 vaccines. This means a lot of people need to keep reading.
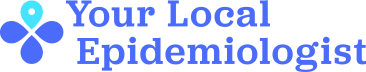
Also, adults 65+ years and/or immunocompromised who got the fall booster may now choose to receive a spring booster (the timing varies, see figure below). This YLE post is for you.
Bivalent safety
Safety data was presented at the ACIP meeting in detail. There were no surprises; it continues to look great.
There are two questions the CDC is trying to get clarity on, though, for those over 65:
3-6 weeks after the fall booster, the rate of strokes was lower among vaccinated than unvaccinated. In other words, there may be a secondary protective effect, which is great news.
Getting the flu and COVID-19 vaccines simultaneously may be a problem. While not statistically significant, there is an elevated rate of stroke within 21 days. (It’s pretty darn close to being statistically significant, too.) I hope we get more clarity before the upcoming fall vaccine campaign.
Bivalent effectiveness
Why do I need a spring booster? CDC presented data that shows vaccine effectiveness waning against hospitalization. Efficacy for bivalent vaccines among those over 65 years decreased from 64% to 39%.
While 39% seems low, there are two important points to keep in mind:
We need to think of effectiveness as “relative” now—relative to some combination of prior vaccination, prior infection, or both. This means the 39% is the benefit above and beyond whatever underlying immunity an individual has. We’re going to see lower numbers than we were used to because of this, but it doesn’t mean we’re not getting protection (i.e., hospitals are not filling up).
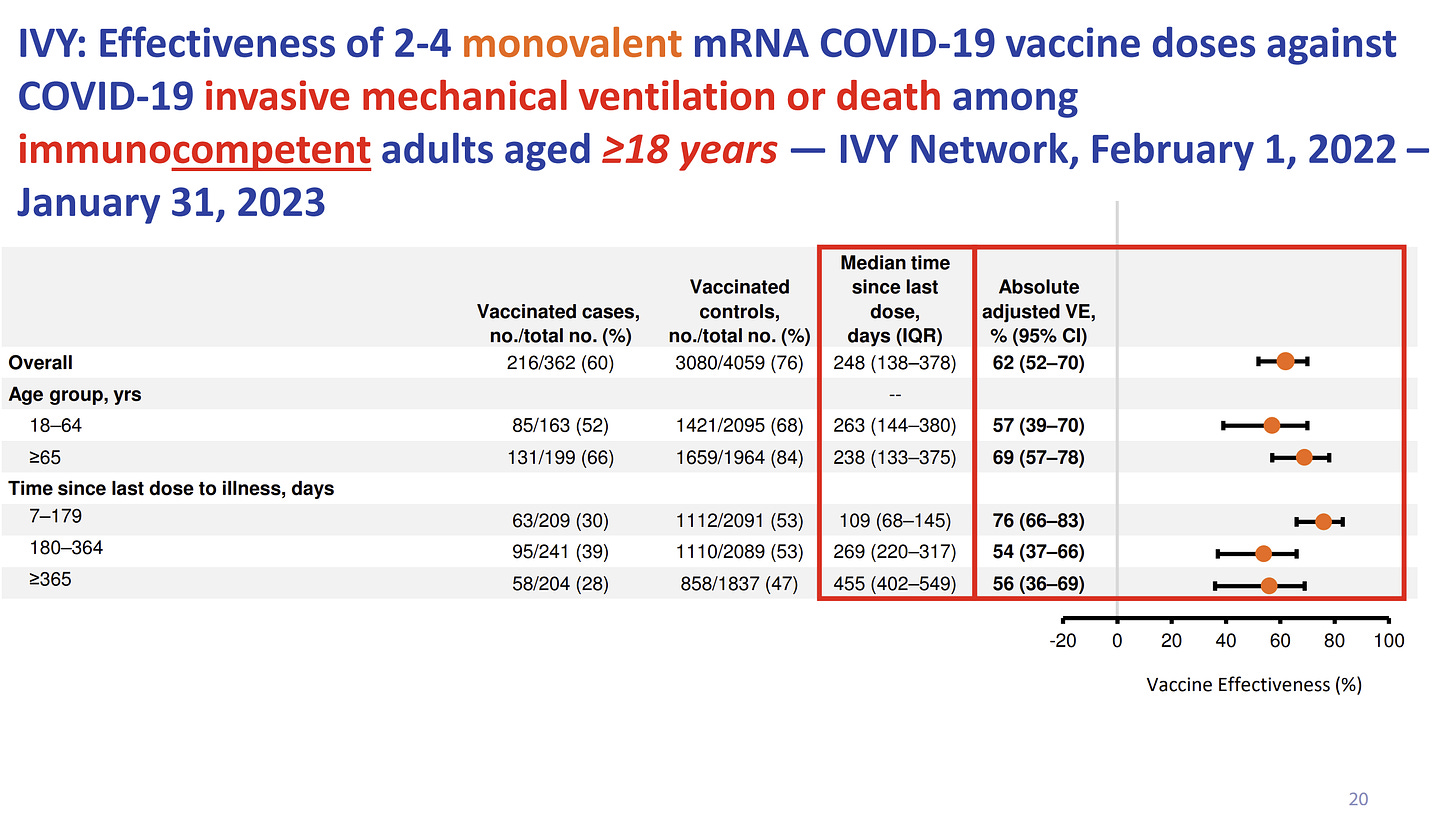
We are getting more hospitalized “with” COVID-19 (vs. “for”) than before, making it harder to understand what it means when someone is hospitalized and has a COVID-19 diagnosis. One way to know if hospitalization is “for” COVID-19 is to look at ventilator use. Protection against ventilator use has not waned.
So the majority of people are still protected against severe disease from COVID-19. However, among older people with comorbidities, risk for hospitalization “with” COVID-19 likely increases with time. (I go through the why and how in more depth on this YLE post.) We don’t know what this risk is prospectively, but getting a spring booster is one way to avoid finding out.
Lingering ACIP questions with some answers
What about people who didn’t get the mRNA vaccine? If someone doesn’t want the mRNA booster or is allergic to some component, there is no option for them at this time. Novavax said they should have a bivalent vaccine by fall.
What about immunocompromised kids under 5 years old? They are not eligible for a spring booster. FDA said that it’s because they just don’t have data to justify it. Pediatricians in the meeting were not happy with this answer and rightfully so. These vulnerable children are being left behind.
What about pregnancy? Pregnant people are not eligible for a spring booster. There’s a good chance this will change in the future. A CDC decision should be made in the coming weeks.
What if I just had an infection? The CDC is still not providing recommendations based on infection history. (I was surprised.) Canada took this route, which I agreed with.
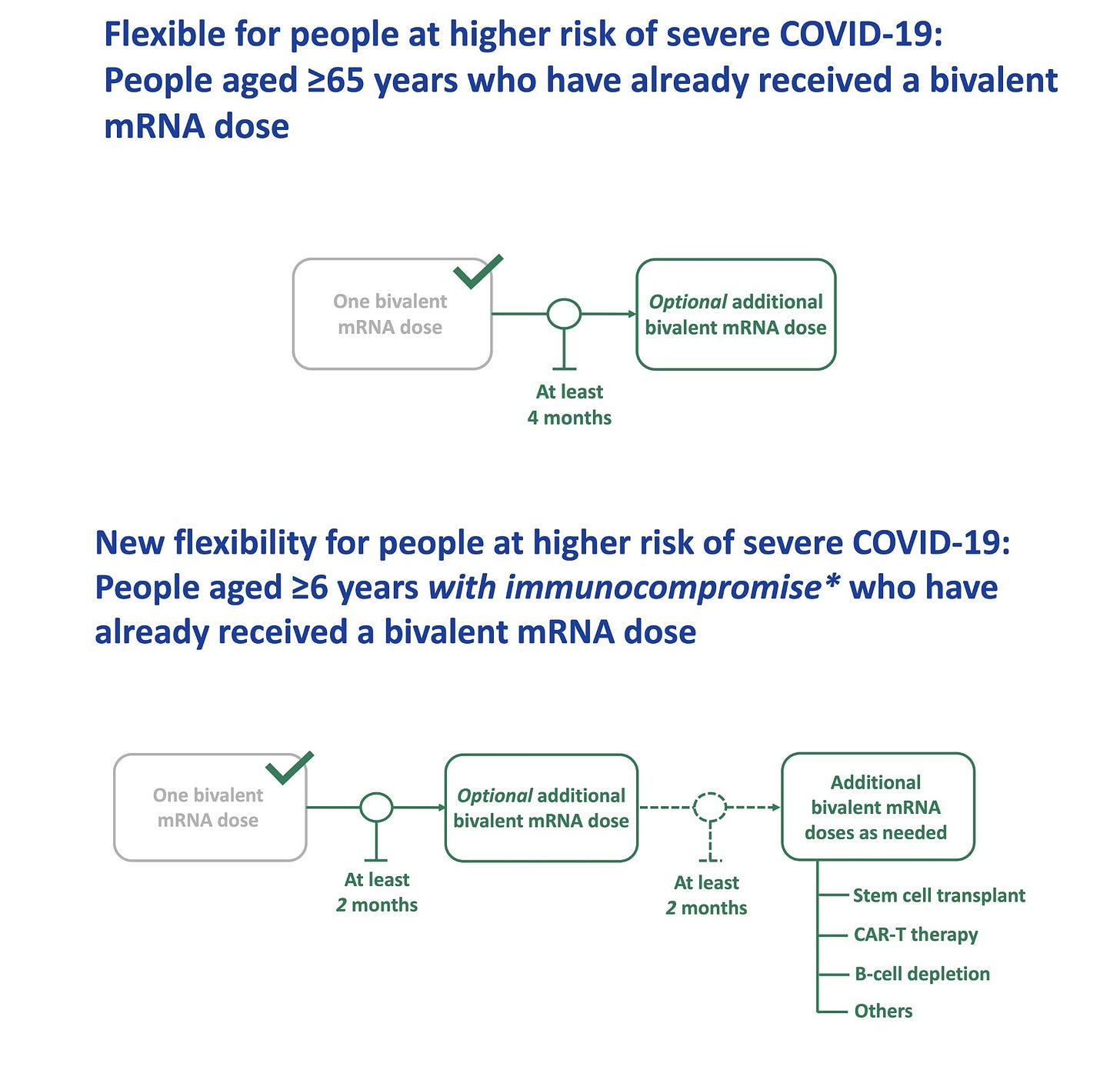
Are the recommendations for children really more simple? No. Parents are supposed to follow the figure below, which is confusing. We need to fix this.
What’s next?
The FDA meets in June to discuss the fall vaccine plan, including the vaccine variant formula. I expect everyone will be eligible for a booster in the fall, but time will tell.
Bottom line
Anyone who hasn’t had a bivalent vaccine (i.e. fall Omicron booster) needs to get one. A small group of Americans are now eligible for a spring booster. This is important given the continued unpredictability of COVID-19—prepare for the worst, and hope for the best.
Love, YLE
P.S. For what it’s worth, I strongly recommended spring boosters to my grandparents (in their 90s) and older adults in my life in with a comorbidity, especially if they haven’t had an infection in the past 6 months.
In case you missed it:
“Your Local Epidemiologist (YLE)” is written by Dr. Katelyn Jetelina, MPH PhD—an epidemiologist, data scientist, wife, and mom of two little girls. During the day she works at a nonpartisan health policy think tank and is a senior scientific consultant to a number of organizations, including the CDC. At night she writes this newsletter. Her main goal is to “translate” the ever-evolving public health science so that people will be well equipped to make evidence-based decisions. This newsletter is free thanks to the generous support of fellow YLE community members. To support this effort, subscribe below.





This is anecdotal, but I noticed after my first bivalent booster in October a significant reduction in my PASC (long Covid) symptoms. A very noticeable improvement. I know correlation doesn't imply causation and I don't understand the mechanism that would be involved if there was causation, but I am very eager to get a second bivalent. My age gives me eligibility!
I wish everyone's language, including yours, would refer to "severe acute disease" instead of "severe disease", to be more accurate. They haven't measured the impact of boosters on Long COVID, nor on what the general public would call severe Long COVID (significant sustained reduction in daily activities). When the public hears facts about severe disease, eg how much less of it there is, they falsely think that severe Long COVID is included. Actually, it has been excluded from the decision making process.