I received thousands of emails, messages, and comments after my last post, all asking, essentially, the same thing: Is there any hope? So, I interrupt my regular broadcast with a big, loud answer: YES.
After reading through these messages, I realized that while I and others actively respond to crises, we’ve neglected to communicate how far we’ve come. One of public health’s biggest challenges is that when it works, it’s largely invisible. This isn’t the case in other fields. For example, in medicine you can see the impact of a surgery. In the drug industry you can see the immediate effect of a prescription. In public health, we don’t see what we prevented. For example, how much do you really appreciate seatbelts on a daily basis? Seeing what public health prevents is nearly impossible for the untrained eye. So, this is what we aren’t seeing right now…
Vaccines are working
And not just working okay, they are working incredibly well. I know this is hard to believe when everyone around us is testing positive. But vaccines are doing their primary job: keeping people out of the hospital. We can easily see that in many graphs, but my favorite is below from New York City, showing a clear distinction in hospitalizations among vaccinated compared to unvaccinated people.

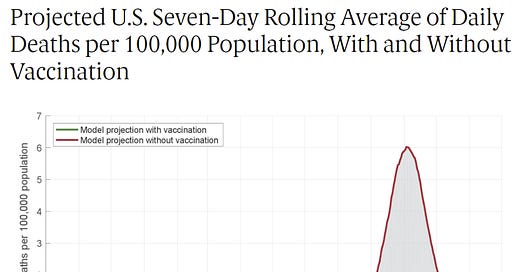
We can see this in totality too. The Commonwealth Fund recently published a brief in which they analyzed the extent to which the vaccine program in the United States averted deaths and hospitalizations since its rollout. Their main conclusion was as follows:
“In the absence of a vaccination program, there would have been approximately 1.1 million additional COVID-19 deaths and more than 10.3 million additional COVID-19 hospitalizations in the U.S. by November 2021.”
Below is their graph comparing projected deaths without a vaccination campaign to deaths with a vaccination campaign from October 2020 to November 2021. The number of lives saved is beautiful.
This is all pretty incredible given the vaccines were made against the original variant that popped up more than 2 years ago, and jumped from person to person across more than 250,000,000 people worldwide.
How did we do this? It’s because Americans got their vaccine in 9 months, which shattered all time records for development of previous vaccines. But speed didn’t mean it was rushed. It meant leveraging a whole lot of smart people, money, and decades of previous work to get us a vaccine in 9 months. (I talked about all of these things in a previous post here.) It also meant that more than 500,000 people volunteered to test the vaccine. They raised their hands to volunteer in clinical trials in which a new biotechnology was being tested that was never before authorized. They also had the chance of getting a placebo. Most of these people stayed in the trial, even after they could have had the placebo. People from 6 months old to the elderly participated. From all different backgrounds. And those neighbors of ours are a key reason we are saving so many lives right now. This couldn’t have been done without each and every one of them.
Omicron gave us some breaks, too
In addition to vaccines, we actually got very lucky with Omicron on many fronts. This includes:
More and more mounting evidence is showing that Omicron is less severe than previous variants. A recent preprint found the risks for ED visits, hospitalization, ICU admission, and mechanical ventilation were consistently LESS THAN HALF among Omicron infections compared to Delta infections. In children under 5 years old, the overall risks of ED visit and hospitalization for Omicron were 3.89% and 0.96% respectively, significantly lower than 21.01% and 2.65% in the matched Delta cohort. The running hypothesis (confirmed in 6 lab studies) is that this is the case because Omicron doesn’t infect the lungs as efficiently; rather, it infects the upper respiratory system much more.
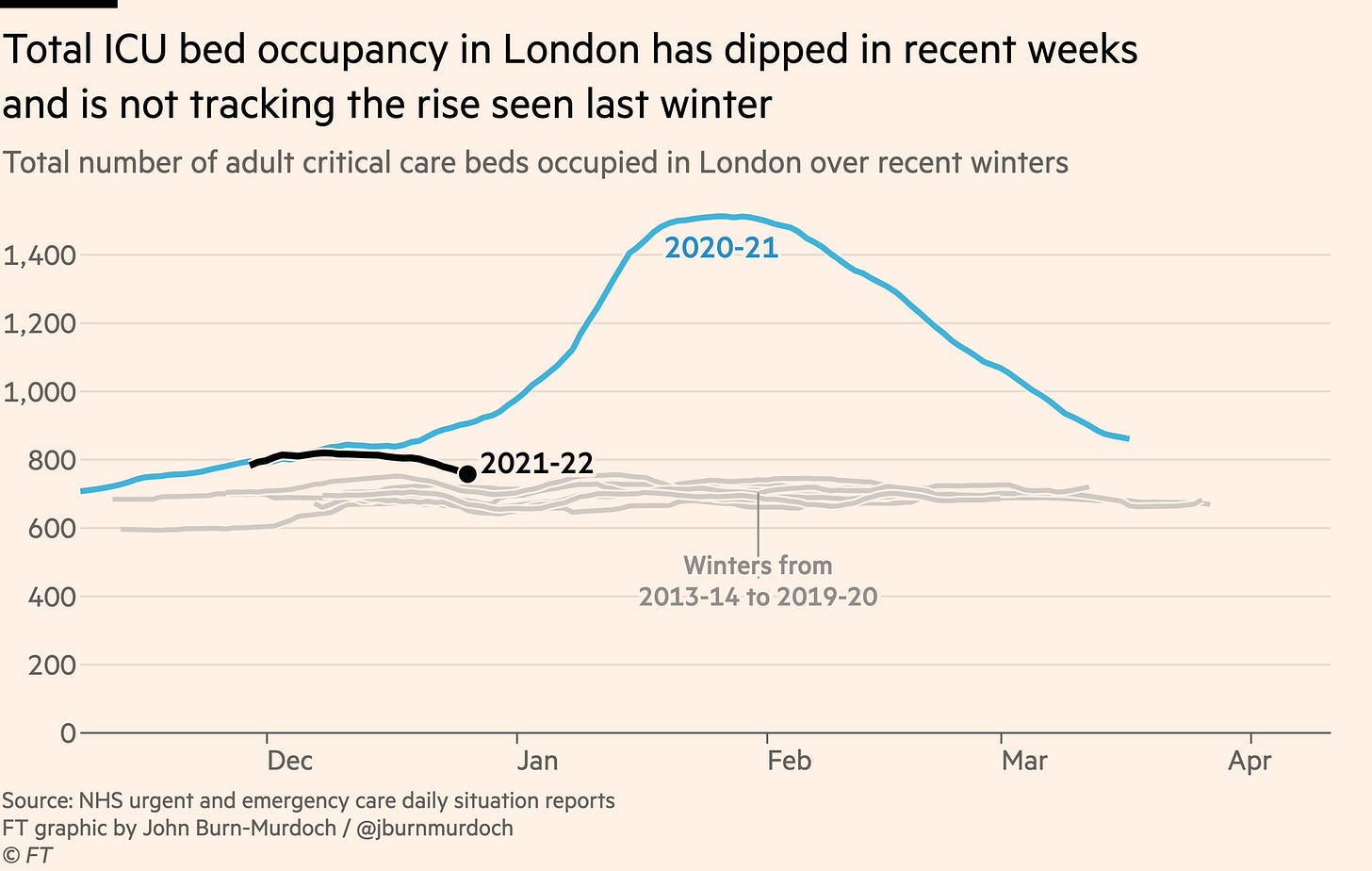
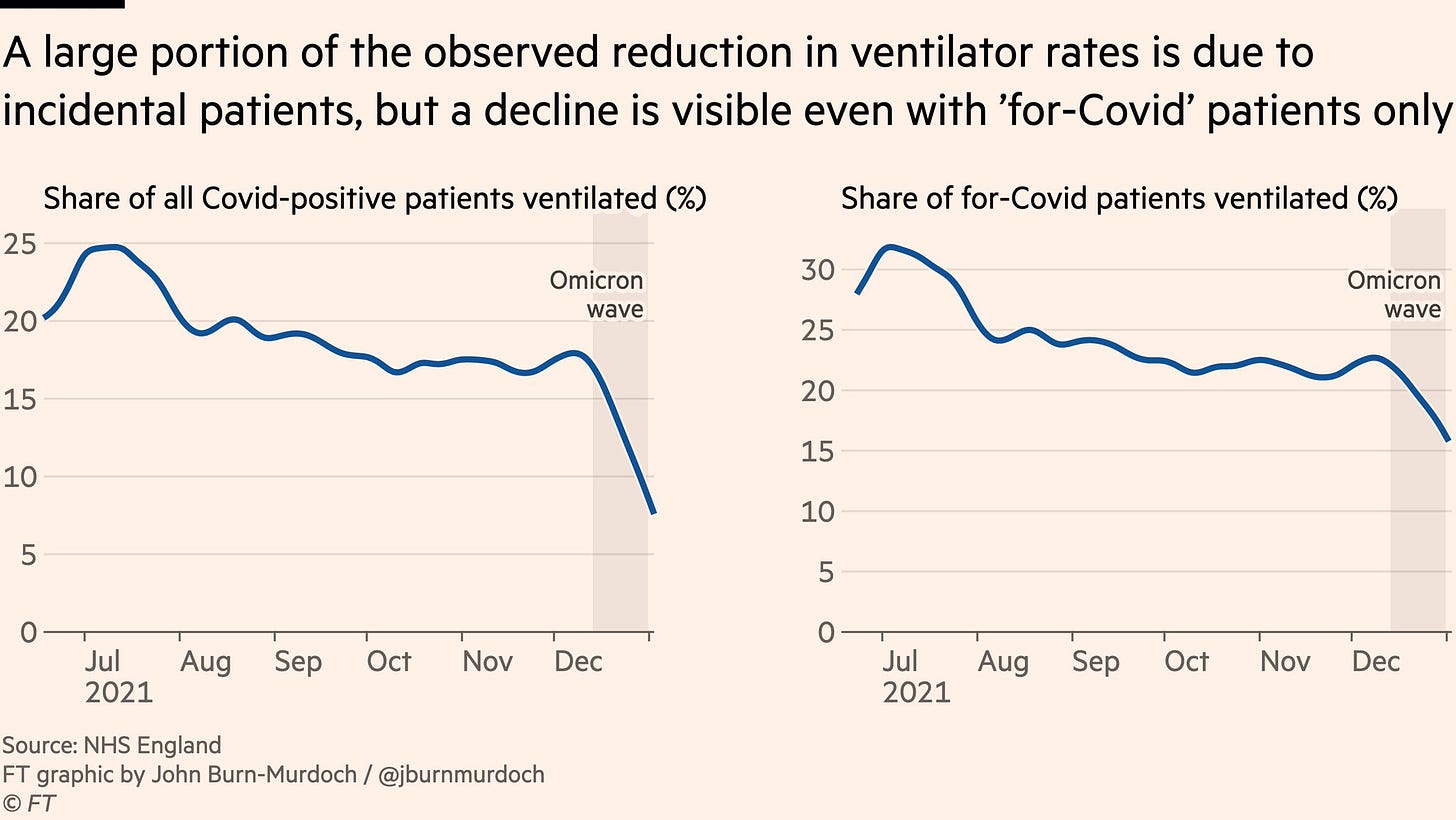
Omicron also didn’t fully escape our vaccines or immune systems. Our boosters are 50-88% efficacious against Omicron. And even if someone doesn’t get a booster (and they are not high risk) their T-cells kick in and still largely protect them from severe disease and death. Together with #1, this is leading to decoupling of hospitalizations from cases: hospitalizations are not rising at the same rate as cases. Because of this, in the UK, the number of ventilators being used is at the same rate as pre-pandemic winters. And decreasing.
Antigen tests can still detect Omicron really well. (I’m writing another post that’s coming out tomorrow about this).
We have a really effective antiviral that some high-risk individuals are getting right now, which will no doubt reduce their individual-level risk of hospitalization and death.
We now know that masks work great. They aren’t perfect, but a recent study that pooled more than 70 studies showed that masks reduce transmission by 57%. N95s are much better (close to 95% reduced transmission). And, unlike at the beginning of the pandemic, we have plenty of N95’s in supply. We also have KN95s for kids.
More help is coming
And although we have a issues right now with distribution and supply, help is on its way. The FDA just announced the authorization of two more antigen tests, which will result in millions and millions of tests coming next month. Also, at-home rapid tests will soon (finally) be reimbursed by insurance. Pfizer is ramping up production for antivirals and we will have enough for 300,000 Americans by the end of February and, eventually, 120 million courses in 2022. A dream coronavirus vaccine is in clinical trials that, if successful, will prevent severe disease from all future coronaviruses. And kids under 5 will get the vaccine by summer.
Bottom line: Public health is invisible when it works. Although we are in crisis mode right now, our tools are working and help is on the way. Every epi curve comes down. This one will too. Don’t take Omicron lightly, but don’t lose hope either.
Love, YLE
“Your Local Epidemiologist (YLE)” is written by Dr. Katelyn Jetelina, MPH PhD—an epidemiologist, biostatistician, professor, researcher, wife, and mom of two little girls. During the day she has a research lab and teaches graduate-level courses, but at night she writes this newsletter. Her main goal is to “translate” the ever-evolving public health science so that people will be well equipped to make evidence-based decisions, rather than decisions based in fear. This newsletter is free thanks to the generous support of fellow YLE community members. To support the effort, please subscribe here:





As my kids are back to distance learning and every other patient I see has COVID-19, I so needed this. Thank you for the reminder of how far we have come and for all that you do to keep us so well-informed. You have been a light in the darkness.
I will literally be printing this out and hanging it up at home and in the office to help manage my severe anxiety. I have an actual, diagnosed anxiety disorder and health-related OCD, so, needless to say, it's been exceptionally difficult for me to logically think through the realistic risk levels and try not to be constantly wracked with panic when I am really taking the highest level of precautions.